The older men get, the more likely they are to have a testosterone deficiency. But hypogonadism is not present until it is confirmed in two laboratories.
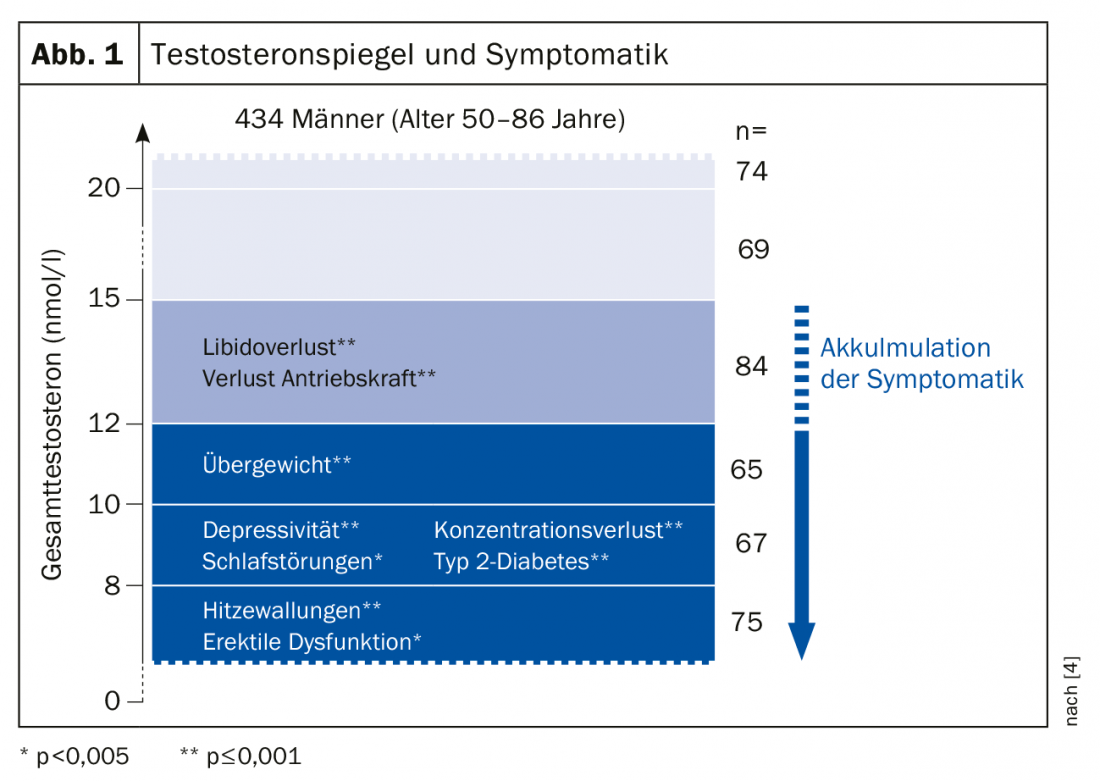
The sex hormone testosterone plays a very important role for the male organism. For example, it influences almost all organ systems of the male body, which is why a permanent testosterone deficiency ultimately leads in many cases to psychological (irritability, nervousness, depression, limitation of cognitive abilities), physical (increase in abdominal fat, decrease in muscle mass, hot flashes, osteopenia/osteoporosis, metabolic syndrome) and sexual symptoms (loss of libido, erectile dysfunction) (Fig. 1).
It is important for physicians that the symptoms listed above are usually only a first indication of a testosterone deficiency (=symptomatic hypogonadism). Caveat: Hypogonadism should not be diagnosed based on presenting symptoms alone. This always requires confirmation in the laboratory twice. This means that in addition to the corresponding symptoms, there must also be repeatedly low testosterone levels in the blood.
In practice, however, it is often the case that symptoms suggesting hypogonadism are overlooked, or men simply do not bring up certain symptoms. Only about 50% of the medical profession thinks of a possible hormone deficiency when it comes to symptoms such as hot flashes in men. The patient is not diagnosed and often lives with the symptoms untreated for several years. Such a failure, however, can have far-reaching health consequences for the patients concerned: For example, a prolonged testosterone deficiency leads to libido and erectile dysfunction. Likewise, fertility problems may occur. In the case of a prolonged, unfulfilled desire to have children, you should therefore also think at least once about the man and his testosterone balance.
Men generally only go to a doctor when sexual problems begin to interfere with their love life in the long term. In keeping with our performance-oriented consumer society, the majority of men will demand that you, as their doctor, give them a “blue pill” that will fix the problem quickly and as if at the push of a button. However, a fact of daily practice is that almost every third man who consults a doctor because of erectile dysfunction already suffers from a manifest testosterone deficiency and is therefore more in need of a causal therapy by means of testosterone replacement.
