Diabetic foot is rather rarely the reason for a consultation with a dermatologist. However, the diabetic may complain of dry or cracked, hyperkeratotic skin on the feet. In the following, our author describes how you should proceed in this case.
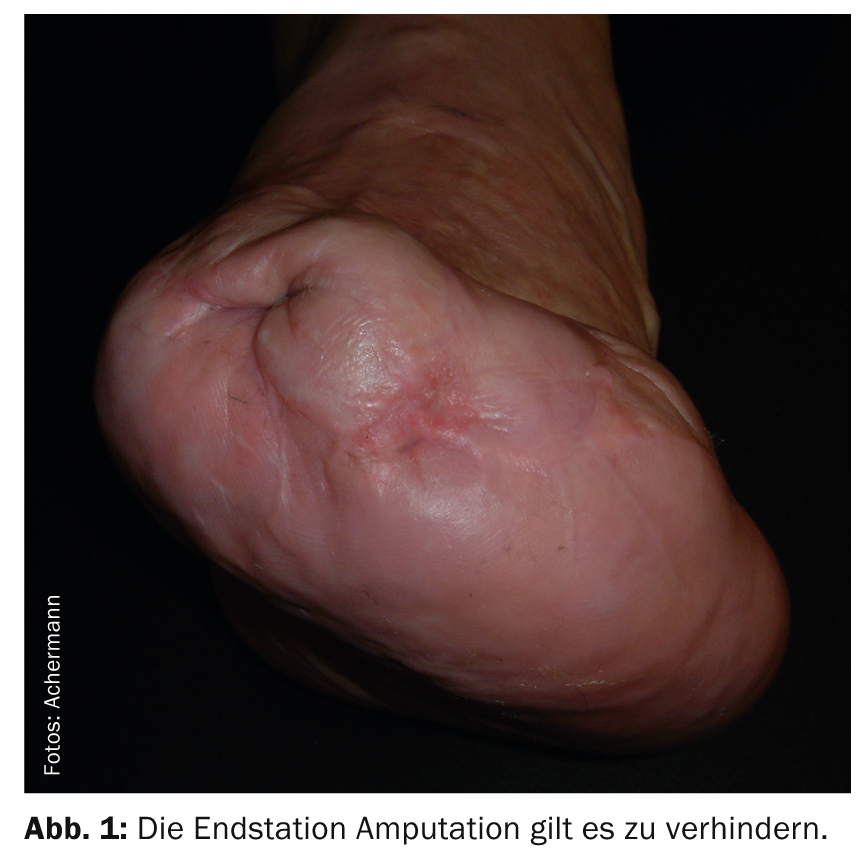
Diabetic foot syndrome with ulcer is the endpoint of many years of neglect on the part of both the sufferer and the care team. An amputation (Fig. 1) is very expensive for the health insurance companies. Training in prophylaxis and early detection can prevent diabetic ulcer and thus much suffering, disability and cost in time.
When a diabetic presents to your practice with dermatological problems, you should therefore take a detailed medical history to set the course and, if necessary, refer the patient to a diabetologist or a diabetic foot consultation.
Is the foot at risk?
In principle, it can be said that if a wound, local redness, blister or ulcer is present in a diabetic patient, there is a diabetic foot with all possible complications. However, even if your patient can answer “yes” to the following questions, the foot is at risk:
- Has the diabetes been present for more than 10 years?
- Are there any circulatory problems?
- Are neuropathic disorders present?
- Are there any incorrect loads?
You should always check for yourself and not just ask if you suspect diabetic foot syndrome (Fig. 2) .
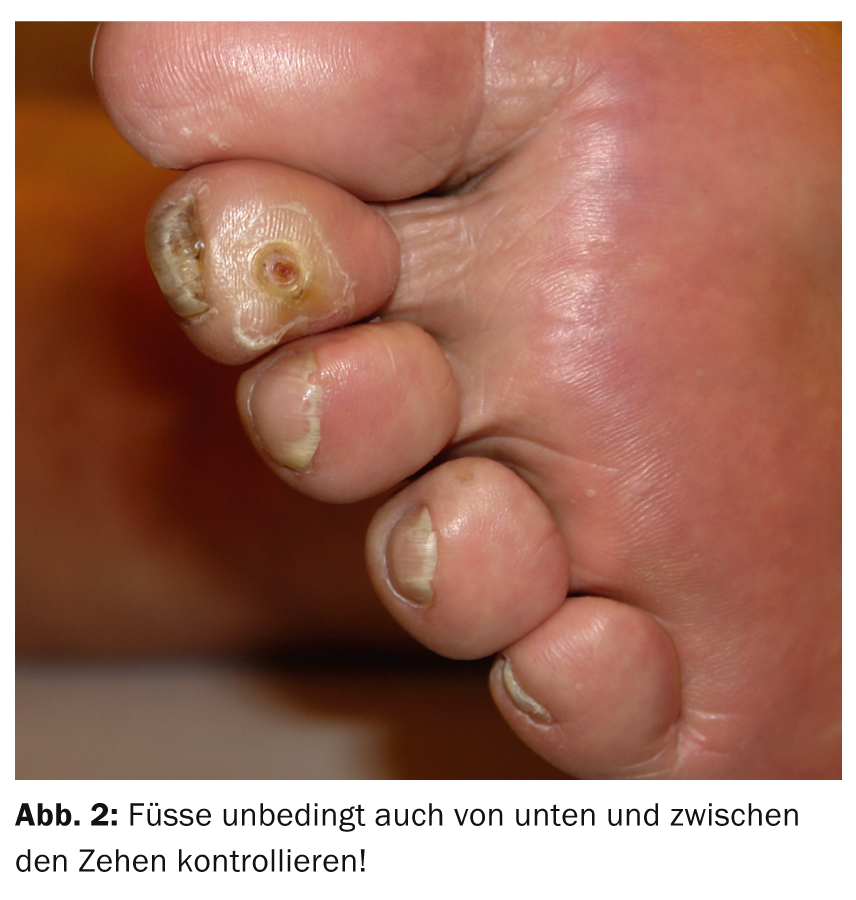
The affected person feels nothing (neuropathy) (Fig. 3) or sees nothing (retinopathy, limited mobility).

