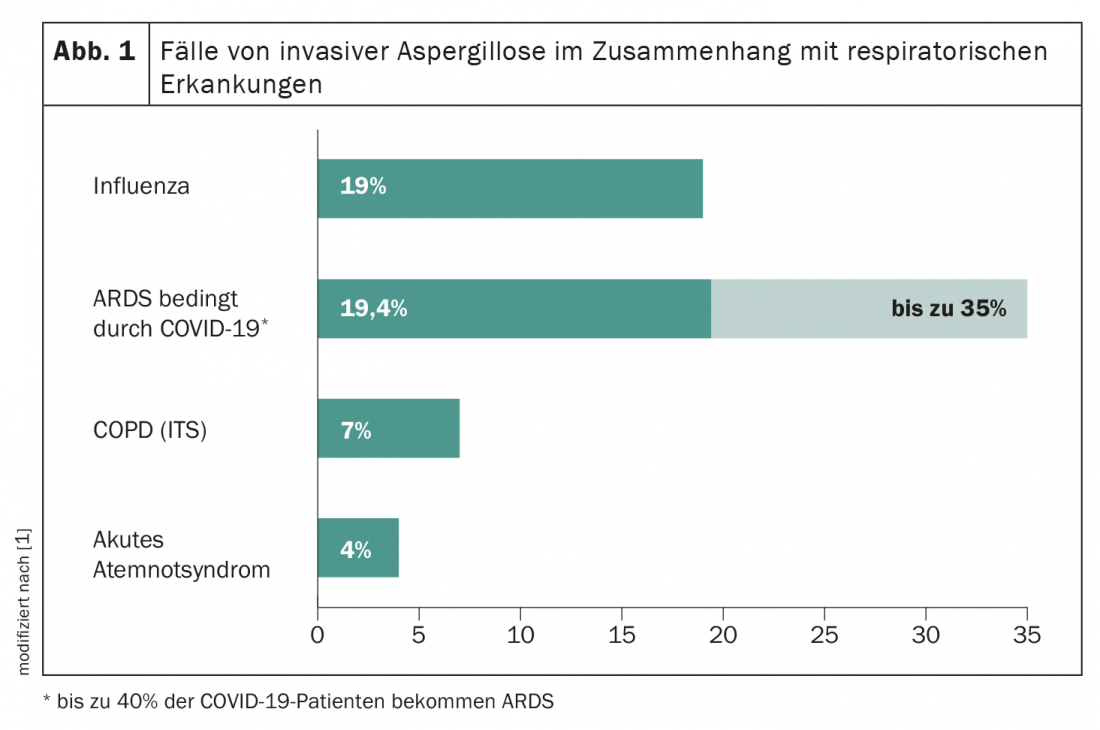
Corona is not alone in having respiratory problems. Invasive pulmonary aspergillosis may also be clustered – usually very rapidly. Therefore, increased attention to this clinical picture is required, especially in COVID-19 patients with ARDS, in order to be able to take appropriate measures regarding diagnosis and therapy at an early stage.
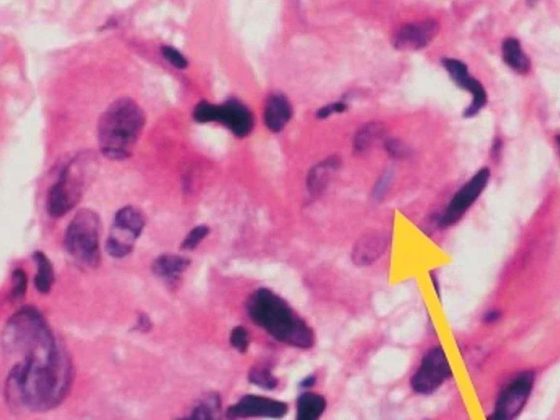
Recent studies suggest that 35% of corona patients with Acute Respiratory Distress Syndrome (ARDS) develop COVID-19 associated invasive pulmonary aspergillosis (CAPA). Deciphering the complex pathogenesis of CAPA requires a molecular understanding of the physiological processes by which infection with SARS-CoV-2 facilitates fungal pathogenesis. Similar to other SARS coronaviruses, SARS-CoV-2 attacks and invades epithelial cells and type II pneumocytes by binding the SARS spike protein to angiotensin-converting enzyme-2 (ACE2) receptors. Cleavage of the S1/S2 domain by the type 2 transmembrane protease TMPRSS2 leads to activation of the spike protein, facilitating entry of the virus into the target cell via ACE2. In addition to its role as a SARS virus receptor, ACE2 has also been shown to be required for protection against severe acute lung injury in ARDS. This is supported by an insertion/deletion polymorphism that affects ACE activity and is associated with susceptibility to ARDS and its outcome. Whether the preceding interaction of SARS-CoV-2 with host cells contributes to the development of CAPA by disrupting the regulation of the renin-angiotensin system and/or the kallikrein-kinin system is unknown.
The release of hazard-associated molecular patterns during severe COVID-19 infection results in both lung epithelial damage and inflammatory disease, which are predisposing risk factors for pulmonary aspergillosis. Moreover, collateral effects of host recognition pathways required for activation of antiviral immunity may paradoxically contribute to a highly permissive inflammatory environment that favors fungal pathogenesis.
Do not take CAPA lightly
Risk factors that may promote CAPA include age, male sex, hypertension, acute or chronic renal failure, COPD, and use of β-lactamase inhibitors or corticosteroids. Most often, Aspergillus co-infection occurs in the first four days after COVID-19 diagnosis. Therefore, diagnostic measures for invasive aspergillosis should be initiated in critically ill patients with progressive disease. But diagnosing CAPA remains difficult. Most importantly, because galactomannan examination of bronchoalveolar lavage fluid and culture, which are the most sensitive diagnostic tests for aspergillosis in the ICU, are hampered by the fact that bronchoscopies are rarely performed in COVID-19 patients because of the risk of disease transmission. Autopsies are also rarely performed, which may lead to an underestimation of the prevalence of CAPA.
Effective therapy management desired
Although it is currently unknown whether antifungal treatment of COVID-19-associated CAPA results in a survival benefit, diagnosis should trigger early antifungal treatment in most cases. However, this is not always easy due to possible drug interactions. The use of voriconazole in particular may be limited. Because it is metabolized via CYP2C19, CYP2C9, and CYP3A4, it is among the drugs most commonly associated with major drug interactions in the ICU. Isavuconazole and liposomal amphotericin B have been shown to be the most important alternatives. Compared with voriconazole, isavuconazole has a more favorable pharmacokinetic profile and is associated with fewer toxicities. Liposomal amphotericin B is a largely effective alternative treatment option, but in the ICU, renal insufficiency often complicates initiation or requires discontinuation of this antifungal agent. This is especially true for patients infected with SARS-CoV-2, which exhibits renal tropism and has been described as a common cause of renal damage. Echinocandins could be used for combination therapy. They are not considered first-line treatment options for invasive aspergillosis due to their limited antifungal activity against Aspergillus spp. but are generally well tolerated and show synergistic interaction with other antifungal agents.
Literature:
- Arastehfar A, Carvalho A, van de Veerdonk FL, et al: COVID-19 Associated Pulmonary Aspergillosis (CAPA) -From Immunology to Treatment. J Fungi 2020; 6(2): 91.
InFo ONCOLOGY & HEMATOLOGY 2022; 10(2): 16.