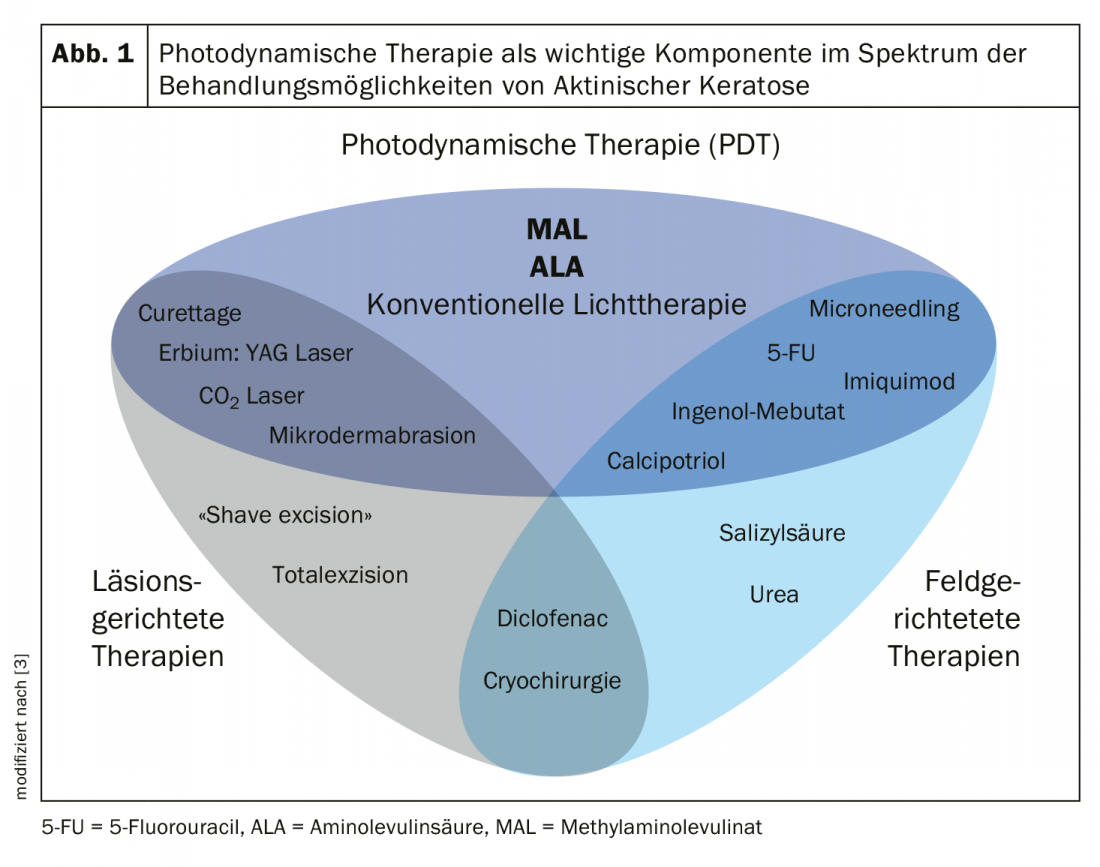
There are numerous methods of intervention for the treatment of actinic keratosis, including lesion- and field-guided approaches. Photodynamic therapy is among the established treatment modalities for these common precancerous lesions of the skin. Several recent studies address the question of how therapy quality and outcomes can still be optimized.
Actinic keratosis is an epithelial carcinoma in situ of the skin that can develop into an invasive squamous cell carcinoma. People with fair skin types who spend a lot of time outdoors are particularly at risk. Photodynamic therapy (PDT) is based on the application of light-sensitizing substances, which selectively accumulate in atypical keratinocytes in the diseased epidermis and are activated by illumination with light of suitable wavelength. In this process, photochemical and physical processes generate reactive oxygen species (ROS), which lead to cell damage and cell death of precancerous changes. In conventional photodynamic therapy, 5-aminolevulinic acid (ALA-PDT) resp. Methyl aminolevulinate (MAL-PDT) applied to the skin. Photoactive ALA is a precursor of the endogenous substance porphyrin and, under the influence of light of a certain wavelength, causes the formation of aggressive oxygen, which contributes to the cell death of diseased cells [1].
Current study findings at a glance
|
Less painful thanks to modified therapy regimen
ALA-PDT is an effective treatment option for actinic keratosis, but some patients experience pain as a side effect during treatment. A clinical trial (n=23) compared a conventional treatment regimen (1 hour pretreatment with ALA followed by blue light irradiation) with a new modified regimen in which blue light irradiation is started immediately after ALA application [2]. A topical formulation of ALA 20% was applied to the entire face and/or scalp. On one side of the body, irradiation with the blue light was started immediately and continued for 30, 45, or 60 minutes (modified PDT). On the contralateral side, blue light started 1 hour after application of ALA and lasted 1000 seconds (conventional PDT). Pain was rated on a scale of 0 to 10. The number of keratotic lesions was determined by clinical examination and photographs. At 3 months after treatment, lesion clearance was almost identical on both sides, as demonstrated by statistical tests in a “noninferiority” design. However, the modified form of PDT, that is, with simultaneous irradiation, resulted in significantly less pain compared with conventional therapy. Regarding the interpretation of the results, it is pointed out that although this was a controlled clinical trial, the subject sample was relatively small.
Combination therapy: the more, the better?
In clinical practice, different interventions are often used in combination to achieve the best possible results. In the current S3 guideline on actinic keratosis and squamous cell carcinoma of the skin, there is a strong consensus-based recommendation to offer a combination of a field-directed with a lesion-directed treatment modality [1]. This is based on the recognition that potential synergistic effects can be achieved by combining different treatment modalities through different mechanisms of action. Combination therapies of a field-directed and an ablative procedure have been shown to be well tolerated in clinical practice [2]. In a publication on this topic published in 2020, the combination of cryosurgery followed by PDT, as well as PDT in combination with topical procedures and PDT with microneedling achieved slightly better results compared to the respective monotherapies. The authors concluded that the use of combination therapies should be assessed individually, taking into account patient- and lesion-specific aspects [3].
Literature:
- Heppt MV, et al: S3 guideline “Actinic keratosis and squamous cell carcinoma of the skin”, abstract, part 1: 4 March 2020, https://onlinelibrary.wiley.com/
- Kaw U, et al: JAAD 2020; 82(4); 862-868.
- Steeb T, et al: JEADV 2020; 34(4): 727-732.
DERMATOLOGY PRACTICE 2020; 30(4): 44