Pregnancy and childbirth are causative factors in 50% of urinary incontinence and 75% of genital descent. Preventively, physical therapy, lifestyle modifications, perineal massage, and warm compresses can help during childbirth.
In addition to descensus genitalis, urinary and fecal incontinence are also classified as pelvic floor disorders. The main forms of urinary incontinence are stress urinary incontinence and overactive bladder (OAB). In fecal incontinence, a distinction is made between fecal (loss of liquid/solid stool) and anal (also involuntary leakage of wind) incontinence.
In the United States, outpatient costs for all these pelvic floor disorders are estimated at $300,000,000 per year [1], with the lion’s share going to the incontinence materials most often required. How exceedingly common such health problems are is very graphically described by a lifetime risk of 11-19% of having to undergo surgery for prolapse or urinary incontinence at some point [2]. If one also considers that not all symptomatic patients actually undergo surgery, the number of affected women is much higher. The rate of women with descensus or incontinence is estimated to be about one-third of all women [3], and it will continue to increase due to demographic change.
Prevalence
Urinary incontinence in pregnancy is common, with a prevalence of 7-60%, although the good news is that it resolves completely in 70-86% of patients [4,5].
Fecal incontinence occurs in 2-13.6% of cases during pregnancy [6], and anal incontinence (additional involuntary discharge of flatus) in up to 65% [7], with rates still 1-6% (fecal) and 13-25% (anal incontinence) after one year [8].
Risk factors
It is estimated that 50% of urinary incontinence and 75% of genital descent are due to pregnancy and childbirth [9]. In recent years, the question of risk factors for pelvic floor dysfunction has become increasingly important in clinical research, with a particular focus on the influence of pregnancy and childbirth. With the identification of risk factors, it is hoped to be able to develop preventive strategies for obstetrics [10], which has already been partially successful.
Studies show that stress incontinence and descensus genitalis are closely associated with pregnancy and vaginal birth [11], but different risk factors are often present simultaneously and therefore isolated effects are difficult to study [12]. Evidence also shows that age, parity, and obesity are among the risk factors for pelvic floor disorders [13].
