At the Swiss Derma Day 2016, visitors could expect an extensive program and a great variety of content. One topic was the treatment of severe acne. What are the treatment options and what should be considered when using isotretinoin? Other topics included UV-related hyperpigmentation and adverse dermatologic travel souvenirs.
Vincenzo Bettoli, MD, Ferrara (I), spoke about treatment approaches for severe acne. First of all, one must be diagnosed. Key points in the history are a detailed description of the clinical development, family background regarding acne, degree of psychological distress (VAS scale 1-10), hormonal situation (clinical signs of hyperandrogenism), contact with toxic substances, concomitant dermatological/systemic diseases, intake of dietary supplements (hormones, proteins, arachidonic acid, etc.), side effects and effects of previous treatments (long-term use of oral antibiotics, flare with oral isotretinoin, dose and onset of oral isotretinoin, etc.).), side effects and effects of previous treatments (long-term use of oral antibiotics, poor tolerance of topicals, flare with oral isotretinoin, dose and onset of oral isotretinoin, etc.) and, most importantly, planned pregnancies. In principle, the following therapeutic agents are used (according to the European S3 guidelines [1]):
- With high recommendation oral isotretinoin as monotherapy, both for severe papulopustular/moderate nodular acne and for severe nodular acne/acne conglobata.
- With moderate level of recommendation for severe papulopustular/moderate nodular acne, systemic antibiotics in combination with adapalene, azelaic acid, or adapalene plus benzoyl peroxide (fixed combination); for severe nodular acne/acne conglobata, systemic antibiotics with azelaic acid.
- Alternatives for female patients are hormonal antiandrogens in combination with topical treatment approaches (only for severe papulopustular/moderate nodular acne) or with systemic antibiotics (for both forms, but low level of recommendation).
Individual therapy options under the microscope
Antibiotics: Among oral antibiotics, second-generation tetracyclines and, in this case, mainly doxycycline and lymecycline are drugs of first choice due to efficacy, safety, and resistance considerations. Therapy should be given for three (at most four) months and at the standard or high dosage [2]. A randomized-controlled trial demonstrated non-inferiority of the combination of doxycycline 200 mg and adapalene/benzoyl peroxide versus oral isotretinoin monotherapy for severe nodular acne (based on a composite safety/efficacy endpoint) [3].
Hormones: pills containing CPA, drospirenone, chlormadinone acetate or dienogest, and spironolactone are considered the first choice. They can be administered for peripheral hyperandrogenism or hyperandrogenemia, but also for acne tarda, refractory acne, desire for oral contraception, or for women requiring systemic isotretinoin administration. The therapy should be carried out for at least 6-12 months [2].
Oral isotretinoin: “Isotretinoin is by far the most effective substance for acne. After one treatment cycle, long-term remissions can be achieved with it in 70-80% of cases,” said the speaker. In Europe, it is approved for severe forms of acne (acne nodularis, acne conglobata, or acne with risk of permanent scarring) that have proven resistant to adequate standard cycles of systemic antibiotics and topical therapy. The starting dose is commonly reported to be 0.5 mg/kgKG/d. “Adequate dosing with this drug is quite crucial for both efficacy and toxicity. Therefore, in my opinion, modifications are also useful here – not least to improve the image of the substance,” Bettoli explained.
A personalized and simple approach for all acne severities that additionally counteracts poor adherence due to side effects/flares is a starting dose of 0.1-0.2 mg/kgKG/d with subsequent increases to the highest tolerable dose. “This approach is also suitable for dealing with generic drugs (different pharmacokinetics). The bottom line is that it can be used to effectively control acne with simultaneously acceptable side effects, shortest possible duration of therapy, and a low recurrence rate [2].”
While continuous or intermittent low dosing also achieves a good efficacy-side effect profile, two other important requirements are not met: The recurrence rate is higher and the duration of therapy is longer [2]. With the high-dose variant, these two points are given, as is the good effectiveness, but the side effects increase. In view of this, the individualized step-by-step approach is recommended, according to the speaker.
Dangers of isotretinoin treatment
Despite the known teratogenicity of isotretinoin and the introduction of strict pregnancy prevention programs (prototypical: iPLEDGE in the USA), there are still few women who become pregnant under the drug. The reasons for this are not easy to pinpoint. In addition to ineffective contraception, insufficient information or poor compliance on the part of the patient are the main reasons. “A problem we also have to face are the electronic pharmacies that offer isotretinoin outside of prevention programs. Patients sometimes receive the teratogenic substance there without a valid prescription and entirely without the associated information material, as a study from 2014 showed,” warned the speaker [4].
