Axillary dissection plays an important role in the treatment of breast carcinoma. It is able to reduce the rate of local recurrence and allows accurate staging, but is also associated with adverse effects. With the increasing use of radiotherapy, surgical-technical advances, and a shift toward more restrictive indications, much has happened in recent years – and more changes are just around the corner.
Axillary dissection plays an important role in the treatment of breast carcinoma. It is able to reduce the rate of local recurrence and allows accurate staging, but is also associated with adverse effects. In particular, there is a significant risk of developing lymphedema or restricted shoulder motion. A careful risk-benefit assessment is therefore essential. With the increasing use of radiotherapy, surgical-technical advances, and a shift toward more restrictive indications, much has happened in recent years – and more changes are just around the corner.
A look back
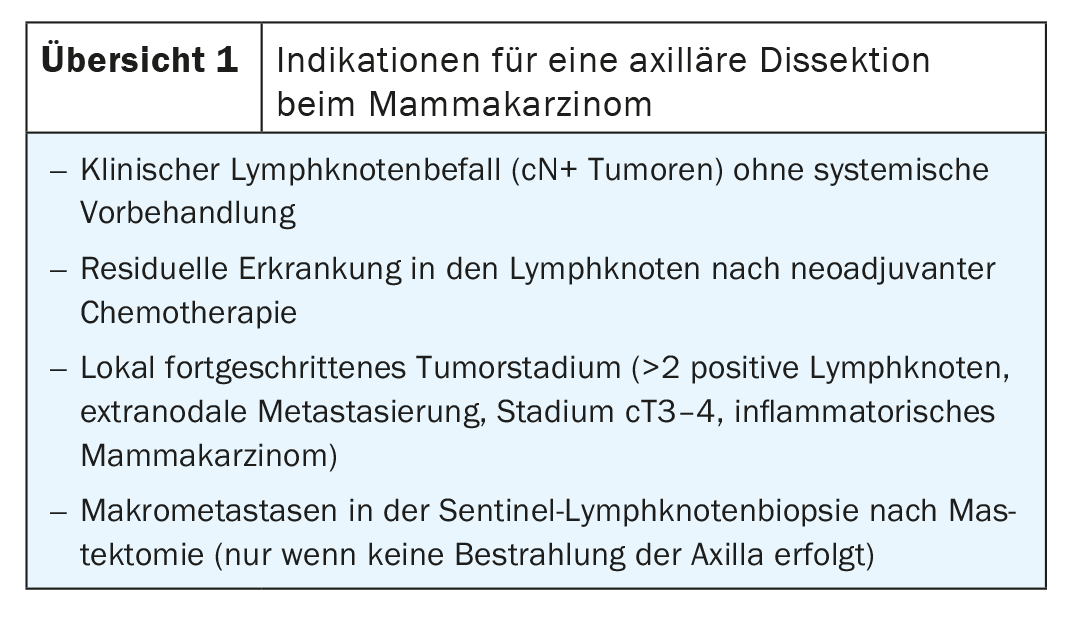
While axillary dissection was the standard of care for all breast cancer patients until 1990, there has since been a marked de-escalation in locoregional therapy. The introduction of sentinel lymph node biopsy in the 1990s proved to be a milestone in this regard. Today, axillary dissection is still recommended for those patients who clinically show lymph node involvement (cN+) and undergo primary surgery or for patients with incomplete remission of lymph node metastasis under neoadjuvant chemotherapy. Other indications for axillary dissection are locally advanced tumor stage or affected sentinel lymph nodes at mastectomy, if adjuvant radiotherapy of the axilla is not performed.
This course could continue in the near future. Among other things, this raises the question of whether surgical staging using sentinel lymph nodes can even be dispensed with in the case of clinical N0 stage. Also, ongoing studies are investigating an even narrower indication for axillary dissection in node-positive breast cancer. For example, can dissection be omitted after neoadjuvant chemotherapy even in the presence of residual tumor?
