The standard treatment for acute venous thromboembolism currently includes parenteral heparin administration, overlapping with the administration of a vitamin K antagonist (VKA). New oral anticoagulants (NOACs) and VKAs show different mechanisms of action: whereas VKAs reduce the activability of vitamin K-dependent coagulation factors, heparins (indirectly, via antithrombin) and the NOACs (directly) inhibit activated factors Xa and/or IIa. For patients stably adjusted to VKAs with corresponding efficiency of the therapy performed, there is no compelling reason to switch to one of the NOACs. The three new oral anticoagulants with the most advanced clinical development are dabigatran, rivaroxaban, and apixaban. Secondary costs such as monitoring are reduced with them, thereby possibly also enabling a higher quality of life with long-term oral anticoagulation.
Oral anticoagulation is commonly used to prevent thromboembolism in patients with atrial fibrillation (AF), mechanical heart valves, and in the secondary prevention of venous thromboembolism (VTE) and for less common, other indications.
Acute venous thromboembolism (deep vein thrombosis [TVT] or pulmonary embolism [LE]) shows an annual incidence of 1-2 cases per 1000 persons in the general population. Short-term (acute) treatment reduces the risk of recurrence from over 20% to about 3% in the first twelve months after initiation of therapy.
The standard treatment of acute venous thromboembolism currently includes parenteral heparin administration, overlapping with the administration of a vitamin K antagonist.
Oral vitamin K antagonists (VKA, e.g., acenocoumarol or phenprocoumon), which have been used for the past 60 years, have several limitations:
- They show delayed onset and delayed onset of action
- The large interindividual variability of the dose-response relationship requires a narrow therapeutic window and regular monitoring of the International Normalized Ratio (INR)
- Despite careful dosage adjustment, the INR is often outside the target range, which increases the risk of thromboembolism and bleeding
- There is a relevant potential for interaction with drugs and food.
When VKA therapy is implemented, the risk of major bleeding after the first year is 1-2%. Therefore, it remains to be constantly weighed whether the prevention of a possible recurrence outweighs the risk of a possible hemorrhage.
Factor Xa initiates the common terminal pathway of the coagulation cascade and thus leads to the formation of thrombin, which induces positive feedback responses as well as promotes platelet activation. New oral anticoagulants (NOACs) and VKAs show different mechanisms of action: whereas VKAs reduce the activability of vitamin K-dependent coagulation factors, heparins (indirectly, via antithrombin) and the NOACs (directly) inhibit activated factors Xa and/or IIa
New oral anticoagulants
NOACs reach peak levels and efficacy within two to three hours after a dose. In future, this should make it possible to dispense with treatment with two different substances, as was previously necessary (heparins and VKA).
The new compounds generally exhibit predictable pharmacokinetics, and the potential for interaction with other drugs is low (but must still be considered where such a potential for interaction exists). However, the different elimination mechanisms of NOACs, especially the distinction between renal and hepatic elimination, must be taken into account. The three new oral anticoagulants with the most advanced clinical development are dabigatran, rivaroxaban, and apixaban.
Dabigatran etexilate
Dabigatran etexilate (Pradaxa®) is a prodrug that is hydrolyzed to the thrombin inhibitor dabigatran, which binds to the active site, inhibiting both fibrin-bound and unbound thrombin. Unfractionated heparin and low-molecular-weight heparins do not inhibit fibrin-bound thrombin.
The absolute bioavailability of dabigatran etexilate after oral administration is 6.5%. Plasma concentration and corresponding anticoagulant effect are dose-dependent, with a peak within two hours. The mean terminal half-life of dabigatran after oral administration is approximately eight hours after a single dose or twelve to 14 hours after multiple doses.
Half-life is significantly increased in patients with creatinine clearance <30 ml/min (>24 h), as renal elimination of dabigatran is the major mechanism of excretion. In patients with renal impairment, this relevantly increases the risk of bleeding due to accumulation. Therefore, in patients at increased risk of renal dysfunction on long-term dabigatran therapy, regular monitoring of renal function is clinically imperative.
In Switzerland, dabigatran 2×150 mg daily (Pradaxa®) is approved for stroke prophylaxis in non-valvular atrial fibrillation based on the RE-LY study in the presence of one or more of the following risk factors: previous stroke, transient ischemic attack or systemic embolism, left ventricular ejection fraction <40%, symptomatic heart failure (≥ NYHA class 2), age ≥75 years, or age ≥65 years with diabetes mellitus, CHD, or arterial hypertension. In patients at increased risk of bleeding, 2 x 110 mg daily may be considered.