Take hypogonadism seriously and treat it
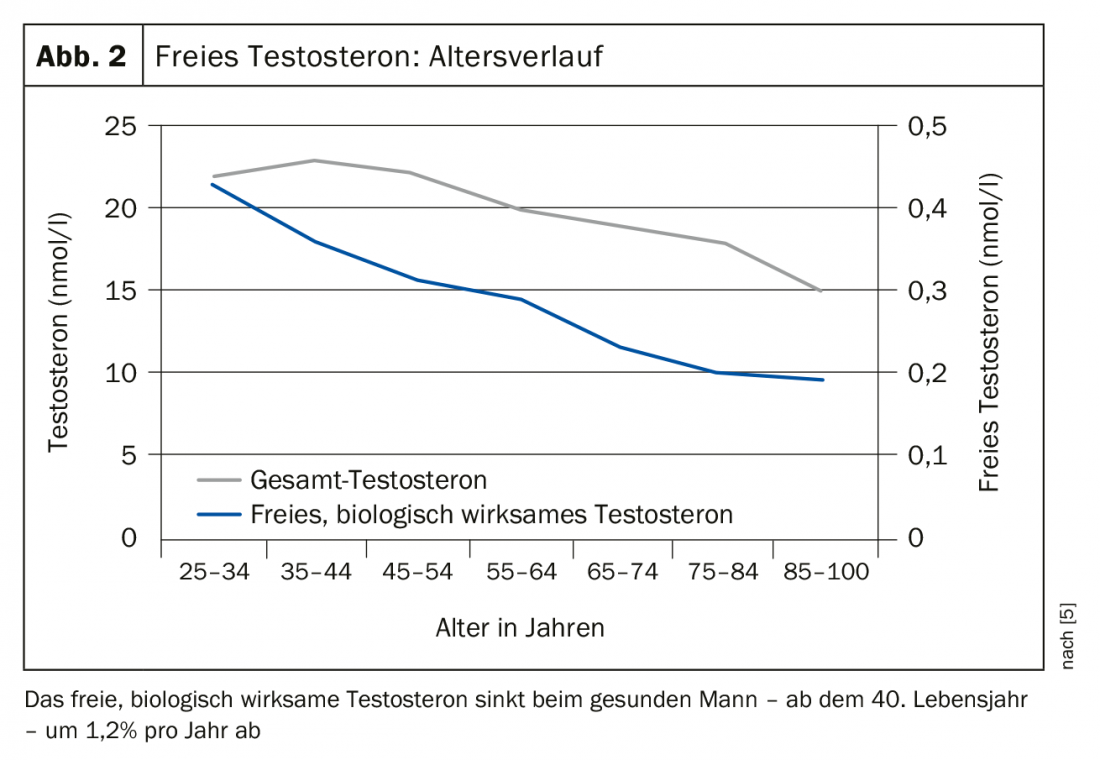
In aging men, the testosterone level also naturally decreases continuously (Fig. 2) . This can most likely be explained by the fact that – comparable to women – men are biologically approaching the end of their reproductive years. In addition to this age-related drop in hormones, however, men’s testosterone levels are also affected by an unfavorable lifestyle. Such lifestyle factors then act at a young age and can have an impact on hormone levels.
These negative influencing factors include obesity, physical and mental stress, excessive alcohol consumption, reduced sexual activity, and acute or chronic illnesses (infections, heart attacks, HIV infection, cirrhosis of the liver, kidney disease, hypothyroidism, diabetes mellitus, or even asthma).
The testosterone deficiency is therefore by no means a “lifestyle phenomenon” or an expression of a temporary condition of the aging man. Confirmed hypogonadism, on the contrary, forms the basis for other, much more serious health problems. Moreover, men with testosterone deficiency even have a higher mortality risk. For example, the risk of mortality in hypogonadal men with testosterone levels <2.5 ng/ml is more than twice that of men with normal testosterone levels (overall risk; OR=2.24). At the same time, men with normal testosterone are less likely to suffer from cardiovascular disease (OR 0.7). In contrast, men with low-normal or hypogonadal testosterone levels are about twice as likely to suffer a stroke, for example.
Cave: Therefore, current EAU guidelines recommend that men with laboratory-confirmed hypogonadism be substituted with testosterone [1].
Testosterone substitution is safe
Testosterone treatment for hypogonadal men – and only in these is testosterone replacement really indicated – has always faced very strong debate. But where does this negative image of testosterone substitution actually come from?