There appears to be no association with increased risk of ulcerative colitis with isotretinoin treatment, but the risk of Crohn’s disease is reduced [5]. In some susceptible individuals, literature suggests there is an association between isotretinoin, depression, and suicide. However, it should be noted here that acne per se may be associated with an increased risk of mental health problems and suicidal ideation, and depression or suicide also occurs under antibiotics. According to Bettoli, the current study situation does not allow a conclusive statement. At most, identification of patients who are particularly susceptible to depression with appropriate questions prior to initiation of therapy is useful. There was also little, if any, risk of poorer wound healing with isotretinoin in the large studies [6]. Some studies found no negative effects at all [7].
To what extent can dangerous changes in laboratory values occur with isotretinoin? A meta-analysis has shown that monthly monitoring is not useful for a standard dose and standard patient because, although there were significant changes in certain parameters, these were rarely in the risk range and the overall number of patients with laboratory abnormalities was low [8].
Pigment shifts
Prof. Dr. med. Peter Itin, Chief Physician Dermatology, University Hospital Basel, spoke among other things about melasma. This is an acquired hyperpigmentation exclusively on UV-exposed areas. Women are nine times more likely to be affected than men. In addition to genetic predisposition and UV exposure, sex hormones, thyroid dysfunction, certain cosmetics and medications play a role in the development process.
Three forms can be distinguished: Centrofacial (forehead, cheeks, upper lip, nose, chin), malar (cheeks and nose) and mandibular (lower jaw). By far the most common melasma is on the cheeks and nose. Hyperpigmentation is much less common on the forehead and upper lip, and even less common on the chin and lower jaw. Epidermal forms are intensified under woodlight, dermal forms are not. In addition, there are mixed expressions with only partial amplification in woodlight. Patients with skin type VI, i.e. black skin, are not even considered for this examination method.
For a more precise determination, the Melasma Area and Severity Index (MASI) can be consulted. The face is divided into three areas of 30% each (forehead, right and left cheek up to half of the nose each) and one area of 10% (chin). This is used to determine the extent of the melasma. In addition, the degree of pigmentation and homogeneity are noted.
Prevention is, as so often, adequate sun protection. Bleaching preparations are also used therapeutically. They act either before, during or after melanin synthesis. The first group includes representatives such as tretinoin and tranexamic acid, the second, for example, hydroquinone, azelaic acid, phenolic compounds or ascorbic acid, and the third niacinamide, glycolic acid, retinoic acid or corticosteroids. The gold standard for the treatment of hyperpigmentation is the triple combination of hydroquinone, tretinoin, and topical steroid [9]. Laser therapy is also a possible (but rather late) treatment option for melasma.
Unpleasant travel souvenirs
Prof. Dr. med. Stephan Lautenschlager, Chief Physician at the Dermatological Outpatient Clinic of the Triemli City Hospital, Zurich, gave an overview of unwanted travel souvenirs of the skin. Dermatoses are among the third most common travel-associated diseases after fever and diarrhea.
Schistosomiasis (bilharzia): Schistosomiasis is endemic in over 60 tropical and subtropical countries and may present as “swimmer’s itch,” acute schistosomiasis (Katayama fever), or bilharziosis cutanea tarda. Symptoms of anogenital schistosomiasis include bleeding (postcoital), pain, and pruritus; possible complications include sterility, anemia, or increased risk for HIV infection. Therapy is with praziquantel 40 mg/kg for three days. Follow-up should be done after six, twelve and 24 months (stool, serology).
“Seabather’s eruption”: Seabather’s eruption is a hypersensitivity or toxic reaction to larval toxins (e.g., the thimble jellyfish Linuche unguiculata). In most cases, the larvae become trapped in the bathing costume and release their venom in response to chemical or physical stimuli (drying off or even showering with fresh water). After minutes to 36 hours, a urticarial/papulovesicular rash appears that resolves over the course of one week or a maximum of 14 days. Most patients suffer from pruritus, but systemic symptoms may also occur, most commonly in children. Treatment recommended is initially a vinegar rinse, and later at most topical steroids, oral antihistamines, and (rarely) oral steroids. It is important to thoroughly clean the bathing suit (cave: showering with fresh water is counterproductive for the reasons mentioned).
