Psychiatric patients are also hospitalized for somatic disorders, and conversely, patients with primarily somatic disorders often require therapy with psychotropic drugs. Management of affected patients can be aided by good collaboration of psychiatrists with general practitioners and specialists from other disciplines. This topic was the focus of the 12th Annual Meeting of the Swiss Society for Drug Safety in Psychiatry (SGAMSP) on October 2, 2014. More than 120 participants took part in the discussion at the University Hospital Zurich.
Patients who receive therapy with psychotropic drugs often also suffer from chronic or acute somatic illnesses. If these are also treated with medication, it is not uncommon for polypharmacy to occur, with effects and side effects that are difficult to manage. In particular, there are a number of combinations with risks that require special controls or that must be explicitly avoided.
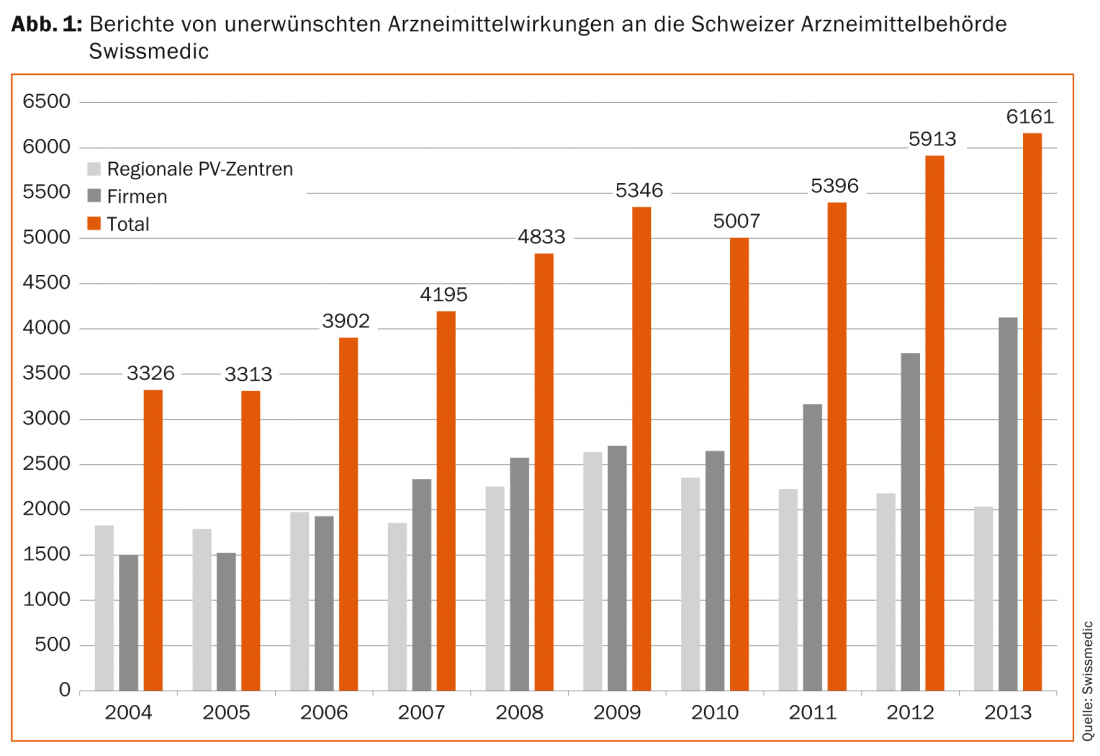
However, it is very difficult, if not impossible, for specialists of all specialties to be sufficiently familiar with the specifics of pharmacotherapy from other specialties, with their numerous interaction risks and the necessary controls. Therefore, in the case of psychiatric patients, the exchange of information between psychiatrists and general practitioners and other specialists is of particular importance. All physicians are also required to report suspected cases of adverse drug reactions to the relevant drug authorities. In Switzerland, this is done through a very well established pharmacovigilance system (Fig. 1), which is actively supported by SGAMSP. In addition, however, physicians should look at innovative ways that electronic prescribing can increase drug safety. Such systems help to identify potential pharmacotherapy problems, assess their clinical relevance, and provide timely warnings of critical situations.
