Acupuncture and Chinese medicinal therapy have great potential in integrative oncology. These are therefore supportive measures. They are not intended to replace biomedical cancer therapies, but to complement them.
The use of acupuncture is widespread in integrative oncology. Many of the major cancer centers in the United States offer acupuncture to their patients [1]. Somewhat less common is the use of Chinese medicinal therapy.
In Switzerland, acupuncture and Chinese medicine are generally well established. Thus, for medical acupuncture there is a certificate of competence and the therapy is reimbursed by the basic insurance; non-medical acupuncture is federally regulated and is reimbursed by the supplementary insurance. The Chinese medicines are considered as remedies and are controlled by Swissmedic. The drug mixtures are prepared by specialized pharmacies and delivered to the patients. However, integrative oncology and thus the use of acupuncture and Chinese medicine in cancer patients is not yet widespread in Switzerland.
In oncology, acupuncture and Chinese medicinal therapy are used complementarily. Cancer patients are supported with acupuncture and Chinese medicinal therapy during and after chemotherapy or radiation therapy. The aim is to reduce side effects, improve the quality of life and tolerability of conventional medical therapy, and increase the overall success of treatment. When administering Chinese medicines, possible interactions with conventional medical therapy must be taken into account.
Current evidence
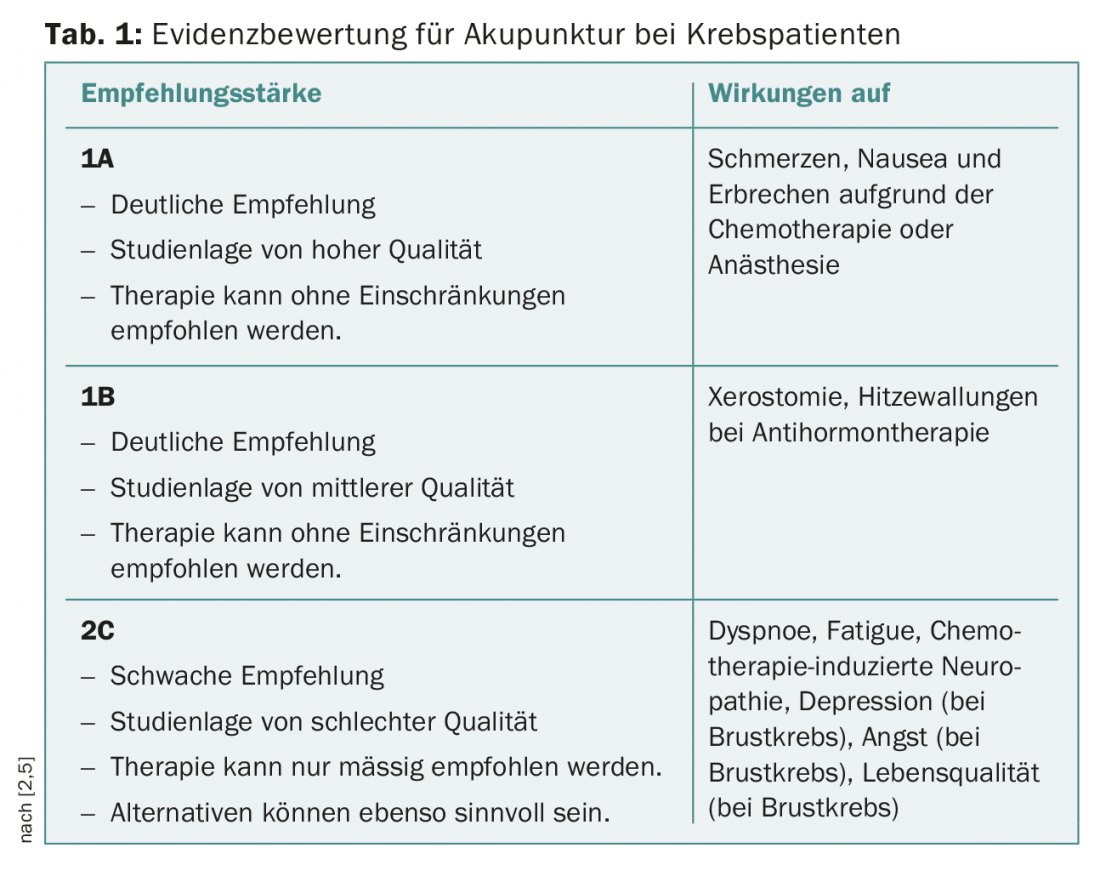
Acupuncture: Comparatively many studies are available on the use of acupuncture in oncological patients. The strength of evidence varies depending on the indication (Tab. 1) . Evidence for the use of acupuncture is available for the treatment of cancer-related pain and for nausea and vomiting secondary to chemotherapy or anesthesia [1,2]. Less clear, but still positive, is the evidence base for a variety of common side effects in cancer patients. Thus, the use of acupuncture may be useful for stiffness and pain due to aromatase inhibitors [1,3], hot flashes secondary to antihormone treatment [1,2], radiotherapy-induced xerostomia [1], dyspnea, fatigue [4], chemotherapy-induced neuropathy [2,5], insomnia [6], and chemotherapy-induced neutropenia [7]. Acupuncture can also be used to help with depression and anxiety that cancer patients experience as part of their disease [5,8]. In addition to the specific symptoms alleviated by acupuncture, patients often report a general positive effect in terms of quality of life and well-being [3,9,10]. Acupuncture can also contribute in a palliative setting because of its effect on improving quality of life [8,11]. The studies cited are for different cancer conditions and it can be expected that the beneficial effects exist regardless of the type of cancer.