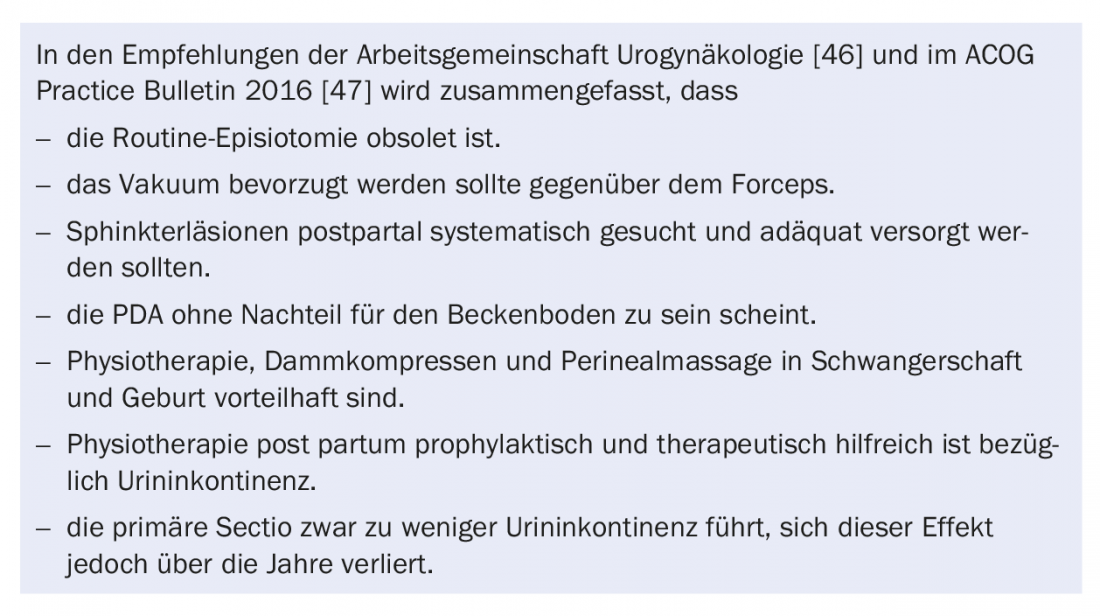
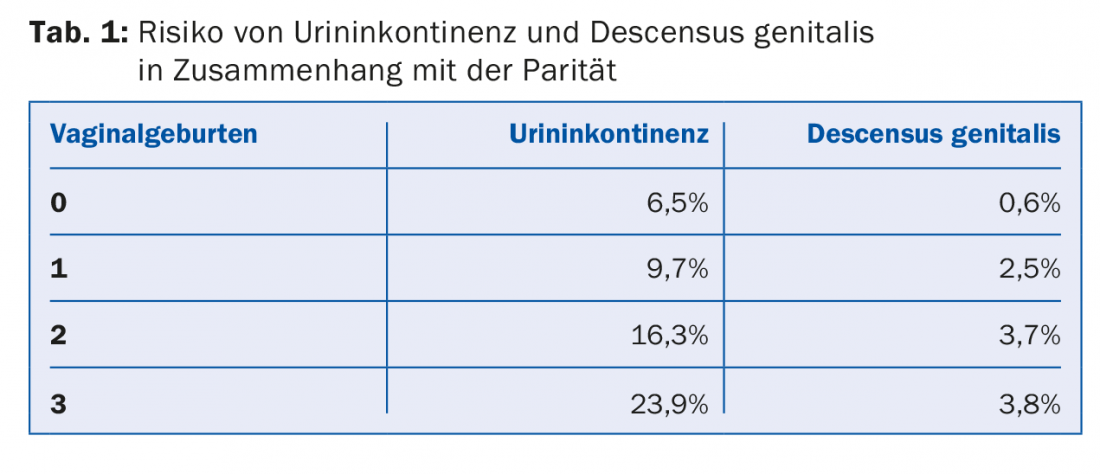
Parity: The risk of urinary incontinence and descensus genitalis increases almost linearly with parity (Table 1) [14,15], with the first birth appearing to have the greatest influence [16]. After menopause, the effect of parity is relativized and age becomes the most important risk factor [15].
Pregnancy: The prevalence and severity of urinary incontinence increase with the course of pregnancy [4].
Vaginal delivery: at birth, the baby’s head circumference is an independent risk factor for pelvic floor dysfunction as is prolonged expulsion [10]. A birth weight >4000 g increases the risk of urinary incontinence later in life by 50% [17]. Compared with cesarean delivery, vaginal delivery has a nearly threefold higher risk of urinary incontinence [18].
Instrumental birth (vacuum bell, forceps): Whereas in the 1920s it was thought that forceps would enable the head to be evacuated in a more controlled manner and thus protect the pelvic floor, it is now known that damage to the levator muscle and the pudendal nerve occurs more frequently after forceps [19]. By using forceps, one additional relevant descensus genitalis occurs for every eight forceps births [20]. Even after up to 23 years, vaginal surgical birth and lower cesarean section increases the risk of pelvic floor disorders [21].
Episiotomy: More than 100 years ago, routine episiotomy was promoted to protect the pelvic floor. The opposite is true: birth injuries are not reduced and descensus and incontinence are not reduced, but even the risk of infections and dyspareunia increases [22], so that episiotomy should be performed routinely only on indication and by no means at every birth.
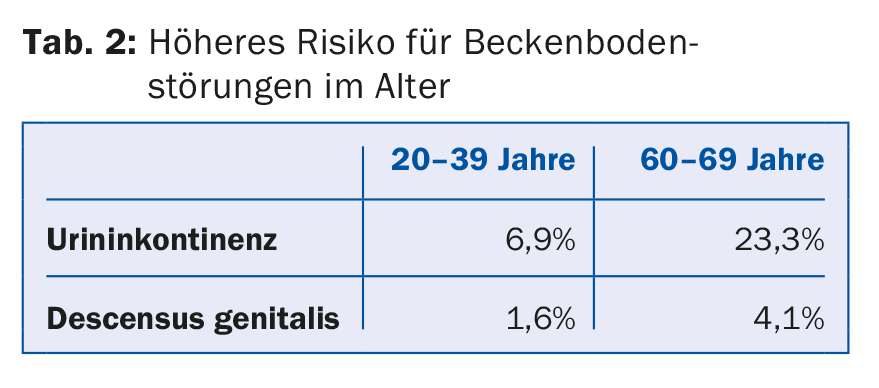
Age: With age, a woman loses about 1% of her pelvic floor muscles per year [23]. This explains a higher risk of pelvic floor disorders at age [15], and maternal age at birth also increases the risk of urinary incontinence by 3% per year of life (Table 2) [24]. In addition, birth trauma at a younger age is compensated by the strength of the pelvic floor and becomes apparent later due to age-related degeneration.
