Back pain has become a common disease. Upright gait, lack of movement, overweight and inadequate load on the spine increase the physiological aging processes of the intervertebral discs and the degeneration of the other spinal structures.
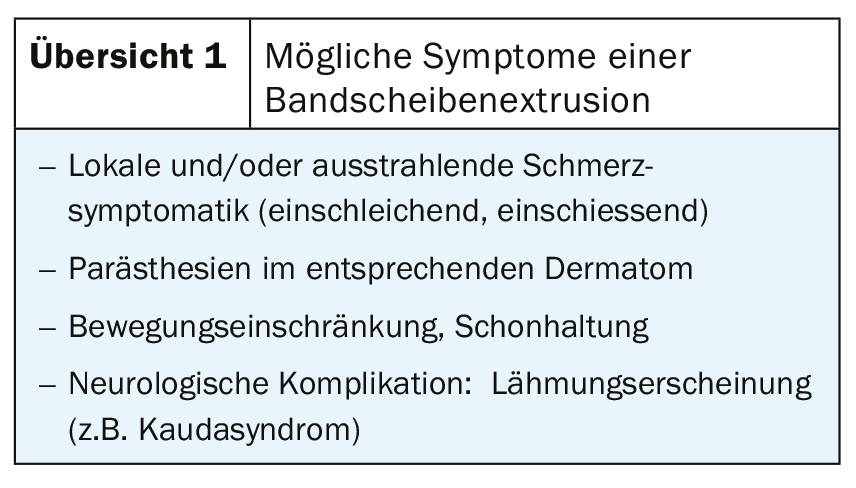
Especially in adults, psychosocial factors should be considered in addition to physiological aspects [8]. Depending on the clinical symptoms and neurological situation, the method with the best informative value, least invasiveness, availability, experience of the examiner, alternative possibilities (radiation exposure) and a balanced cost-benefit ratio should be selected for imaging diagnostics. Overview 1 lists the possible symptoms of disc extrusion. However, not all disc dislocations detectable on diagnostic imaging are symptomatic. Clinical symptoms, neurological and image diagnostic findings must correlate to derive a therapeutic consequence.
Following the discovery of X-rays by W.C. Röntgen in 1895, the development of computed tomography and, in particular, magnetic resonance imaging (MRI) also revolutionized imaging of the spine. The neuroaxis and surrounding structures of the spinal canal and spine could be visualized in detail noninvasively. Conventional radiographs have become less important in routine imaging diagnostics following the introduction of CT and MRI. Indications still arise in the clarification of primarily bony degenerative and inflammatory as well as traumatic changes, as well as anomalies and developmental anomalies. Today, magnetic resonance imaging undoubtedly represents the imaging method of the spine with the most comprehensive statements, significantly expanding and improving the information content of X-ray diagnostics, myelography and computed tomography (CT). Visualization of the extent of disc degeneration, concomitant changes in the vertebral endplates, ligamentous reactions, as well as wear of the vertebral joints and signs of possible instability and resulting dysstatics allow the symptoms to be causally assigned [4].
Computed tomography and magnetic resonance imaging have not only revolutionized neuroimaging, but also significantly reduced or eliminated the risks associated with invasive examination procedures. This is also reflected in the replacement of surgical therapies with minimally invasive neuroradiological procedures. For the minimally invasive procedures that can be performed primarily on an outpatient basis, the preinterventional imaging examination not only has the task of diagnosing the cause of the complaints, but also of confirming the indication or contraindications. The radiological minimally invasive therapy option, CT-guided periradicular therapy (PRT), has already been referred to in a previous report. A clear conceptual definition of disc displacement should be universal and should be based on the current 2014 version developed by three professional societies: the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology [1]. Table 1 lists the current version of the nomenclature, based on that of 1995 with update 2001.