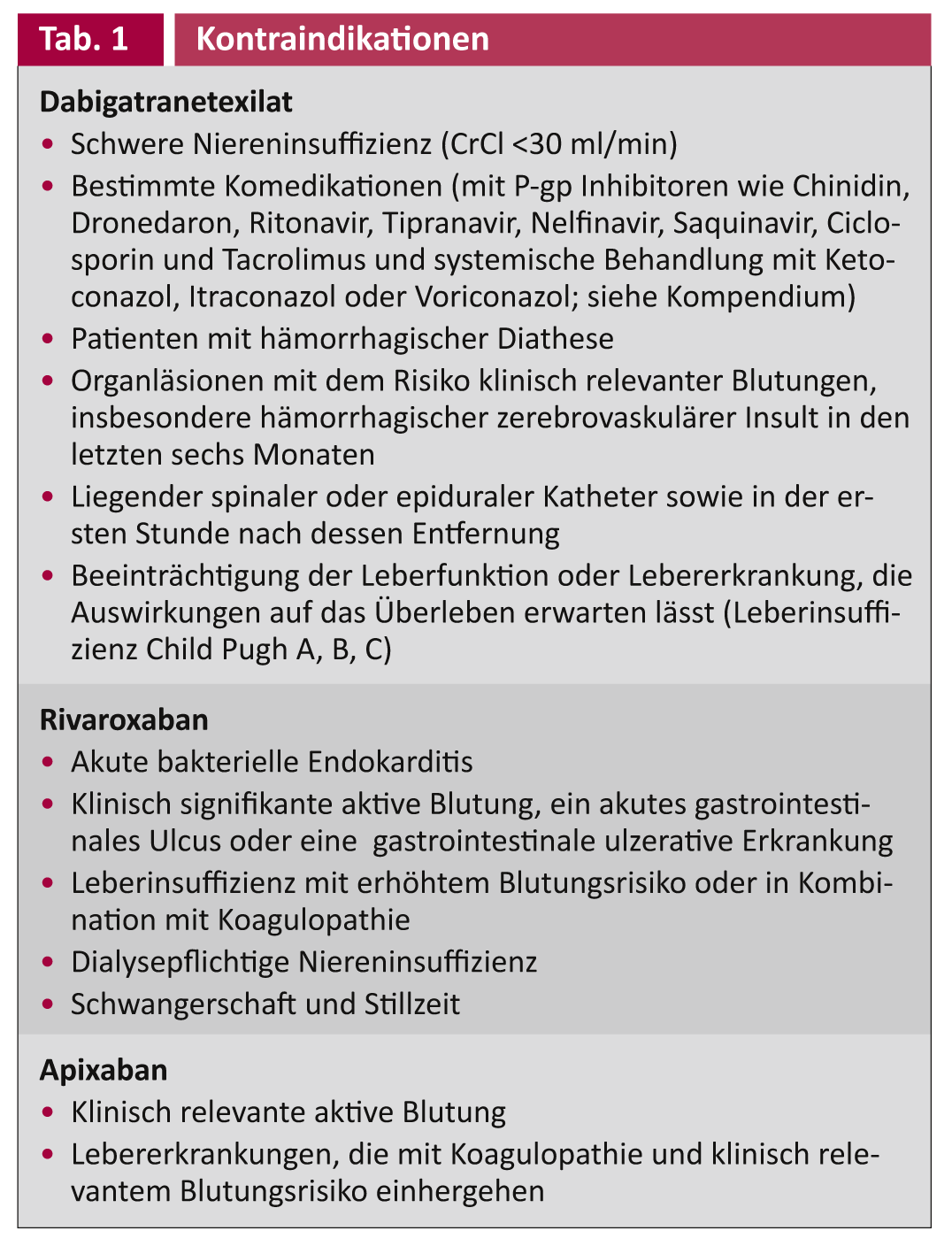
The contraindications besides hypersensitivity are summarized in Table 1. Use during pregnancy and lactation is not recommended due to the current lack of data and experience. The RE-LY trial showed that dabigatran 150 mg 2 x/day was significantly more likely to prevent stroke and systemic embolism than treatment with warfarin (INR 2-3) (Relative risk with dabigatran 0.66 [95% KI 0,53–0,82]). At the same time, dabigatran 150 mg 2 x/day was associated with significantly less life-threatening and intracranial bleeding.