Circulatory and neuropathic disorders are briefly discussed below.
Circulatory disorders
Decreased arterial blood flow has the following clinical signs:
- Lack of hair growth on the toes dorsal
- Missing pulses Aa. tibialis posterior/Aa. dorsalis pedis
The blood circulation of the foot must be clarified angiologically in the case of a lesion.
Special attention should be paid to a possible clinical misinterpretation in mediasclerosis (no pulses perceptible). This situation is not clinically assessable. Furthermore, avoid misdiagnosis due to arteriovenous shunts in the foot caused by autonomic denervation. This results in pale skin in the forefoot, but rather warm, reddish skin and venous filling in the midfoot. There is danger here.
Neuropathic disorders
Painful neuropathy usually leads to consultation because of the discomfort. Because of this pain, the reduction in sensitivity is often misjudged (because of the pain, it is thought that there is normal sensitivity) – the foot is very much at risk for the development of an ulcer!
There are three relevant forms of neuropathy: distal symmetric sensory neuropathy, autonomic neuropathy, and motor neuropathy.
Symmetric sensory neuropathy is silent. The affected person feels nothing and the examiner sees nothing! The person concerned must therefore be actively informed of the risk and of the need for regular checks by third parties.
Autonomic neuropathy is manifested by very dry skin. Sympathetic denervation may lead to misjudgment of skin blood flow to the feet. Erectile dysfunction is almost always present as well.
Motor neuropathy leads to paresis and atrophy of the foot muscles. Disturbances of the foot architecture with reduced mobility in the joints and incorrect loading are the consequences.
Clinically, pressure calluses, lack of complaining when changes are visible, and lesions at pressure-loaded sites are clues that must be taken seriously.
Temperature discrimination (Neurotherm), epicritical sensitivity (Spitzrad pointed/blunt sensation), and vibration sense (Riedel Seiffer’s tuning fork) can be examined, as well as touch perception with a 10-g monofilament. A decrease in sensitivity means danger. Close follow-up examinations are therefore recommended, as well as the wearing of appropriate shoes with adapted insoles to relieve pressure in vulnerable areas.
Therapeutic consequences
The first therapeutic consequence when you detect a risk to the foot in a person with diabetes is to educate the patient. The partner should be involved. The regular foot control by the partner is necessary, because mostly a retinopathy exists and the self-control of the sole of the foot is often no longer possible. Furthermore, prophylactic measures should be initiated. This includes referral to a diabetic team or diabetic foot consultation, control or prescription of appropriate footwear/insoles and skin care (possibly Ablation of hyperkeratoses, the rehabilitation of heel rhagades, Fig. 4).

Incidentally, a healed ulcer does not mean that the diabetic foot syndrome has healed. It stays! (Fig. 5)

The follow-up checks remain. A diabetes affected person with diabetic foot syndrome unfortunately often does not change his/her neglect behavior, she/he has no pain! Metabolism should be optimized by insulin therapy and concomitant diseases (high blood pressure, renal insufficiency, PAVK, CHD, heart failure) must be treated as well.
Frank Achermann, MD
CONCLUSION FOR PRACTICE
- If a diabetic patient has a wound, local redness, blister or ulcer, there is a diabetic foot with all possible complications.
- As a basic principle, always check for yourself and don’t just ask.
- The blood supply to the foot must be clarified angiologically in the event of a lesion.
- Distal symmetric sensory neuropathy, autonomic neuropathy, and motor neuropathy are relevant to foot hazards.
- A healed ulcer does not mean that the diabetic foot syndrome has healed.
HAUSARZT PRAXIS 2014; 9(7): 18-20