Body weight: a BMI >25 kg/m2 doubles the risk of descensus genitalis [25] and per BMI point increases the risk of urinary incontinence by 8% [24].
Further: chronic constipation also appears to increase the risk [26]. With regard to a genetic component as a risk factor, few data exist [27].
One of the most important risk factors for fecal incontinence is higher grade perineal tears with involvement of the sphincter ani internus/externus muscle at birth [6,8]. Risk factors for higher grade perineal tears include vaginal operative delivery, birth weight, fetal head attitude abnormalities, rapid expulsion, Asian origin, age, primiparity, whereas PDA does not seem to have an influence [28,29]. Detection and adequate primary care of higher grade perineal tears are eminent in preventing fecal incontinence [30,31].
View
Algorithms such as UR-CHOICE are designed to help assess risk for subsequent pelvic floor disorders with known risk factors in order to find “informed consent” for the mode of delivery. This algorithm incorporates data on pre-pregnancy continence status, ethnicity, age at first pregnancy, height, obesity, family history, parity, and infant estimated weight, and it is currently the subject of clinical research [32].
Pathomechanism
Various theories attempt to explain the relationship between pregnancy and childbirth and pelvic floor disorders. Stress incontinence during pregnancy is favored by increasing pressure on the bladder from the growing uterus, the relaxing effect of progesterone in the tissues, and decreased relaxin and collagen and overstretching of the paravaginal tissues, leading to an overmobile urethra and resulting incontinence [33].
During birth, damage to the continence mechanism is discussed, i.e. direct damage to the pelvic floor muscles [34] and/or damage to the motor innervation due to pressure and (over)stretching with consecutive demyelination. Biomechanical computer simulations have shown that some women overstretch their pelvic floor muscles by up to 245% during childbirth [35]. If degenerative manifestations of old age are also present, the damage manifests itself years after the initial trauma [36]. The neuromuscular damage appears to partially regenerate within one year post partum, which could explain the frequent spontaneous remission of stress incontinence in the first year [37].
Prevention
Preventive physical therapy helps reduce the risk of urinary incontinence up to six months post partum, and symptomatic patients with postpartum urinary incontinence experience significant improvement twelve months after delivery [38].
Thus, the focus in the prevention of postpartum incontinence is on physical therapy, but there are other modifiable factors [39]. Grade B recommendations exist for achieving normal weight preconceptually, achieving baseline weight postpartum, exercise, avoiding constipation, and smoking cessation.
Perineal massage may not prevent incontinence or higher grade perineal tears, but it does reduce perineal trauma and persistent pain postpartum [40].
Warm compresses perineally during childbirth, on the other hand, have been shown to result in less urinary incontinence and fewer higher-grade perineal tears [41].
The most important modifiable risk factor is body weight, as a 10% weight reduction decreases urinary incontinence symptoms by 50% [24].
Elective Sectio – “Protect your love channel”?
Especially at the end of the last millennium, cesarean section was provocatively promoted to avoid pelvic floor disorders and sexual insensitivity. This has not prevailed in any of the current guidelines [42–44]because even though the sectio has a lower risk for descensus and incontinence [45]First, eight to nine sectiones would be necessary to prevent one case of urinary incontinence, and secondly, the sectio offers only incomplete protection: even after sectio, the rate of urinary incontinence is 25%, because the pregnancy itself already stresses the pelvic floor. [24]. In addition, the sectio itself is not risk-free (surgical risks, wound pain, fetal respiratory distress syndrome, and adaptation disorders) for either the mother or the child. Many women also underestimate the pain in the days following childbirth that is caused by the sectio.
