Pneumococcal pneumonia significantly increases the risk of myocardial infarction; as late as four weeks after pneumonia, cardiac biomarkers remain detectably elevated. Vaccination against Streptococcus pneumoniae even in adulthood is therefore useful especially, but not only, for patients with underlying pneumological and cardiovascular diseases.
At the beginning of the 20th century, Central Europe had a high birth rate and an average life expectancy of 60-65 years. Due to high infant mortality, the focus at the time was on vaccinating children. In the 21st century, this has changed significantly: There is now a high proportion of older people in the population and an average life expectancy of 80 to as much as 85 years. Demographic change therefore requires an adjustment of vaccination programs. This is because immunocompetence, while generally good in adults, declines steadily with age. Conversely, with poorer immunocompetence, susceptibility to infection and risk of disease increase in people over 60.
Modes of action of PCV13 and PPV23
Pneumococci are estimated to cause more than 1000 serious illnesses (meningitis or blood poisoning) each year in Switzerland, 70 of them in children under 5 years of age. In addition, there are more than 1600 pneumonias and 1 to 3 deaths before the age of 5 years [1]. Pneumococcal disease (IPE) is also dangerous for people with chronic diseases such as cardiopulmonary disease, diabetes, renal insufficiency, and HIV infection, among others.
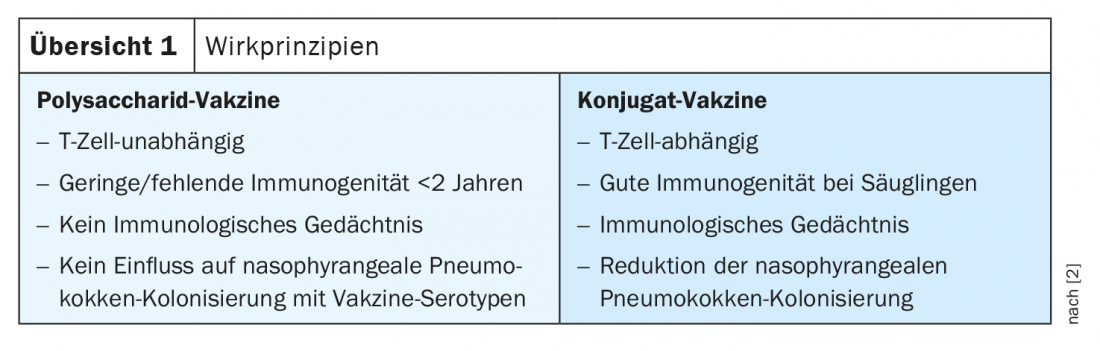
The 13-valent conjugate vaccine (PCV13) and the 23-valent polysaccharide vaccine (PPV23) are available for vaccination against Streptococcus pneumoniae . In PPV vaccination, the polysaccharide antigens of the vaccine bind to the B cell. As a plasma cell, the B cell can then produce type-specific antibodies against the serotypes contained in the vaccine, explained Prof. Dr. Thomas Weinke, Clinic for Gastroenterology and Infectiology at the Ernst von Bergmann Hospital, Potsdam (D) [2]. Thus, the polysaccharide vaccine is T-cell-independent and thus has no immunologic memory and no effect on nasopharyngeal pneumococcal colonization with vaccine serotypes (review 1) .
For conjugate vaccines, this immunological process is more complex. Again, the polysaccharide binds to the B cell, which then produces antibodies. In addition, however, the B cell also interacts with the T cell, inducing immunological memory as well.
Switzerland prefers vaccination with PCV13
In Germany, the Standing Committee on Vaccination (STIKO) recommends vaccinating all children from the age of two months against pneumococci due to the high risk of infection, the frequent complications and the relatively high risk of permanent sequelae, especially for infants and young children. PCV13 is usually used here. In contrast, chronically ill patients and those over 60 years of age are treated only with PPV23 unless they have an immunodeficiency or an increased risk of meningitis. If so, vaccination is done first with PCV13 and 6-12 months later with PPV23.