Chinese medicinal therapy: In contrast to the West, traditional medicinal therapy is used much more frequently in China than acupuncture [12]. This has an impact on the study situation. A large number of studies on the use of Chinese medicinal therapy in oncological patients come from the Asian region. Similar to acupuncture, the use of Chinese medicinal therapy in chemotherapy or radiation patients is shown to improve the quality of life by reducing side effects [13,14]. Chinese medicinal therapy can also alleviate side effects and improve overall well-being during follow-up treatment with aromatase inhibitors [15].
The effectiveness of Chinese medicinal therapy is sometimes criticized with the argument that chemotherapy is attenuated and therefore its toxicity is reduced. In this regard, it has been shown that when Chinese medicinal therapy and conventional oncological treatment are used simultaneously, there is an improved survival rate in advanced breast cancer [16], gastric cancer [17] or liver cancer [18].
The overall study situation for Chinese medicinal therapy is less certain than for acupuncture, and the reduction of chemotherapy-induced toxicity by Chinese medicinal therapy is not considered proven [19].
Security
Performed by qualified individuals, acupuncture is an extremely safe therapeutic method [2]. In a study of the side effects of acupuncture, no severe side effects and only 43 mild side effects such as nausea, dizziness, bruising, or pain were documented in 34,000 treatments [20]. The studies cited above on oncological use also confirm the safety of acupuncture.
Chinese medicinal therapy has much more potential for discussion regarding safety. If Chinese medicinal therapy is used in parallel with chemotherapy, the question of possible interactions arises. This question cannot be answered conclusively. At this point, some important topics are discussed in an overview.
Phytohormones can be problematic in hormone-sensitive cancers. The focus here is on phytoestrogens in ER-positive breast cancer. For phytohormones, it is difficult to extrapolate data from in vitro studies or animal studies to humans [21]. Further, α- and β-receptors must be distinguished among estrogen receptors. The data situation is correspondingly complex and difficult to interpret. Some Chinese medicines exhibit phytoestrogenic effects [22]. However, when these agents are used within the multi-substance mixtures of Chinese medicinal therapy, the phytoestrogenic effect changes [23]. In addition, due to the prescription of multi-substance mixtures with 8-14 individual substances, the individual dosage of the individual remedies is very low, which also affects the phytohormonal activity. Nevertheless, if there are positive data on phytohormonal effects of individual Chinese medicines, they must not be used.
The second important interaction issue is metabolization. The Chinese drugs can block or induce the P-450 enzyme system. Both have a negative effect on concurrent chemotherapy. Hypericum serves as an example: by activating the P450 3A4 and 2C9 enzyme systems, it lowers plasma levels of the metabolites of irinotecan by 42% [24]. However, this example also illustrates the difference between single-drug extracts (“single-drug” phytotherapy) and the Chinese use of multidrug mixtures. The effect of a multi-substance mixture on individual enzyme systems is much lower. On the one hand, because the dosages of the individual agents are low, and on the other hand, because the different substances have different effects on the enzyme systems.
Practice seems to support this argument. Studies of the pharmacokinetic effects of Chinese drug formulations on docetaxel [25], irinotecan, and 5-FU [26] show no interactions at a pharmacokinetic level. The dosing argument is further supported by studies showing pharmacokinetic interactions between a Chinese drug mixture and 5-FU at very high doses in animal experiments [27].
Also to be taken into account is the load on the liver caused by the administration of Chinese medicines. However, practical experience shows that problems here are very rare. A study just published from Germany reported 26 cases of severely elevated ALT (>5× elevated) in 21 470 patients monitored. Liver values returned to normal after discontinuation of the drugs [28].