The right therapy for the right patient
In light of these developments, patient selection is at the center of optimal locoregional management of breast carcinoma. Long-term data from large studies impressively demonstrate that axillary surgery for positive sentinel lymph nodes prevents few recurrences. For example, in both the IBCSG 23-01 trial and the ACOSOG Z0011 trial, axillary recurrence rates of less than 1% at ten years were observed in breast cancer patients with positive sentinel lymph node status when axillary dissection was performed. At less than 2%, recurrence rates were only slightly higher without further local treatment of the axilla [1,2]. A positive sentinel lymph node alone is therefore by no means sufficient to decide on locoregional therapy, and the selection of suitable candidates must be more differentiated (overview 1) .
With the technical advances in radiotherapy, it can now be classified as similar in efficacy to surgical intervention, at least in the setting without systemic pretreatment [3]. In the EORTC AMAROS trial, which included 1425 breast cancer patients with positive sentinel findings, the rate of axillary recurrence at ten years was 0.9% after dissection, compared with 1.8% after radiation [3]. Even if it was not possible to statistically prove the equivalence of the two methods, these figures demonstrate the clinically high efficacy of radiotherapy. If further treatment of the axilla is necessary, both methods – radiation or surgery – can be used, depending on the individual initial situation.
Residual disease after neoadjuvant chemotherapy represents a special case in this regard. If persistence of lymph node involvement is demonstrated by sentinel lymph node examination, it is currently unclear whether radiotherapy of the axilla is sufficient. This question is currently being investigated in the Alliance A011202 trial, with initial results expected in a few years (NCT01901094). Not randomized, but no less interesting, are the results of a recent real-world analysis showing that radiation to the axilla alone after sentinel lymph node biopsy is already used instead of axillary dissection for chemotherapy-resistant tumors [4]. This with a 5-year overall survival of 71% after radiation compared with 77% after axillary dissection and radiation. Thus, in the analysis, lymph node surgery was statistically superior to radiation alone. Only in the subgroups with luminal A or B tumors with only one affected lymph node did both methods perform equally. Because of the study design, the results should be interpreted with caution, but caution against too casual an abandonment of axillary dissection in chemotherapy-resistant cases.
cN+ tumors in focus
Clinical lymph node involvement is now considered a clear indication for axillary dissection. But is the decision to operate really so clear-cut, or can locoregional treatment, including surgical staging, be dispensed with even in cN+ patients under certain conditions? This question has been on the minds of oncologists and surgeons for quite some time. A recent meta-analysis that included 13 studies with a total of 2380 patients investigated the possibility of bypassing sentinel lymph node removal after neoadjuvant systemic therapy using imaging methods [5]. Unfortunately, neither ultrasound or MRI, nor PET-CT seem to be able to reliably assess axillary response to systemic treatment. While the sensitivity of sonography was 65% and that of magnetic resonance imaging 60%, PET-CT performed even worse with a sensitivity of only 38%. Thus, at this time, pathologic examination of the lymphatic drainage pathway is still necessary to make important treatment decisions.
By means of sentinel lymph node examination, in contrast to imaging, a reliable statement can be made as to whether axillary lymph node metastases have responded to neoadjuvant therapy and thus dissection is most likely unnecessary. To prevent false negative results, it is important that at least three lymph nodes are analyzed and duplicate tracers are used [6]. Other methods already exist by means of which the sensitivity of lymph node examination after systemic therapy can be further increased. Worth mentioning at this point are the MARI ( M arking the A xillary lymph node with R adioactive I odine seeds) procedureand Targeted Axillary Dissection (TAD). Both are based on the labeling of lymph nodes with biopsy confirmed metastasis. Whereas in the MARI procedure only the labeled lymph node is selectively removed and examined after neoadjuvant systemic therapy, in the TAD procedure a sentinel lymph node biopsy is also performed [7,8]. Although the use of these methods is not yet widely established, studies have shown that the rate of false negative results has been reduced to 7% by the MARI procedure and to 2-4% by TAD [6]. In the prospective clinical SenTa study, in which 50 German centers participated, these results were largely confirmed [9]. However, it was found that the marking clip was correctly identified and removed in just under 87% of cases. This could have unpleasant consequences not only for the patient. After all, no doctor wants to leave behind a lymph node that has been affected by cancer and is even marked.
