Anyone who, for whatever reason, looks at the list of banned substances in sports will be amazed to find insulin there. For years, this drug – still the gold standard of diabetes treatment, is listed under “Substances and methods prohibited at any time (in and out of competition) S4, Hormones and metabolic modulators 5.2 Insulin and insulin mimetics”. What explains the presence on the doping list of this life-saving drug for 422 million adult diabetics worldwide?
Insulin not only accelerates the uptake of glucose and the formation of the energy store glycogen in the liver and muscle cells, but also acts on protein metabolism with an increase in protein synthesis, through the activation of other anabolic hormones (IGF-1, MGF = mechanical growth factor). Insulin thus belongs in a broader sense to the anabolic and regeneration-promoting doping substances. The hormone is not only popular with musclemen, endurance athletes also appreciate it because it improves aerobic capacity. This can be increased up to twice. To achieve the desired effect, athletes apparently inject insulin and glucose as a mixed infusion. Classic anabolic steroids are often used at the same time. Finding the exact mixing ratio of this power cocktail is a tightrope walk between performance enhancement and hypoglycemic coma and other reactions unfavorable to health (fat storage, edema, visual disturbances, etc.). Insulin as a doping agent has already claimed numerous lives. Contrary to what is often said among users, that detection is not possible because of the physiological properties and short half-life of the hormone, is incorrect: misuse can be detected in the laboratory.
Top sporting performance despite diabetes
However, therapy with insulin is of course possible for competitive athletes with diabetes; it is simply subject to notification with an exceptional authorization for therapeutic purposes (ATZ). Several diabetic very successful top athletes are known, including world champions and Olympic champions, in sports as diverse as figure skating and rowing.
It should be noted that the new anti-diabetes drugs such as the SGLT2 inhibitors, the DPP-4 inhibitors, glinides, glitazones, α-glucosidase inhibitors, and GLP-1 receptor agonists are not on the doping list, nor are the older biguanides and sulfonylureas. For this, the insulin analogues are prohibited both in training and in competition.
There are numerous top athletes with diabetes known at home and abroad, most of them belong to type 1 diabetics. What progress since the 1980s, when this diagnosis was effectively tantamount to a ban on sports! Today, those affected can achieve peak performance thanks to improved monitoring and therapy options. Nevertheless, blood glucose control during exercise remains tricky. It is impressive how certain athletes practice their sport with the insulin pump: In triathlon, for example, with different basal insulin requirements in the individual disciplines, it is programmed to prevent hypoglycemia during the competition. Other athletes wear a sensor for continuous glucose measurement. All are well informed about the insidiousness of the disease, probably the cardinal point of the problem.
Constant increase in type 2 diabetes worldwide
However, the number of competitive athletes among diabetics is vanishingly small. Despite constant development of diabetes research, a constant increase in the incidence and prevalence of this disease is observed worldwide, this is especially true for type 2 diabetes. Today, the number of diabetics worldwide is estimated at 400 million; by 2040, it will be 640 million. According to the WHO, one in six people will soon have diabetes. This means a real pandemic that progresses in parallel with the development of obesity. Type 2 (non-insulin-dependent) is six to ten times more common than insulin-dependent type 1.
In recent years, there have been many changes in the treatment of type 2 diabetes, not least because of new compounds such as the aforementioned SGLT2 inhibitors, the DPP-4 inhibitors, glinides, glitazones, α-glucosidase inhibitors, and GLP-1 receptor agonists. Also available on the market are new forms of insulin. Further, the target values have changed: Instead of a universal HbA1c target, the aim today is to achieve an individual value. Finally, factors such as the patient’s preferences, the physician’s objectives, and other underlying conditions (reimbursement) are considered.
Positively influence the disease
Nevertheless, a change in lifestyle is a basic measure in all therapy stages: Balanced nutrition, supported by regular physical activity (sports), plays the most important role in this context. From a medical point of view, exercise primarily aims to improve metabolic control (glycemia, blood lipids, cholesterol, blood pressure, etc.). This with the aim of reducing the risks for secondary diseases (myocardial infarction, ictus).
At the same time, effects on general well-being and mental health are achieved, which reduces the feeling of illness and negative attitudes towards the disease. As generally recommended, five times 30 minutes of exercise per week is sufficient to positively impact diabetes and health. As physical activity, the professional societies recommend endurance, strength and flexibility training. The combination of strength and endurance sports has proven to be particularly effective for diabetics. Glycemic control improves under both aerobic and strength training. In both types of training, it is important to involve different muscle groups of the entire body. However, it is equally important that the patient receives specific instructions from the doctor. The advice alone to move is hardly enough! Studies have shown that with appropriate training, HbA1C reductions of 0.5 to 0.8 percentage points can be achieved. This is close to the effect of insulin therapy in a similar period.
Observe contraindications
So physical activity is important for type 2 diabetics, but apparently not everyone benefits to the same extent. It is known that up to 20% of diabetics do not improve glucose homeostasis, insulin sensitivity, or mitochondrial density in muscle with exercise. In about 7%, a negative effect can even be demonstrated, such as an increase in resting systolic blood pressure or fasting H DL lowering. Twin studies were used to search for genetic causes of these interindividual differences and indeed found diverse gene loci that influence the metabolic response to exercise. In the future, genetic tests will certainly be used to detect such phenomena.
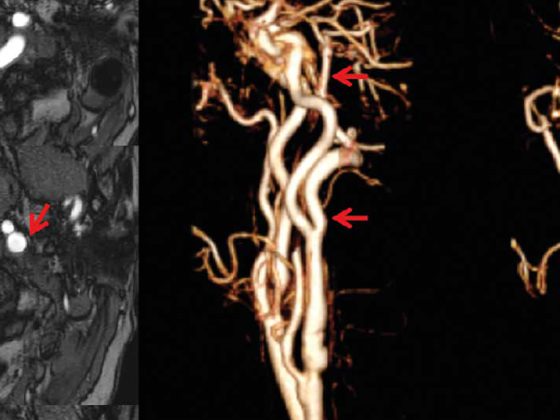
It goes without saying that the basically positive physical activities in diabetes should only be approached after thorough medical clarification. In fact, there are some contraindications to moderate to intense exercise for type 2 diabetics. In any case, progressive proliferative retinopathy prohibits shock loads because of the increase in intraocular pressure. In case of peripheral neuropathy, pay attention to foot health and prefer swimming or cycling. In autonomic neuropathy, the intensity range must be well delineated. And in this situation you should remember that heart rate is not reliable as a measure of exertion.
Diabetes and sport could be understood on the one hand as a therapeutic symbiosis of purpose and on the other hand as a contradiction. In fact, exercise as therapy and prevention is unbeaten in terms of effectiveness, but also non-compliance!