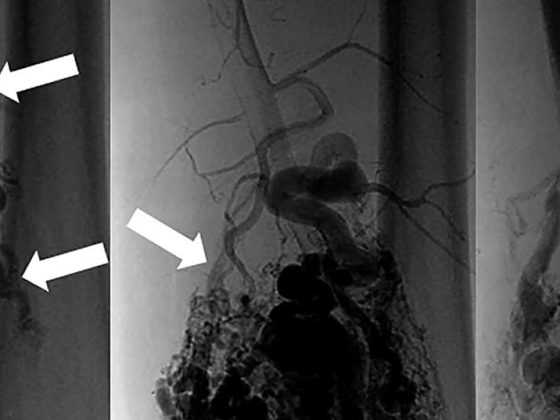
Larva migrans cutanea: Larva migrans is found in the Caribbean, South America, Southeast Asia and Africa. Characterized by tortuous, filiform, elevated, intensely itchy, mobile duct structures that elongate 1 mm to 3 cm per day. Children are affected more often than adults. Most often, the parasitic disease manifests itself on the feet (walking barefoot in larval-containing sand contaminated with cat/dog feces). The disease is self-limiting (two to eight weeks). For example, treatment can be with thiabendazole 10% topically for three to four days (although not approved in Switzerland) – other options include albendazole 400 mg for two to three days and (less commonly used) ivermectin 0.2 mg/kg/d for one to two days. “A tip for prevention: if possible, avoid beaches where there are free-roaming dogs,” advised Prof. Lautenschlager.
Tungiasis: Tungiasis is caused by female chiggers 1 mm in size. These are endemic to South America, the Caribbean and Africa. In regions with poor populations, the prevalence can be as high as 50%. Tungiasis manifests as erythema with intense itching or even pain. The parasite can often already be seen on dermoscopy as a central brown dot surrounded by a bright halo. The disease occurs more frequently on the feet than on the hands and is often accompanied by a superinfection, which must be given special consideration, according to Prof. Lautenschlager. There is no effective drug therapy for tungiasis. The parasite can be removed with a punch/surgical excision. Killing with a topical dimeticone combination of low viscosity also appears to be possible [10]. “As a patient, you’re tempted to just reach for the needle, tweezers or some other sharp object, but that’s not a good idea,” the expert said.
Source: Swiss Derma Day, January 28, 2016, Lucerne
Literature:
- Nast A, et al: European evidence-based (S3) guidelines for the treatment of acne. J Eur Acad Dermatol Venereol 2012 Feb; 26 Suppl 1: 1-29.
- Zouboulis CC, Bettoli V: Management of severe acne. Br J Dermatol. 2015 Jul; 172 Suppl 1: 27-36.
- Tan J, et al: A treatment for severe nodular acne: a randomized investigator-blinded, controlled, noninferiority trial comparing fixed-dose adapalene/benzoyl peroxide plus doxycycline vs. oral isotretinoin. Br J Dermatol 2014 Dec; 171(6): 1508-1516.
- Lagan BM, et al: Assessing the availability of the teratogenic drug isotretinoin outside the pregnancy prevention program: a survey of e-pharmacies. Pharmacoepidemiol Drug Saf 2014 Apr; 23(4): 411-418.
- Racine A, et al: Isotretinoin and risk of inflammatory bowel disease: a French nationwide study. Am J Gastroenterol 2014 Apr; 109(4): 563-569.
- Wootton CI, et al: Should isotretinoin be stopped prior to surgery? A critically appraised topic. Br J Dermatol 2014 Feb; 170(2): 239-244.
- Chandrashekar BS, et al: Safety of performing invasive acne scar treatment and laser hair removal in patients on oral isotretinoin: a retrospective study of 110 patients. Int J Dermatol 2014 Oct; 53(10): 1281-1285.
- Lee YH, et al: Laboratory Monitoring During Isotretinoin Therapy for Acne: A Systematic Review and Meta-analysis. JAMA Dermatol 2016 Jan 1; 152(1): 35-44.
- Bayerl C: Undesirable and desirable pigmentation. Dermatologist 2015 Oct; 66(10): 757-763.
- Thielecke M, et al: Treatment of tungiasis with dimeticone: a proof-of-principle study in rural Kenya. PLoS Negl Trop Dis 2014 Jul 31; 8(7): e3058.
DERMATOLOGIE PRAXIS 2016; 26(2): 44-47