The examination of sentinel lymph nodes after neoadjuvant systemic therapy is now used in clinical practice. The question to be answered here is whether omission of axillary dissection is justifiable in the presence of negative lymph node status and initial node-positive tumors. In fact, recent data indicate that dissection in this case does not confer a survival benefit, nor is the rate of axillary recurrence higher without axillary dissection [10,11]. Even if more and more research is being conducted to clarify this issue, no clear statement can be made at present. Too many factors – for example, the value of local radiotherapy – remain unresolved. Overall, the influence of radiation seems to be increasingly important and that of false-negative results of sentinel lymph node examination surprisingly small. Thus, there is much to suggest that the indication for axillary dissection may become even narrower in the near future.
cN0: The role of the sentinel lymph node
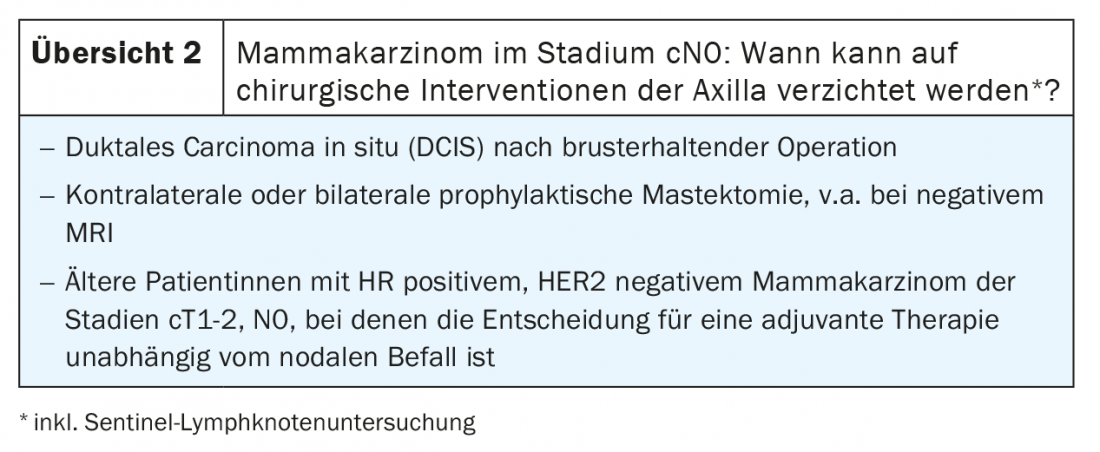
The treatment of cN0 stage breast carcinomas could soon do without axillary surgery altogether. Indeed, various studies in recent years have shown that locoregional treatment has no effect on overall survival or local recurrence rates in cN0 cases that had one to two positive lymph nodes on sentinel examination [3,12–14]. There is now a consensus that any surgical intervention of the axilla can be omitted if certain conditions are met (review 2) . However, the importance of sentinel lymph node biopsy for the choice of therapy should not be underestimated. This is because decisions regarding adjuvant breast cancer treatments are often based on histologic lymph node status. How important this role actually is and whether there are less invasive alternatives for reliable staging is currently under active investigation. There is also the question of whether knowledge of tumor biology or biomarkers is sufficient to make further treatment decisions.
Operate, but how?
If there is an indication for axillary dissection, the question of the exact procedure is increasingly raised with the advent of new procedures. Tailored approaches aim to reduce therapy-associated morbidity and increase efficiency. The TAXIS phase III trial is currently underway to evaluate the clinical concept of Tailored Axillary Surgery (TAS). In this case, palpatory conspicuous findings as well as sentinel lymph nodes are removed. Optionally, extirpation of the lymph node metastasis marked under imaging may also be performed. This is followed by regional radiotherapy. Compared to axillary dissection, the focused axillary surgery procedure is less invasive. Its purpose is to selectively reduce tumor infestation so that the disease can be effectively controlled by radiation after surgery. In a previously completed feasibility study, TAS removed a median of five lymph nodes, whereas axillary dissection removed a median of 14 additional lymph nodes. Whether focused axillary surgery can establish itself as a less radical option and rival axillary dissection in terms of efficacy remains to be seen. A first analysis of the data is expected in 2030.
Take-Home Messages
- The indication for locoregional therapy of the axilla is currently in flux. There are clear trends towards less radical surgical interventions. This applies with or without clinically visible lymph node involvement.