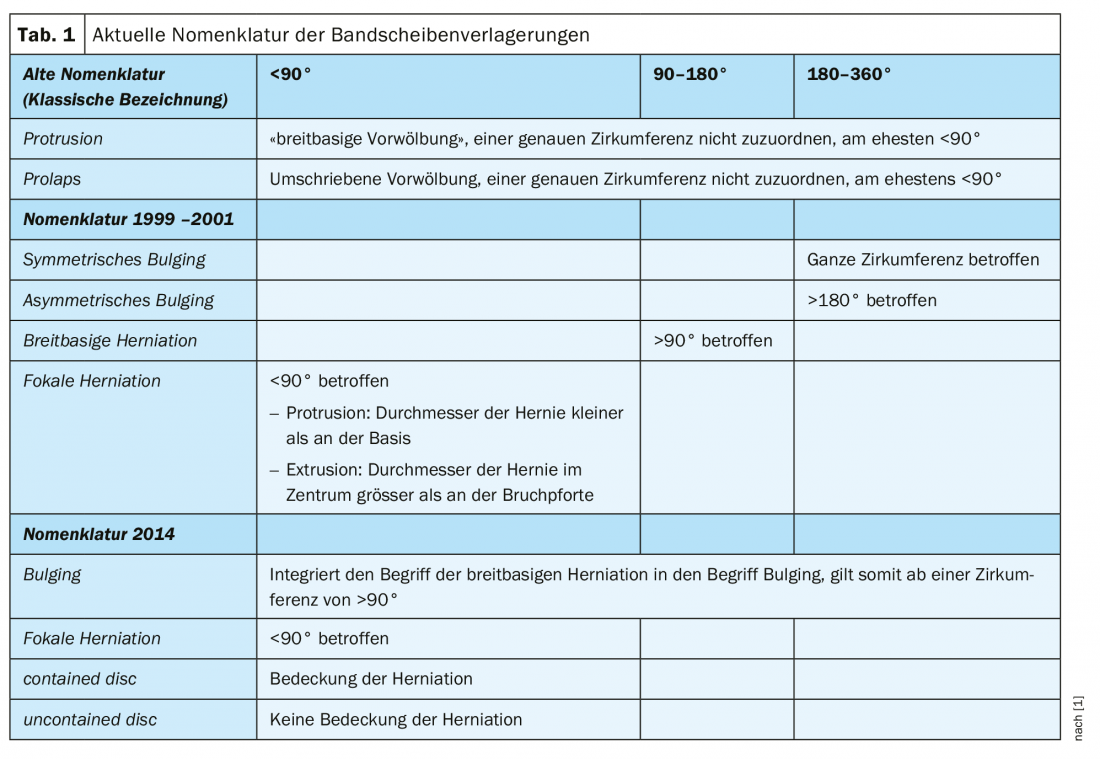
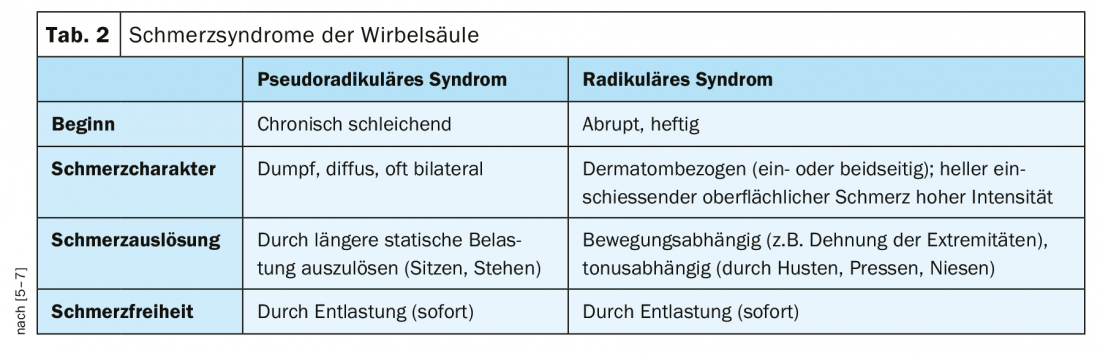
In daily practice, the description of disc displacement as disc protrusion or bulging disc and disc prolapse or extrusion is common and, especially for many referrers, the understandable, ultimately also common nomenclature for many years. The differentiation of vertebral pain symptoms is shown in Table 2 [6,7,9].