The literature regarding interactions is currently insufficient but not negative. In a 2010 review of interactions between Chinese medicines and anticancer drugs, the author concludes that the benefit outweighs the risk [29]. Since then, the literature has tended to support this conclusion.
Practical application
In practical application, acupuncture and Chinese medicinal therapy can be combined or used separately. Due to interaction concerns with Chinese medicines, the threshold for acupuncture therapy is much lower. Acupuncture therapy is associated with minimal risk, is positively evaluated by patients [30] (and experienced as “very important” [31]) and can therefore be offered as a possible complementary therapy [2,32]. When choosing an acupuncturist, it is important to recommend a qualified professional [1,2]. Acupuncture sessions are usually held weekly – throughout the duration of chemotherapy or radiation therapy. The treatments are adapted by qualified acupuncturists to the current individual needs of the patients.
Chinese medicinal therapy is mostly prescribed in Switzerland in the form of dry extracts or, less frequently, as liquid extracts. Dry extracts can also be pressed into tablets. The traditional form of decoction is rather rare due to the complex preparation. Chinese medicines are prescribed as prescriptions. Prescriptions consist of 8-15 individual substances and are usually individually prescribed and precisely adapted to the patient’s problem. If the disease situation changes, the recipe is also adjusted. For this reason, no side effects should occur. Specialists in Chinese medicinal therapy compile individual prescriptions from a base of around 350 individual remedies.
When supporting oncological patients, the Chinese medicines are taken between each chemotherapy day. Usually, no mixture is taken one day before and after chemotherapy. Although this handling is not scientifically proven, it is widely implemented in practice. However, this approach is inconsistent with studies showing an improvement in chemotherapeutic efficacy [33] or a reduction in “multidrug resistance” when Chinese medicines are administered concurrently with chemotherapeutic agents [34].
Take-Home Messages
- Acupuncture and Chinese medicinal therapy have great potential in integrative oncology.
- Communication with the patients is important: These are exclusively supportive treatment options, which are used in addition to and never instead of biomedical cancer therapies.
- Acupuncture is an option for most oncology patients because of its very positive risk-benefit ratio. In Chinese medicinal therapy, the question of possible interactions cannot be answered conclusively. If one wants to exclude the (small) possibility of an interaction, the Chinese medicinal therapy must be renounced.
- In any case, choosing a qualified specialist in acupuncture and/or Chinese medicinal therapy with oncology experience is important.
Literature:
- Zia F, et al: The National Cancer Institute’s Conference on Acupuncture for Symptom Management in Oncology: State of the Science, Evidence, and Research Gaps. Journal of the National Cancer Institute Monographs 2017; 2017(52): lgx005.
- Deng G, et al: Evidence-Based Clinical Practice Guidelines for Integrative Oncology: Complementary Therapies and Botanicals. Journal of the Society for Integrative Oncology 2009; 7(3): 85-120.
- Crew K, et al: Randomized, Blinded, Sham-Controlled Trial of Acupuncture for the Management of Aromatase Inhibitor-Associated Joint Symptoms in Women With Early-Stage Breast Cancer. Journal of Clinical Oncology 2010; 28(7): 1154-1160.
- Cheng CS, et al: Acupuncture for cancer-related fatigue in lung cancer patients: a randomized, double blind, placebo-controlled pilot trial. Supportive Care in Cancer 2017; 25(12): 3807-3814.
- Greenlee H, et al: Clinical Practice Guidelines on the Use of Integrative Therapies as Supportive Care in Patients Treated for Breast Cancer. Journal of the National Cancer Institute Monographs 2014; 2014(50): 346-358.
- Choi TY, et al: Acupuncture for Managing Cancer-Related Insomnia: A Systematic Review of Randomized Clinical Trials. Integrative Cancer Therapies 2017 Jun; 16(2): 135-146.
- Lu W, et al: Recent Advances in Oncology Acupuncture and Safety Considerations in Practice. Current Treatment Option in Oncology 2010; 11(3-4): 141-146.
- Romeo M, et al: Acupuncture to treat the symptoms of patients in a palliative care setting. Explore 2015; 11(5): 357-362.
- Kasymjanova G, et al: The potential role for acupuncture in treating symptoms in patients with lung cancer: an observational longitudinal study. Current Oncology 2013; 20(3): 152-157.
- Glick R, et al: Acupuncture for Cancer-Related Pain: An Open Clinical Trial. Medical Acupuncture 2015; 27(3): 188-193.
- Zhou J, et al: The effect of acupuncture on chemotherapy-associated gastrointestinal symptoms in gastric cancer. Current Oncology 2017; 24(1): e1-e5.