Psychiatry and general medicine
If a psychiatric clinic is part of a general medical hospital, there are a priori good conditions for close interdisciplinary cooperation. Prof. Dr. med. Josef Jenewein from the Department of Psychiatry at the University Hospital of Zurich reported that the prevalence of mental disorders among inpatients in “normal” hospitals is estimated at about 25-60%. These disorders are distributed in roughly similar proportions among depression, addictive disorders, and psychoorganic disorders. Psychiatrists, on the one hand, can provide an “outside” consultation service to other hospitals. In addition, however, psychiatry can act as part of a fully integrated multidisciplinary team in a liaison capacity when needed. Interventions can then affect not only the patients, but also the treatment team in special cases. In each case, interdisciplinary collaboration involves sharing and expanding expertise on the effects, side effects, and interactions of interdisciplinary pharmacotherapy between psychiatrists and other physicians – to the benefit of all involved.
Consultative inquiries often concern delirium and depression
Delirium deserves special attention. Especially in the case of pre-existing dementia, it is often a typical complication when patients are admitted for somatic diseases. In about one third of all cases, delirium is not recognized as such. Prof. Jenewein referred in particular to benzodiazepines, a common and often easily preventable risk factor. In the best case, antipsychotics for delirium treatment, which are susceptible to interactions with other medications, need not be used at all. In alcohol withdrawal delirium, however, benzodiazepines are successfully used for treatment.
Depression is also a very common reason for psychiatric pharmacotherapy in somatic patients. New here is the possible use of psychostimulants such as methylphenidate or modafinil in special cases, e.g. in oncological patients. However, special attention must be paid to interactions and adverse effects.
Cardiac risks of psychopharmacotherapy
Cardiovascular disease is one of the leading causes of death in the Western world. At the same time, cardiovascular disease has a striking association with both psychiatric diagnoses and their pharmacotherapy. In this context, Alice Walder, MD, presented data from the AMSP project, because there, too, it is noticeable that among the side effects occurring under psychotropic drugs, the proportion of cardiovascular events is particularly high at almost 10%.
In clinical practice, two risk constellations in particular must be anticipated and intensively monitored. First, virtually all antipsychotics and also most antidepressants including citalopram are known to prolong QT time, increasing the risk of torsade de pointes tachycardia and sudden cardiac death (Fig. 2) .
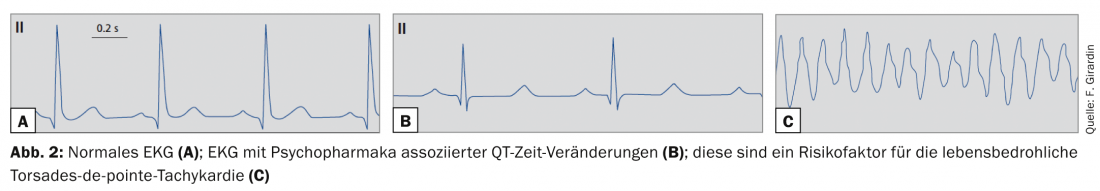
In a somatic hospital setting, dangerous interactions can typically occur with numerous other drugs that also prolong QT time. These include, in particular, the antibiotics clarithromycin, moxifloxacin, and co-trimoxazole, the potent antiemetic ondansetron, and methadone. Essential preventive measures here are to avoid combining several QT-prolonging drugs (interaction check, e.g. at www.mediq.ch) and to check the ECG regularly.
The second typical problem is the metabolic syndrome associated with antipsychotics, a risk factor for ischemic cardio- and also cerebrovascular events. Close monitoring of metabolic parameters, including baseline values, prior to initiation of therapy is therefore recommended. In the case of elevated values, appropriate measures can then be initiated after a careful risk-benefit assessment: a change in therapy of the antipsychotics, programs to improve diet and physical activity, and finally also an additional reduction of blood pressure, cholesterol and blood sugar with medication.
Two new studies on cardiac risks
The cardiac risks associated with the administration of antipsychotics were discussed more intensively in an interactive workshop; the workshop was led by Prof. Waldemar Greil, MD, Sanatorium Kilchberg and Ludwig Maximilian University, Munich, and François Girardin, MD, University Hospital, Geneva. Prof. Greil pointed to a new AMSP study that found about 200 cases of severe cardiovascular side effects in about 160,000 prescriptions of antidepressants. Among tricyclic antidepressants, cardiac adverse events were reported about twice as frequently, at 0.15% compared with 0.08% for SSRIs [1].