Therapy
If descensus or incontinence symptoms occur during pregnancy, surgical therapy should only be considered after weaning and the accompanying hormonal changes and regeneration of the pelvic floor. Accordingly, for the treatment of symptoms in pregnancy, the main focus is on physiotherapy and pessaries. Subsequently, surgical measures should also be performed only after family planning has been completed, if possible, because there are few data on pregnancy and birth after incontinence/descensus surgery.
If the decision is made to treat stress incontinence surgically, tension-free vaginal tape (TVT) is currently the gold standard. For the treatment of urge incontinence in pregnancy, oxybutinin preparations are the most suitable (category B).
After a higher-grade perineal tear, history and endoanal ultrasound should help in assessing whether another spontaneous delivery is justifiable or whether a primary incisional delivery should be recommended. Such an assessment can be done in the urogynecology center, so every patient should be offered such a consultation after higher grade perineal tear.
Take-Home Messages
- 11-19% is the lifetime risk for incontinence or descensus surgery.
- Pregnancy and childbirth are causative factors in 50% of urinary incontinence and 75% of genital descent.
- Fecal incontinence is closely associated with higher grade perineal tears.
- Pathomechanisms are likely pudendal and levator lesions.
- Physical therapy, lifestyle modifications (drinking patterns, weight, alcohol/nicotine cessation), perineal massage, and warm compresses during labor are preventively useful.
Literature:
- Sung VW, Washington B, Raker CA: Costs of ambulatory care related to female pelvic floor disorders in the United States. Am J Obstet Gynecol 2010; 202: 483-484.
- Smith FJ, et al: Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 2010; 116: 1096-1100.
- Boreham MK, et al: Anal incontinence in women presenting for gynecologic care: prevalence, risk factors, and impact upon quality of life. Am J Obstet Gynecol 2005; 192: 1637-1642.
- Solans-Domenech M, Sanchez E, Espuna-Pons M: Urinary and anal incontinence during pregnancy and postpartum: incidence, severity, and risk factors. Obstet Gynecol 2010; 115: 618-628.
- Cerruto MA, et al: Prevalence, incidence and obstetric factors’ impact on female urinary incontinence in Europe: a systematic review. Urol Int 2013; 90: 1-9.
- Gyhagen M, et al: Faecal incontinence 20 years after one birth: a comparison between vaginal delivery and caesarean section. Int Urogynecol J 2014; 25: 1411-1418.
- King VG, et al: Using the Brink score to predict postpartum anal incontinence. Am J Obstet Gynecol 2010; 203: 486-485.
- Guise JM, et al: Incidence of fecal incontinence after childbirth. Obstet Gynecol 2007; 109: 281-288.
- Patel DA, et al: Childbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol 2006; 195: 23-28.
- Lavy Y, et al: Can pelvic floor injury secondary to delivery be prevented? Int Urogynecol J 2012; 23: 165-173.
- Leijonhufvud A, et al: Risk of surgically managed pelvic floor dysfunction in relation to age at first delivery. Am J Obstet Gynecol 2012; 207: 303-307.
- Memon HU, Handa VL: Vaginal childbirth and pelvic floor disorders. Womens Health (Lond) 2013; 9: 265-277.
- Jelovsek JE, Maher C, Barber MD: Pelvic organ prolapse. Lancet 2007; 369: 1027-1038.
- DeLancey JO: The hidden epidemic of pelvic floor dysfunction: achievable goals for improved prevention and treatment. Am J Obstet Gynecol 2005; 192: 1488-1495.
- Nygaard I, et al: Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008; 300: 1311-1316.
- Rortveit G, et al: Age- and type-dependent effects of parity on urinary incontinence: the Norwegian EPINCONT study. Obstet Gynecol 2001; 98: 1004-1010.
- Thom DH, et al: Parturition events and risk of urinary incontinence in later life. Neurourol Urodyn 2011; 30: 1456-1461.