- Liu J, et al: Traditional Chinese Medicine in Cancer Care: a review of case reports published in Chinese literature. Researching Complementary Medicine 2011; 18(5): 257-263.
- Zhong L, et al: The efficacy of Chinese herbal medicine as an adjunctive therapy for colorectal cancer: a systematic review and meta-analysis. Complementary Therapies in Medicine 2012; 20(4): 240-252.
- Zhang M, et al: Chinese medicinal herbs to treat the side-effects of chemotherapy in breast cancer patients. Cochrane Database of Systematic Reviews 2007; (2): CD004921.
- Peng N, et al: Effects of the Chinese medicine Yi Shen Jian Gu granules on aromatase inhibitor-associated musculoskeletal symptoms: A randomized, controlled clinical trial. The Breast 2017 Oct 20; 37: 18-27.
- Lee YW, et al: Adjunctive traditional Chinese medicine therapy improves survival in patients with advanced breast cancer: a population-based study. Cancer 2014; 120(9): 1338-1344.
- Hung KF, et al: Complementary Chinese herbal medicine therapy improves survival of patients with gastric cancer in Taiwan: A nationwide retrospective matched cohort study. Journal of Ethnopharmacology 2017; 199: 168-174.
- Liao YH, et al: Adjunctive traditional Chinese medicine therapy improves survival of liver cancer patients. Liver International 2015 Dec; 35(12): 2595-2602.
- Mok TSK, et al: A double-blind placebo-controlled randomized study of Chinese herbal medicine as complementary therapy for reduction of chemotherapy-induced toxicity. Annals of Oncology 2007; 18(4): 768-774.
- MacPherson H, et al: A Prospective Survey of Adverse Events and Treatment Reactions following 34,000 Consultations with Professional Acupuncturists. Acupuncture in Medicine 2001; 19(2): 93-102.
- Piersen C: Phytooestrogens in Botanical Dietary Supplements: Implications for Cancer. Integrative Cancer Therapies 2003; 2(2): 120-138.
- Wiebrecht A: Safety in Chinese Medicinal Therapy. In: Focks C (ed.): Guide to Chinese Medicine: Fundamentals. 7th ed. Munich: Elsevier 2017; 978-1028.
- Zierau O, et al.: Functions of Danggui Buxue Tang, a Chinese Herbal Decoction Containing Astragali Radix and Angelicae Sinensis Radix, in Uterus and Liver are Both Estrogen Receptor-Dependent and -Independent. Evidence-Based Complementary and Alternative Medicine 2014; 2014: 438531.
- Mathijssen R, et al: Effects of St. John’s Wort on Irinotecan Metabolism. Journal of the National Cancer Institute 2002; 94(16): 1247-1249.
- Cassileth B, et al: Safety and pharmacokinetic trial of docetaxel plus an Astragalus-based herbal formula for non-small cell lung cancer patients. Cancer Chemotherapy and Pharmacology 2009; 65(1): 67-71.
- Kummar S, et al: A Phase I Study of the Chinese Herbal Medicine PHY906 as a Modulator of Irinotecan-based Chemotherapy in Patients with Advanced Colorectal Cancer. Clinical Colorectal Cancer 2011; 10(2): 85-96.
- Chiang MH, et al: Herb-drug pharmacokinetic interaction of a Traditional Chinese Medicine jia-wei-xiao-yao-san with 5-Fluorouracil in the blood and brain of rat using microdialysis. Evidence-Based Complementary and Alternative Medicine 2015; 2015: 729679.
- Melchart D, et al: Herbal Traditional Chinese Medicine and suspected liver injury: A prospective study. World Journal of Hepatology 2017; 9(29): 1141-1157.
- Cheng CW, et al: Evidence-based management of herb-drug interaction in cancer chemotherapy. Explore 2010; 6(5): 324-329.
- Garcia M, et al: Inpatient Acupuncture at a Major Cancer Center. Integrative Cancer Therapies 2016 Dec 1: 1534735416685403.
- Johnstone P, et al: Integration of acupuncture into the oncology clinic. Palliative Medicine 2002; 16(3): 235-239.
- Kilian-Kita A, et al: Acupuncture: could it become everyday practice in oncology? Contemporary Oncology 2016; 20(2): 119-123.
- Tan W, et al: Anti-cancer natural products isolated from Chinese medicinal herbs. Chinese Medicine 2011; 6(1): 27.
- Chai S, et al: Circumvention of multi-drug resistance of cancer cells by Chinese herbal medicines. Chinese Medicine 2010; 5: 26.
InFo ONCOLOGY & HEMATOLOGY 2018; 6(1): 23-26.