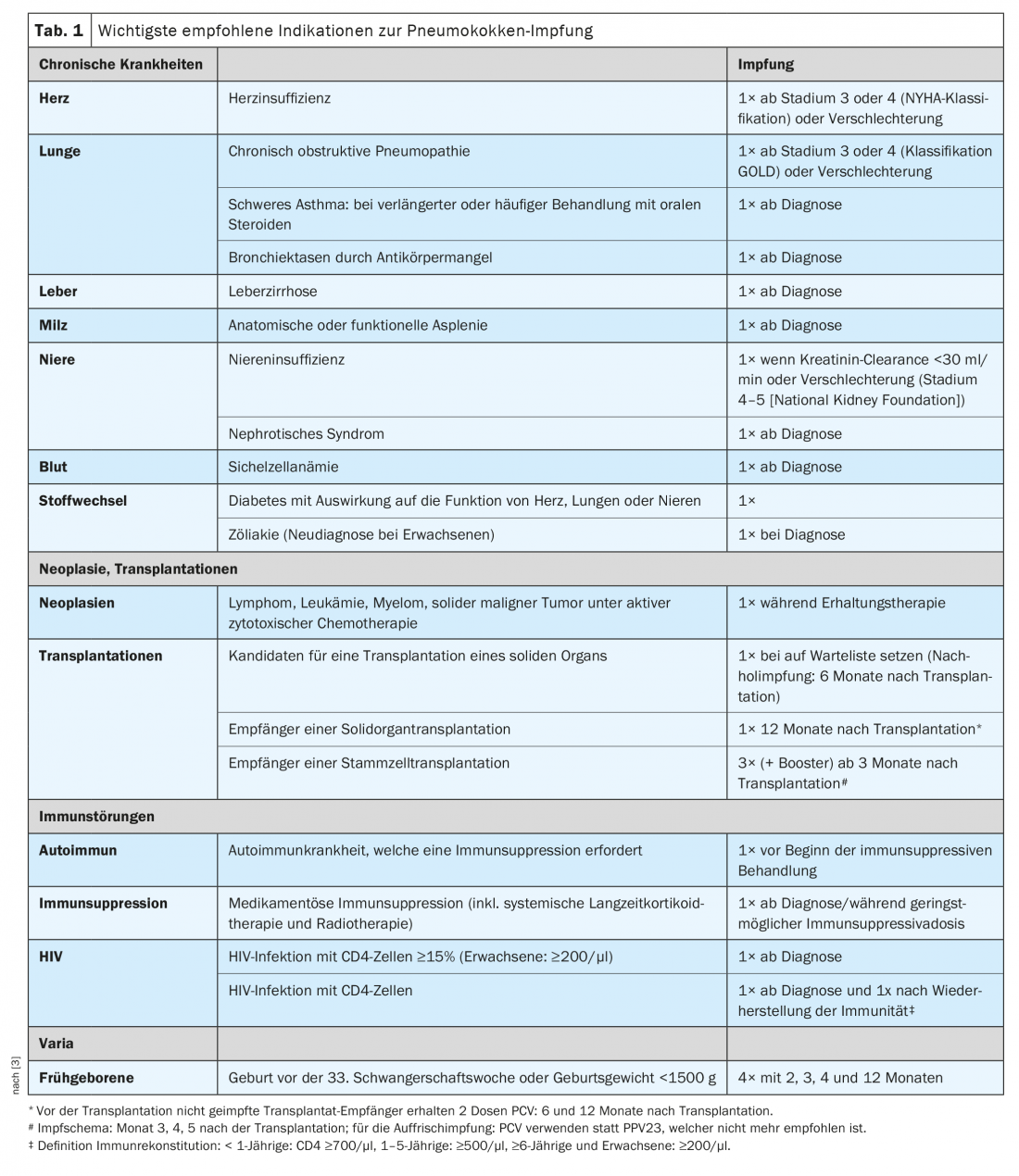
The Swiss Federal Commission on Immunization (EKIF) and the Federal Office of Public Health (FOPH) currently consider vaccination with a conjugated pneumococcal vaccine to be the best choice for prevention of invasive IPE in all persons at increased risk, regardless of age (≥2 months). The conjugated pneumococcal vaccine has a very high efficacy of >95%. In 2020, the Swiss Vaccination Plan made an amendment to the risk groups: Accordingly, a single dose of PCV13 is now recommended for adults diagnosed with celiac disease (Tab. 1) . This is intended to protect against the increased risk of invasive pneumococcal infections due to celiac disease-induced hyposplenia or functional asplenia.
In addition, vaccination not only against pneumococci, but also against influenza, for example, has further positive effects for chronically ill patients, such as heart or lung patients. Among other things, this reduces antibiotic consumption, decreases resistance and has positive side effects for the cardiovascular system.
No booster vaccinations recommended
Based on the current serotype distribution of IPE in Switzerland, no booster vaccinations or additional vaccinations with PPV23 are currently recommended. If a person was recently vaccinated with PPV23 (which is no longer recommended in Switzerland since 2014), the Swiss vaccination schedule states that a minimum interval of 12 months must be observed before PCV vaccination to obtain an optimal immune response to PCV. PCV booster vaccination is not recommended for the time being due to pending data [3]. If IPE occurs in PCV vaccinated individuals, serotype-specific antibody titers should be determined individually to clarify seroprotection and the need for any booster vaccination.
Literature:
- infovac.ch; www.infovac.ch/de/impfunge/nach-krankheiten-geordnet/pneumokokken; last accessed 11.06.2022.
- FomF WebUp: “Preventing respiratory infections caused by pneumococcus in adults,” 6/04/2022.
- Federal Office of Public Health: Swiss Vaccination Plan 2022; as of January 2022; www.bag.admin.ch/bag/de/home/gesund-leben/gesundheitsfoerderung-und-praevention/impfungen-prophylaxe/schweizerischer-impfplan.html.
HAUSARZT PRAXIS 2022; 17(6): 28-29