Dr. Girardin presented his recently published work with 6790 psychiatric patients [2]. He found that the risk for arrhythmias while taking antipsychotics is increased, especially in patients with hypokalemia, preexisting T-wave changes in the ECG, and HCV and HIV infection. In clinical practice, therefore, particularly good monitoring is required when these risk factors are present.
New methods of therapy monitoring
Systematic analyses and clinical information systems can make an important contribution to identifying dangerous or even contraindicated drug combinations and warning about them in good time. As a clinical pharmacologist and epidemiologist, PD Dr. med. Stefan Russmann is working on this topic at the University Hospital Zurich. With his research group, he has built up a local database of about 7 million prescriptions over the past few years. Through the “interventional pharmacoepidemiology” program he developed, medication errors in a hospital can be identified, quantified and their clinical relevance evaluated within a very short time (Fig. 3). The knowledge gained can then be used to integrate targeted automated alerts into electronic drug prescribing.
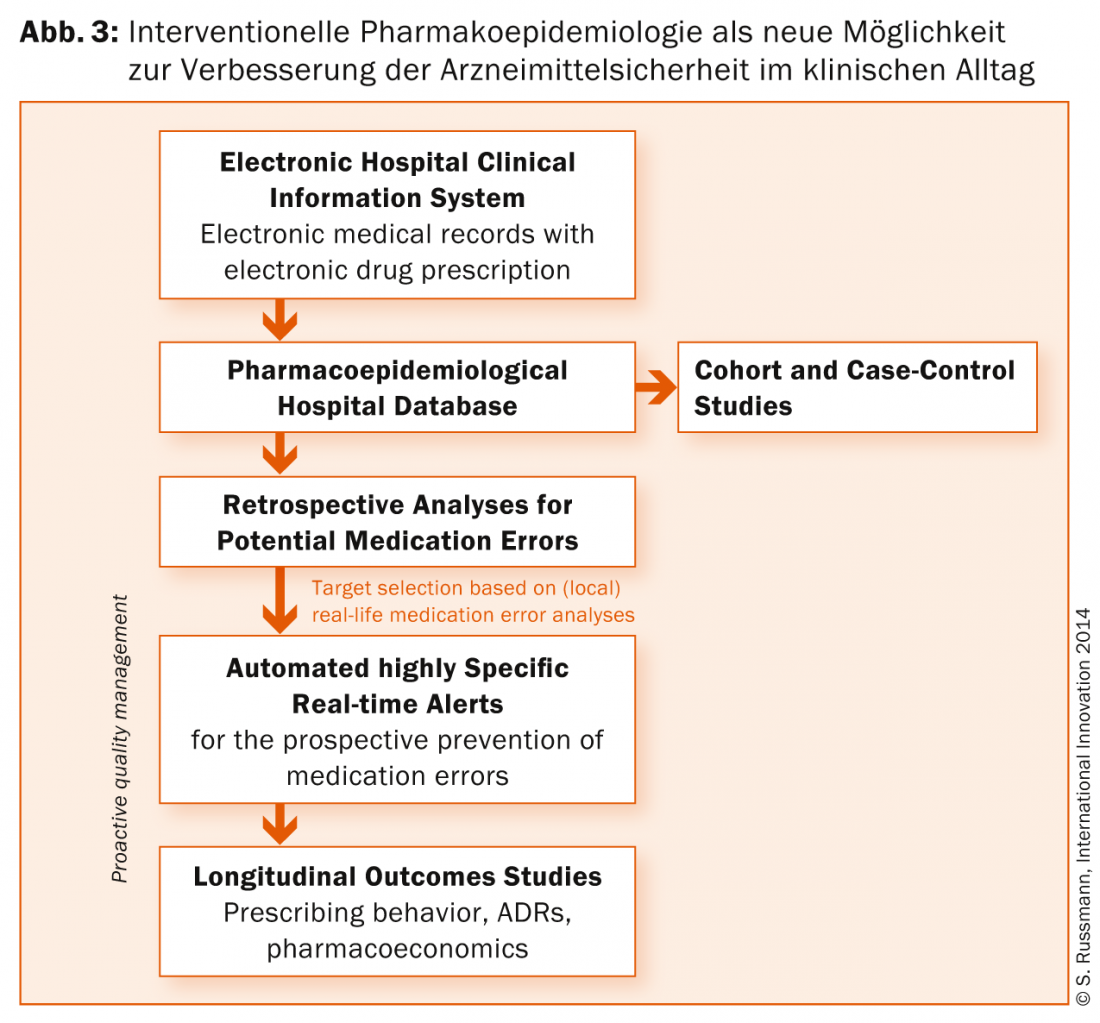
In psychiatry, it has been shown that particularly with clozapine, fluvoxamine and lithium, but also with the antiarrhythmic drug amiodarone, dangerous combinations with other drugs occur particularly frequently [3]. However, the most serious medication errors can be effectively and efficiently prevented in the future with appropriate algorithms. Highly specific alerts should then be displayed at the time of drug prescription. This requires an electronic patient file, which is currently becoming the international standard anyway.