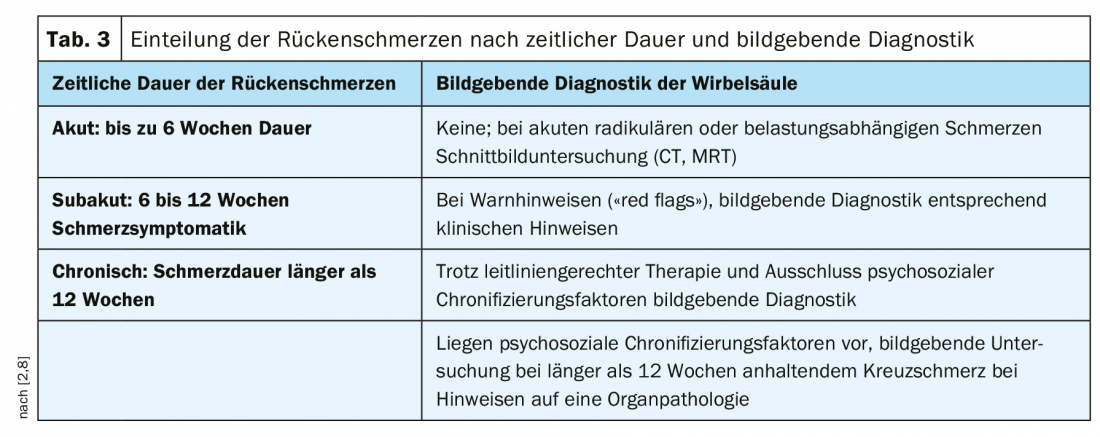
Information on the performance of diagnostic imaging procedures depending on the duration of vertebrogenic symptoms is provided in Table 3 [2,8].
Case studies
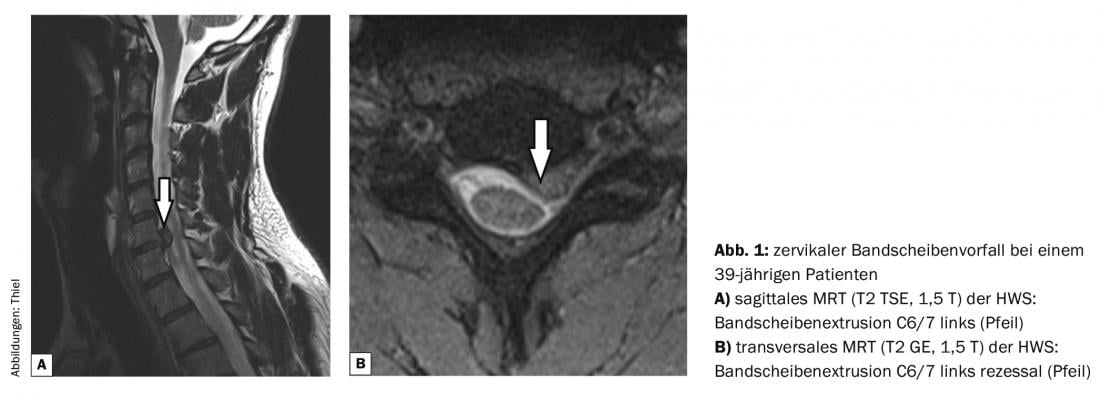
Case report 1 shows a cervical disc herniation in a 39-year-old patient who complained of paresthesias in the fingers of the left hand and pain radiating to the arm, associated with neck stiffness and headache. MR tomography demonstrated a herniated disc in the C6/7 segment on the left (Fig. 1).