Although long disproven by studies, some physicians, but especially patients, still fear that testosterone substitution could cause prostate cancer or further promote a previously undetected tumor. However, even after years of substitution treatment with testosterone, there is no evidence for this, neither in studies nor from daily practice.
However, a study published by Vigen and colleagues back in 2013 [2] initially concluded that men on substitution may have an increased cardiovascular risk. However, the study was flawed and after correction of the calculations, the statement of higher cardiovascular risks under testosterone substitution was also no longer tenable. Nevertheless, the study remained present in people’s minds until today and unsettled both patients and treating physicians.
Vigen and colleagues claimed in the original version of their article that testosterone administration led to higher cardiovascular risks in appropriately predisposed patients. The article’s statements were then continually cited as evidence of a link between testosterone administration and resulting cardiovascular disease. Subsequently, the worldwide media picked up on this story, making it known to a wide audience.
However, the correction of the results shortly thereafter received little media attention, so that the original misinformation led to a distorted perception of testosterone substitution. As a result, patients’ trust in the health care system was permanently damaged with regard to men’s health.
In fact, however, the study had serious flaws. As a result, the study result was not only falsified, but downright reversed.
The errors of the JAMA study in detail
Six days after its first appearance, the article was already corrected. Another three months passed before the major errors of the study were finally published: For example, one group of men included in the study did not include 1132 as previously stated, but after reviewing the data, there were only 128 men (!). The error rate within this study group was thus an impressive 89%!
A second group was reportedly composed of more than 900 men. Surprisingly, examination of these data after the study was published revealed that 100 women were among the 900 men reported – 10% of this group studied were therefore of the “wrong” sex for the study.
After the necessary corrections of the data, many of the statements of the study now finally read completely different: 10.1% of the men who received testosterone suffered a heart attack or a stroke or died during the study period. In contrast, 21.2% of the men in the untreated group suffered a heart attack, stroke or died – so without testosterone replacement, even twice as many men with a manifest hormone deficiency were affected by cardiovascular events.
Testosterone deficiency/hypogonadism in everyday practice
Testosterone deficiency and hypogonadism requiring therapy are, moreover, very common in practice, and not only in older men. In October 2017, the German Society for Men and Health (DGMG) published for the first time results from its own nationwide cross-sectional study called the “20,000 Testosterone Study” [3].
In this study, blood samples from more than 20,000 men between the ages of 18 and 100 were analyzed for their respective testosterone levels. As a result, almost one in seven men suffered from a significant testosterone deficiency – the majority of the values were below 8.7 nmol/l (<2.5 ng/ml).
As already explained at the beginning, such a pronounced testosterone deficiency more often shows symptoms and threatens health consequences for the affected men. In the “20,000 Testosterone Study” [3] of the DGMG, men with hormone deficiency were much more likely to have hypertension (+41%) and type 2 diabetes mellitus (+68%).
In addition, other international studies also confirm these connections between lowered testosterone levels and the increasingly widespread diseases of civilization today, including a higher risk of cardiovascular disease.
Important: If you have a reasonable suspicion of a testosterone deficiency in a patient based on the symptoms, the testosterone value must be determined as a “health insurance service”. If the testosterone level is confirmed by laboratory diagnosis after two independent measurements, hypogonadism requiring treatment and billing is present.
Laboratory measurement remains a prerequisite for diagnosis!
The testosterone value can be determined as follows if hypogonadism is suspected: According to the current EAU recommendations [1], the testosterone value from the blood should always be determined in the morning before 11 am and on an empty stomach. Importantly, the blood draw must be performed on two independent dates and the testosterone determination must be performed using a validated test method.
The current EAU guideline gives as reference values for testosterone concentration in men:
Total testosterone
- Normal range: ≥12.1 nmol/l (≥3.5 ng/ml)
- Limit range: 8-12 nmol/l (2.3-3.5 ng/ml)
- Testosterone deficiency: <8 nmol/l (<2.3 ng/ml)
Free testosterone
- Testosterone deficiency: <243 pmol/l (=0.243 nmol/l; <0.07 ng/ml)
Important for practice: For a confirmed diagnosis of hypogonadism, at least two independent testosterone values must be determined, both showing low total testosterone values or decreased free testosterone values. In addition, the man must have symptoms, e.g. suffer from fatigue, loss of libido or lack of drive.