Interdisciplinary collaboration using the example of chronic pain disorders
Dr. med. Esther Hindermann from the Barmelweid Clinic used the example of the management of chronic pain disorders to address the typical problems of polypharmacy and the need for interdisciplinary collaboration. About 20% of the European population is plagued by chronic, non-tumor related pain. Early initiation of collaboration is very important to counteract chronification. Fortunately, there is now an increasing range of multimodal programs whose effectiveness is well documented scientifically. Patients with opioid use in particular can receive close multidisciplinary care.
Common errors can be avoided through competent, highly specialized care, and the risk of uncontrolled analgesic abuse is contained. Means to achieve this include choosing sustained-release opioids, avoiding drop forms, strict dose caps, and proactively addressing adverse effects. From the somatic and psychological-psychiatric side, work is done simultaneously to uncover causes and bring about behavioral changes. In this way, the use of painkillers can be reduced in the medium term and, in the best case, even stopped altogether.
Risks and efficacy profiles of new psychotropic drugs
PD Dr. med. Daniel Schüpbach, Psychiatric University Hospital Zurich, reported on new psychotropic drugs. Research related to future antipsychotics continues to focus on antidopaminergic mechanisms of action. The “wish list” for the properties of new antipsychotics still resembles the squaring of the circle: optimal efficacy, usable in various indications, few undesirable effects and acceptable costs should be combined in one preparation. Dr. Schüpbach presented data from the highly regarded meta-analysis comparing antipsychotics published in the Lancet in 2013 [4]. It is striking that the good efficacy of clozapine is also emphasized here.
At the same time, Dr. Girardin reported that the importance of the risk of agranulocytosis in comparison may be historically rather than rationally thought to be so high [5]. There is evidence that the risk is no higher than with olanzapine, for example. The risk-benefit balance of blood count checks under clozapine is now increasingly questioned, and these are now recommended only every three months in the Netherlands, for example. In contrast, the importance of the high risk for metabolic adverse effects with clozapine may be rather underestimated.
Psychotropic drugs as “lifestyle drugs”?
New antipsychotics such as aripiprazole and lurasidone turn out to be much more beneficial in terms of metabolic effects. However, their perception as better tolerated antipsychotics may also contribute to an indication expansion up to the questionable use as “lifestyle drugs”. Aripiprazole is already one of the top-selling drugs worldwide, and modafinil is also frequently taken without psychiatric indication to enhance performance. Thus, the use of new psychotropic drugs is likely to become an issue of increasing importance to psychiatrists, general practitioners, epidemiologists, and health care payers.
Literature:
- Spindelegger C, et al: Int J Neuropsychopharmacology 2014, online first.
- Girardin F, et al: Am J Psychiatry 2013; 170(2): 1468-1476.
- Haueis P, et al: Clin Pharmacol Ther 2011; 90(4): 588-596.
- Leucht S, et al: Lancet 2013; 382: 951-962.
- Girardin F, et al: Lancet Psychiatry 2014; 1: 55-62.
InFo NEUROLOGY & PSYCHIATRY 2015; 13(1): 35-38.