- Casey BM, et al: Obstetric antecedents for postpartum pelvic floor dysfunction. Am J Obstet Gynecol 2005; 192: 1655-1662.
- Krofta L, et al: Pubococcygeus-puborectalis trauma after forceps delivery: evaluation of the levator ani muscle with 3D/4D ultrasound. Int Urogynecol J Pelvic Floor Dysfunct 2009; 20: 1175-1181.
- Handa VL, et al: Pelvic floor disorders after vaginal birth: effect of episiotomy, perineal laceration, and operative birth. Obstet Gynecol 2012; 119: 233-239.
- Volloyhaug I, et al: Pelvic organ prolapse and incontinence 15-23 years after first delivery: a cross-sectional study. BJOG 2015; 122: 964-971.
- Hartmann K, et al: Outcomes of routine episiotomy: a systematic review. JAMA 2005; 293: 2141-2148.
- Perucchini D, et al: Age effects on urethral striated muscle. I. Changes in number and diameter of striated muscle fibers in the ventral urethra. Am J Obstet Gynecol 2002; 186: 351-355.
- Gyhagen M, et al: The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 2013; 120: 144-151.
- Swift S, et al: Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 2005; 192: 795-806.
- Weber AM, et al: Posterior vaginal prolapse and bowel function. Am J Obstet Gynecol 1998; 179: 1446-1449.
- Ward RM, et al: Genetic epidemiology of pelvic organ prolapse: a systematic review. Am J Obstet Gynecol 2014; 211: 326-335.
- Wang A, et al: Fecal incontinence: a review of prevalence and obstetric risk factors. Int Urogynecol J Pelvic Floor Dysfunct 2006; 17: 253-260.
- Burrell M, et al: Risk factors for obstetric anal sphincter injuries and postpartum anal and urinary incontinence: a case-control trial. Int Urogynecol J 2015; 26: 383-389.
- Bradley CS, et al: Risk factors for sonographic internal anal sphincter gaps 6-12 months after delivery complicated by anal sphincter tear. Am J Obstet Gynecol 2007; 197: 310-315.
- Sultan AH, et al: Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ 1994; 308: 887-891.
- Wilson D, et al: UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J 2014; 25: 1449-1452.
- Sangsawang B, Sangsawang N: Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment. Int Urogynecol J 2013; 24: 901-912.
- Guzman RR, et al: Impact of levator trauma on pelvic floor muscle function. Int Urogynecol J 2014; 25: 375-380.
- Svabik K, Shek KL, Dietz HP: How much does the levator hiatus have to stretch during childbirth? BJOG 2009; 116: 1657-1662.
- Toglia MR, DeLancey JO: Anal incontinence and the obstetrician-gynecologist. Obstet Gynecol 1994; 84: 731-740.
- Allen RE, et al: Pelvic floor damage and childbirth: a neurophysiological study. Br J Obstet Gynaecol 1990; 97: 770-779.
- Boyle R, et al: Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 2012; 10: CD007471.
- Wesnes SL, Lose G: Preventing urinary incontinence during pregnancy and postpartum: a review. Int Urogynecol J 2013; 24: 889-899.
- Beckmann MM, Garrett AJ: Antenatal perineal massage for reducing perineal trauma. Cochrane Database Syst Rev 2006; CD005123.
- Aasheim V, et al: Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 2017; 6: CD006672.
- Koc O, Duran B: Role of elective cesarean section in prevention of pelvic floor disorders. Curr Opin Obstet Gynecol 2012; 24: 318-323.
- Nelson RL, et al: Cesarean delivery for the prevention of anal incontinence. Cochrane Database Syst Rev 2010; CD006756.
- Lavender T, et al: Caesarean section for non-medical reasons at term. Cochrane Database Syst Rev 2012; CD004660.
- Koc O, et al: Is cesarean section a real panacea to prevent pelvic organ disorders? Int Urogynecol J 2011; 22: 1135-1141.
- Meyer S, et al: The pelvic floor during pregnancy and postpartum: recommendations of the AUG Board. Expert letter SGGG 2012; No. 29.
- Practice Bulletin No. 165: Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstet Gynecol 2016; 128: e1-e15.
HAUSARZT PRAXIS 2018; 13(5): 23-26