Rivaroxaban
Rivaroxaban (Xarelto®) is a direct and potent inhibitor of factor Xa. It acts by inhibiting circulating factor Xa and factor Xa in the prothrombinase complex and thrombus-associated factor Xa, respectively.
Rivaroxaban has relatively high bioavailability (80-100%), is well tolerated gastrointestinally, and has a rapid onset of action with predictable pharmacokinetics. Its half-life is about five to nine hours, and two-thirds of it is excreted by the kidneys and one-third by the liver. Again, there is only a small risk of interaction from food intake or other medications (but these must be taken into account if present).
Rivaroxaban (Xarelto®) is approved in Switzerland for thromboprophylaxis after major orthopedic surgery of the lower extremity, for stroke prophylaxis in non-valvular atrial fibrillation, for the treatment of deep vein thrombosis, and for recurrence prophylaxis after venous thrombosis or pulmonary embolism.
The contraindications besides hypersensitivity are summarized in Table 1.
In the RECORD trial program, Xarelto 10 mg daily was shown to be superior in efficacy to the standard European regimen for thromboprophylaxis in hip and knee replacement. There was a significant, marked reduction in the incidence of deep vein thrombosis with a slightly higher, but not significantly different, bleeding rate. This resulted in a significant clinical “net benefit” (HR 0.69, 95% CI 0.53-0.89).
The EINSTEIN program reviewed in randomized trials treatment and recurrence prophylaxis after acute deep vein thrombosis, treatment of acute pulmonary embolism (approval pending), and prolonged recurrence prophylaxis following treatment of acute deep vein thrombosis (EINSTEIN extension).
In the EINSTEIN-TVT trial, rivaroxaban (15 mg twice daily for the first 3 weeks, followed by 20 mg once daily) was compared with the “classic” regimen (low-molecular-weight heparin plus vitamin K antagonist). Statistically comparable results were found with respect to the primary endpoint (recurrence frequency), with a trend toward better control with rivaroxaban (HR 0.68, 95% CI 0.44-1.04).
The EINSTEIN-Extension study showed a significant, pronounced improvement (HR 0.18; 95% CI 0.9-0.39) in patients with questionable indication for continued relapse prophylaxis (20 mg once daily) with respect to efficacy versus placebo.
The Einstein trial showed comparable bleeding rates between the two treatment arms, resulting in a net clinical benefit significantly in favor of rivaroxaban (HR 0.67, 95% CI 0.47-0.95).
Apixaban
Apixaban (Eliquis®) is another new oral direct Factor Xa inhibitor. Apixaban has an oral bioavailability greater than 50%. The peak concentration is reached after about three hours, and its half-life is about twelve hours. Apixaban is excreted approximately two-thirds by the liver and approximately one-third by the kidney. There is no relevant interaction with food; again, interaction with other drugs is rare but must be considered if present.
Apixaban has so far been approved in Switzerland for thromboprophylaxis after hip and knee replacement (2.5 mg 2 x daily); other indications are currently in the approval process. The contraindications besides hypersensitivity are summarized in Table 1. Use in patients with a CrCl <15 ml/min is not recommended, nor is use during pregnancy and lactation. Apixaban should be used only with caution and under clinical supervision together with strong inhibitors or inducers of CYP3A4 and P-gp.
Other considerations
The new anticoagulants show many potential advantages over coumarins, including their rapid onset of action, predictable therapeutic effect, and limited drug interactions.
Since monitoring of drug efficacy is usually not necessary with the new anticoagulants, it remains to be seen whether this could lead to delayed detection of complications and/or recurrences; however, based on experience to date, there is no evidence for this. However, due to partial or near-complete renal elimination, monitoring of renal (and hepatic) function must be kept in mind when using NOACS.
For patients stably adjusted to VKAs with corresponding efficiency of the therapy performed, there is no compelling reason to switch to one of the NOACs. Coumarins are very inexpensive and the actual drug costs of the new oral anticoagulants are currently much higher. On the other hand, secondary costs such as monitoring are reduced, possibly allowing for a higher quality of life with long-term oral anticoagulation.
However, coumarins will remain the primary treatment option for patients with mechanical heart valves, at least for the time being, but appropriate trials for NOACs are already underway. Coumarins also remain a good option for patients whose compliance needs to be assessed.
Conclusion for practice
- In summary, currently available data show that the new oral anticoagulants represent an attractive, safe, and efficient(er) alternative to anticoagulation with VKAs in the approved indications.
Literature list with the authors
CARDIOVASC 2012; no. 6: 13-16.