In case report 2 (Fig. 2), a right recessive disc herniation in a 29-year-old man in the L5/S1 segment is the cause of right lumboischialgia, also confirmed by MRI.
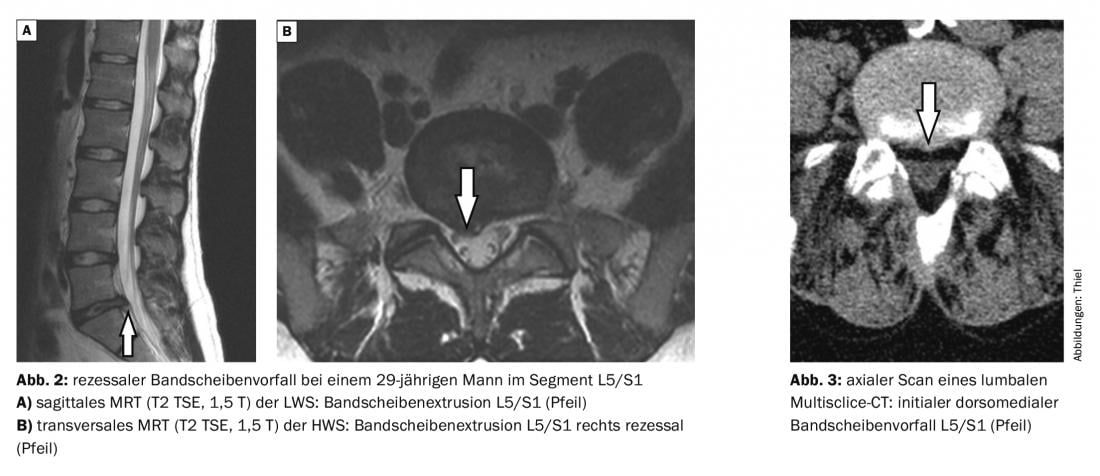
In case report 3, a small dorsomedial subligamentous extrusion of the L5/S1 ligamentous disc (lumbar multislice CT) is the cause of reciprocal complaints.
Take-Home Messages
- Spinal disc extrusions may be clinically silent, and not every disc dislocation is relevant.
- The symptomatology is variable, rarely occurs the
- “neurologic emergency,” which may also require immediate neurosurgical intervention.
- The use of imaging depends on the extent and duration of the symptomatology.
Literature:
- Breitenseher JB, Pones M, Breitenseher MJ: Nomenclature of the (lumbar) intervertebral discs. Radiology up2date 2017; 17: 63-77.
- German Medical Association (BÄK), National Association of Statutory Health Insurance Physicians (KBV), Association of the Scientific Medical Societies (AWMF): Nationale VersorgungsLeitlinie Kreuzschmerz – Langfassung. Version 1.X.2010.
- Casazza BA: Diagnosis and treatment of acute low back pain. Am Fam Physician 2012; 85(4): 343-350.
- Emch TM, Modic MT: Imaging of lumbar degenerative disk disease: history and current state. Skeletal Radiol 2011; 40(9): 1175-1189.
- Grönemeyer DHW, Seibel RMM: Interventional computed tomography. Vienna, Berlin: Ueberreuter Wissenschaft, 1989 (3-4): 94-103.
- Grönemeyer DHW, Thiel H.-J, Moser C: Tomographic periradicular microtherapy. Berlin: ABW Wissenschaftsverlag GmbH, 2013; pp. 16-20, pp. 40-43, pp. 79-81, pp. 93-104, pp. 119-143.
- Junker U, Nolte T: Fundamentals of special pain therapy. Munich: Urban & Vogel, 2005.
- Kloska S, Freund M: Radiological diagnosis of intervertebral disc lesions. Radiology up2date 2003; 1: 37-55.
- Thiel HJ: CT-guided PRT for MTRA. Berlin: ABW Wissenschaftsverlag, 2014.
GP PRACTICE 2020; 15(3): 36-38











