Many people with psoriasis suffer from comorbidities. Among mental impairments, the prevalence of depressive disorders is significantly increased compared with the general population. It is assumed that there is a bidirectional interaction structure that negatively influences the course of the disease. A reduction in skin symptoms also helps to alleviate the accompanying psychological symptoms. Nevertheless, depression screening may be useful for patients at risk.
According to the Global Report of the World Health Organization (WHO), psoriasis affects 100 million people worldwide [1]. In addition to arthritis, gastroenterological, cardiovascular and metabolic diseases, depressive disorders are among the frequently occurring comorbidities. During this year’s virtual EADV annual congress, Prof. Dimitrios Ioannides, MD, from the Aristotle University of Thessaloniki (Greece), spoke about the psychological impact of psoriasis [2]. A survey study of more than 5,000 psoriatic patients found that disease-typical skin symptoms such as itching, pain, burning, and hypersensitivity had a significant negative impact on emotional well-being in a majority of sufferers [3]. 82% of respondents reported feeling impaired in their enjoyment of life, 87% felt helplessness, and 89% reported anger and frustration related to psoriasis.
Often psoriasis strikes the psyche
Stigmatization contributes to the psychological burden to a not inconsiderable extent, and a large proportion of those affected suffer from social discrimination. “This points to the importance of effective symptom control,” Prof. Ioannides said. The frequency of depressive symptoms is massively increased in psoriasis sufferers compared to the general population. Secondary analyses showed that 28% of patients with psoriasis or psoriatic arthritis are affected by depressive symptoms. Criteria for clinical depression were met by 12% and 9% of patients required antidepressant medication [4,5]. There appear to be bidirectional relationships, with recent data showing that depressed individuals have a higher risk of psoriasis [6]. The negative psychological impact of psoriatic disease is compounded by other comorbidities such as morbid obesity, diabetes, cardiovascular disease, or gastrointestinal disorders, the speaker explained, explaining that this can lead to a vicious cycle, with psychosocial dimensions and the psoriatic disease condition compounding each other [7]. According to Patel et al. there is a pathophysiological link between psoriasis and depression, which is coupled to the serotonergic system. Thus, indoleamine 2,3-dioxygenase, which is upregulated by several cytokines involved in psoriasis, leads to a decrease in serotonin precursor tryptophan, contributing to lower serotonin levels, which is a known neurophysiological correlate of depressive disorders [8]. In summary, psoriasis is associated with the development of depressive disorders and there are underlying etiopathogenetic commonalities. That psoriatic patients not only have an increased vulnerability to depression, but also to anxiety disorders, sleep disorders, and sexual dysfunction is also considered empirically proven [9].
Screen at-risk patients
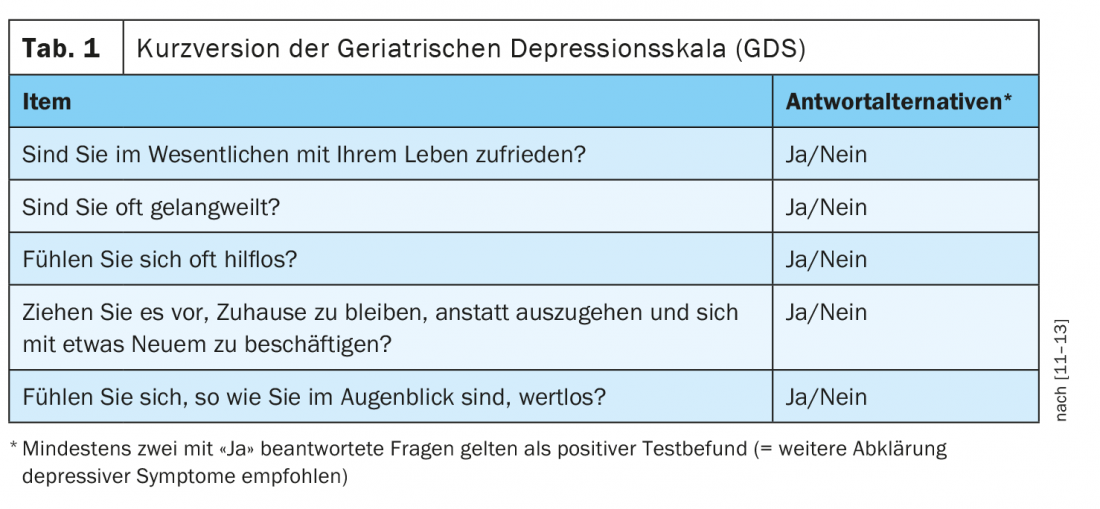