- A prerequisite for the best possible treatment is adequate patient selection. A careful risk-benefit assessment is essential to achieve optimal tumor control and to minimize therapy-associated morbidity.
- The role of radiotherapy in locoregional management depends on the tumor stage and is currently not fully understood.
- There is evidence that axillary dissection may be superior to radiotherapy for residual disease after neoadjuvant therapy, even when radiotherapy alone is already performed in practice.
- Currently, no validated alternatives to invasive sentinel lymph node biopsy exist. Therefore, this remains the gold standard for tumor staging. In early-stage breast cancer, a sentinel procedure may not be necessary under certain circumstances.
- Tailored surgical approaches such as TailoredAxillary Surgery (TAS) are increasingly being used to try to develop less radical alternatives to axillary dissection. Their clinical value is being tested in the ongoing TAXIS study.
Literature:
- Giuliano AE, et al: Effect of Axillary Dissection vs No Axillary Dissection on 10-Year Overall Survival Among Women With Invasive Breast Cancer and Sentinel Node Metastasis: The ACOSOG Z0011 (Alliance) Randomized Clinical Trial. JAMA. 2017; 318(10): 918-926.
- Galimberti V, et al: Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23-01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol. 2018; 19(10): 1385-1393.
- Presentation by Rutgers E: Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer patients: 10 year follow up results of the EORTC AMAROS trial. San Antonio Breast Cancer Symposium, December 6, 2018, San Antonio, Texas, USA.
- Almahariq MF, et al: Omission of an Axillary Lymph Node Dissection is Associated with Inferior Survival in Patients with Residual Nodal Disease Following Neoadjuvant Chemotherapy. International Journal of Radiation Oncology, Biology, Physics. 2020; 108(3): S152-S3.
- Samiei S, et al: Diagnostic Performance of Noninvasive Imaging for Assessment of Axillary Response After Neoadjuvant Systemic Therapy in Clinically Node-positive Breast Cancer: A Systematic Review and Meta-analysis. Ann Surg. 2021; 273(4): 694-700.
- Simons JM, et al: Diagnostic Accuracy of Different Surgical Procedures for Axillary Staging After Neoadjuvant Systemic Therapy in Node-positive Breast Cancer: A Systematic Review and Meta-analysis. Ann Surg. 2019; 269(3): 432-442.
- Donker M, et al: Marking axillary lymph nodes with radioactive iodine seeds for axillary staging after neoadjuvant systemic treatment in breast cancer patients: the MARI procedure. Ann Surg. 2015; 261(2): 378-382.
- Caudle AS, et al: Improved Axillary Evaluation Following Neoadjuvant Therapy for Patients With Node-Positive Breast Cancer Using Selective Evaluation of Clipped Nodes: Implementation of Targeted Axillary Dissection. J Clin Oncol. 2016; 34(10): 1072-1078.
- Kuemmel S, et al: A Prospective, Multicenter Registry Study to Evaluate the Clinical Feasibility of Targeted Axillary Dissection (TAD) in Node-Positive Breast Cancer Patients. Ann Surg. 2020. doi: 10.1097/SLA.00000000004572. epub ahead of print.
- Wong SM, et al: Oncologic Safety of Sentinel Lymph Node Biopsy Alone After Neoadjuvant Chemotherapy for Breast Cancer. Ann Surg Oncol. 2021; 28(5): 2621-2629.
- Galimberti V, et al: Sentinel node biopsy after neoadjuvant treatment in breast cancer: Five-year follow-up of patients with clinically node-negative or node-positive disease before treatment. Eur J Surg Oncol. 2016; 42(3): 361-368.
- Giuliano AE, et al: Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010; 252(3): 426-32; discussion 32-33.
- Giuliano AE, et al: Locoregional Recurrence After Sentinel Lymph Node Dissection With or Without Axillary Dissection in Patients With Sentinel Lymph Node Metastases: Long-term Follow-up From the American College of Surgeons Oncology Group (Alliance) ACOSOG Z0011 Randomized Trial. Ann Surg. 2016; 264(3): 413-420.
- Donker M, et al: Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014; 15(12): 1303-1310.
InFo ONCOLOGY & HEMATOLOGY 2021; 9(3): 6-9.