No testosterone in the absence of a medical indication
Occasionally, patients may present to the practice who do not suffer from hypogonadism but ask for testosterone replacement, e.g., for mood swings or to increase libido in times of stress. You should clearly explain to these men that testosterone substitution is not possible without laboratory-confirmed hypogonadism as a treatment-related indication. Testosterone is by no means a feel-good drug for tired men. Neither is it a magic bullet against belly fat and obesity. Rather, testosterone replacement therapy is used to correct laboratory-confirmed symptomatic hypogonadism in men. On the one hand, it is intended to bring testosterone back into the normal range for the patient’s age and, on the other hand, to reduce the possible risk of serious secondary diseases.
Men with testosterone levels in the low normal range should instead be advised to be more active, control their weight, and maintain a healthy alternation of tension and relaxation in combination with sufficient nighttime sleep. This will help most overcome the low mood or performance slump entirely without testosterone replacement therapy.
Conclusion
While women change, men tend to lose weight – so there is no such thing as an andropause comparable to menopause in the true sense of the word. The corresponding clinical picture of male testosterone deficiency is called hypogonadism. This is a condition that requires treatment and is not a matter of wellness, as numerous studies have now proven. If men suffer from a permanent testosterone deficiency – up to confirmed hypogonadism – they are at risk of cardiovascular diseases, obesity and type 2 diabetes mellitus. The comorbidities of untreated, manifest hypogonadism cost men their health and quality of life, and possibly even their lifetime.
Take-Home Messages
- Hypogonadism is a common condition of the aging male that requires treatment. If left untreated, there is a risk of cardiovascular disease,
- Obesity as well as diabetes mellitus type 2.
- For a confirmed diagnosis, two independent testosterone values must be obtained, both showing low levels of total testosterone or decreased levels of free testosterone. In addition, other symptoms such as fatigue, loss of libido or listlessness must be present.
- As a rule, testosterone substitution is very effective. However, this should only be used in cases of laboratory-confirmed hypogonadism.
Literature:
- Dohle GR, et al: Guidelines on Male Hypogonadism. European Association of Urology 2018. https://uroweb.org/guideline/male-hypogonadism/
- Vigen R, et al: Association of Testosterone Therapy with Mortality, Myocardial Infarction, and Stroke in Men With Low Testosterone Levels. JAMA 2013; 310(17): 1829-1836.
- German Society for Men and Health, November 2017, “DGMG 20,000 Testosterone Study,” www.mann-und-gesundheit.com/aktuelles/105-deutsche-testosteron-studie-auf-weltniveau.
- Zitzmann M, Faber S, Nieschlag E: Association of specific symptoms and metabolic risks with serum testosterone in older men. J Clin Endocrinol Metab 2006; 91(11): 4335-4343.
- Leifke E, et al: Age-related changes of serum sex hormones, insulin-like growth factor-1 and sex-hormone binding globulin levels in men: cross-sectional data from a healthy male cohort. Clin Endocrinol 2000; 53(6): 689-695.
Further reading:
- Deutsche Gesellschaft für Mann und Gesundheit e. V., December 2018, “Precautionary Guide to Men’s Health for Physicians.” https://www.mann-und-gesundheit.com
- Deutsche Gesellschaft für Urologie e.V. Hypogonadism: When is hormone therapy useful. Business magazine for the urologist 2016; 5.
- Hackett G, et al: Serum testosterone, testosterone replacement therapy and all-cause mortality in men with type 2 diabetes: retrospective consideration of the impact of PDE5 inhibitors and statins. Int J Clin Pract 2016; 70(3): 244-253.
- Haider A, Yassin A, Doros G, Saad F: Effects of Long-Term Testosterone Therapy on Patients with “Diabesity”: Results of Observational Studies of Pooled Analyses in Obese Hypogonadal Men with Type 2 Diabetes. Int J Endocrinol 2014; 2014: 683515. doi: 10.1155/2014/683515. Epub 2014 Mar 11.
- Kapoor D, Goodwin E, Channer KS, Jones TH: Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol 2006; 154: 899-906.
- Muraleedharan V, et al: Testosterone deficiency is asssociated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur J Endocrinol 2013; 169: 725-733.
- Rao PM, Kelly DM, Jones TH: Testosterone and insulin resistance in the metabolic syndrome and T2DM in men. Nat Rev Endocrinol 2013; 9: 479-493. doi: 10.1038/nrendo.2013.122. Epub 2013 Jun 25.
- Schipf S, et al: Low total testosterone is associated with increased risk of incident type 2 diabetes mellitus in men: results from the Study of Health in Pomerania (SHIP). Aging Male 2011; 14(3): 168-175. doi: 10.3109/13685538.2010.524955. epub 2010 Nov 2.
HAUSARZT PRAXIS 2019; 14(5): 14-18