In addition to the Hospital Anxiety and Depression Scale (HADS-D) questionnaire, the GHQ-12 can also be used to screen for psychological distress. Both test procedures are available in a validated German-language version [14–16]. The GHQ-12 is an abbreviated form of the General Health Questionnaire, which is used to survey general health conditions and complaints. It is a self-report questionnaire, and responses to the twelve items are made on a four-point scale. The GHQ-12 is considered a reliable screening tool to detect psychological abnormalities and is commonly used in somatic patients. According to Prof. Ioannides, the “Five-Item Geriatric Depression Scale” has also proven to be a practical depression screening tool (tab. 1) . A score is determined by answering five questions; depending on the result, further clarifications should be made regarding the presence of a depressive disorder. In this context, the speaker emphasized the relevance of interdisciplinary cooperation, especially between dermatological, rheumatological and psychotherapeutic specialists, in order to be able to guarantee an integrative treatment of the systemic disease psoriasis.
Source: EADV 2020
Literature:
- WHO: WHO Global report on Psoriasis 2016, https://apps.who.int/iris/handle/10665/204417
- Ioannides D: The psychological burden of psoriasis. Prof. Dr.med. Dimitros Ioannides, Inflammatory diseases : Psoriasis, EADV Vienna (Virtual), 29.10.2020.
- Armstrong W, et al. : Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003-2011. PLoS One 2012; 7(12): e52935. doi: 10.1371/journal.pone.0052935. Epub 2012 Dec 28.
- Ferreira BR, et al: Analysis of the Prevalence of Mental Disorders in Psoriasis: The Relevance of Psychiatric Assessment in Dermatology. Psychiatr Danub 2017; 29(4): 401-406.
- Dowtlatshahi EA, et al: The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol 2014; 134(6): 1542-1551.
- Min C, et al: Bidirectional association between psoriasis and depression : Two longitudinal follow-up studies using a national sample cohort. J Affective Disord 2020; 262: 126-132.
- Stebut E, et al: Impact of Secukinumab on Endothelial Dysfunction and Other Cardiovascular Disease Parameters in Psoriasis Patients over 52 Weeks. J Invest Dermatol 2018; 139(5): 1054-1062.
- Patel N, et al: Psoriasis, Depression and Inflammatory Overlap: A Review. Am J Clin Dermatol 2017; 18(5): 613-620.
- Ferreira BIRC, et al: Psoriasis and Associated Psychiatric Disorders : A Systematic Review on Etiopathogenesis and Clinical Correaltion. J Clin Aesthet Dermatol 2016; 9(6): 36-43.
- Oji V, Luger TA: The skin in psoriasis: assessment and challenges. Clin Exp Rheumatol 2015; 33 (Suppl 93): S14-S19.
- Hoyl MT, et al: Development and testing of five-item version of the Geriatric Depression Scale. J Am Geriatr Soc 1999; 7: 873-878.
- Maurer DM: Screening for depression. Am Fam Physician 2012; 85(2): 139-144.
- Geriatric Depression Scale (GDS), German translation, www.aio-portal.de/html/studie/pdf/gds.pdf, last accessed 09.11.2020.
- Schmitz N, et al: Psychometric properties of the General Health Questionnaire (GHQ-12) in a German primary care sample. Acta Psychiatrica Scandinavia 1999; 100: 462-468.
- Herrmann-Lingen C, et al: Hospital Anxiety and Depression Scale – German version, 2011, 3rd updated and re-normalized edition.
- Psyndex: https://psyndex.de/tests/info, last accessed 09.11.2020
DERMATOLOGIE PRAXIS 2020; 30(6): 29 (published 12/3/20, ahead of print).











