Fortunately, osteoporosis and its consequences no longer have to be accepted as an untreatable fate. Thanks to intensive research in this field, many options are now available for prevention, early detection and therapy. Several studies published in the second half of 2012 have addressed specific aspects of osteoporosis treatment.
The lifetime risk of suffering an osteoporotic fracture is 51.3% for Swiss women aged 50 years and 20.2% for men [1, 2]. Osteoporotic fractures bring with them increased mortality in addition to limitations in quality of life and functional ability in everyday life. Furthermore, each fracture increases the risk of further fractures.
Bisphosphonates always together with vitamin D?
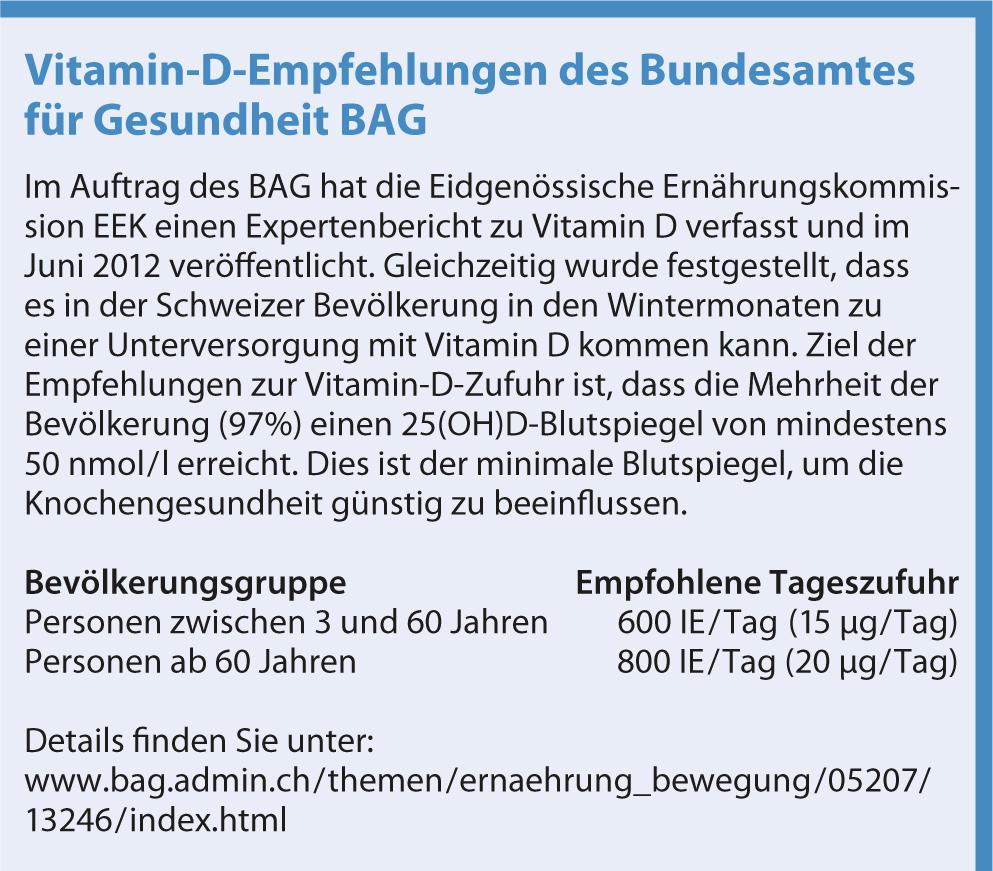
Virtually all guidelines recommend concomitant calcium and vitamin D supplementation during bisphosphonate therapy. In addition, vitamin D was also administered in most bisphosphonate studies. This is despite the fact that little is known about the role of vitamin D in the bisphosphonate treatment of osteoporosis. Is the effect of these drugs supported by vitamin D, or does it even need vitamin D for them to exert their effect?
To address these questions, a Spanish group investigated the extent to which the decrease in bone resorption markers under bisphosphonates depends on Vi-tamine D blood levels in 140 consecutive postmenopausal patients in their osteoporosis consultation [3]. Over three months, women received either aldendronate plus 25OHD3 (ALN+VitD) or alendronate (ALN) alone. As expected, vitamin D3 levels increased significantly in the ALN+VitD group and remained unchanged in the ALN group, whereas the levels of bone resorption markers decreased significantly more in the ALN+VitD group than in the ALN group. However, when the women with baseline vitamin D levels >20 ng/ml and those with levels <20 ng/ml were considered separately, it was apparent that in the latter, bone resorption markers decreased significantly more in the ALN+VitD group than in the ALN group, whereas no differences were found between ALN+VitD and ALN in the women with normal vitamin D levels. The authors conclude that vitamin D supplementation is not mandatory during treatment with bisphosphonates because women with normal vitamin D levels do not benefit from supplementation. In contrast, in women with vitamin D deficiency, the decrease in bone loss markers is about 25% greater when vitamin D is given in addition to bi-sphosphonates.
Does osteoporosis therapy affect fracture healing?
Since bisphosphonates and the monoclonal antibody inhibit osteoclastic bone resorption, early initiation of osteoporosis treatment after a fracture could – on theoretical grounds – have an unfavorable effect on fracture healing. Two studies published at the end of 2012 show that this is not the case.
Gong et al. studied 50 women with distal radius fracture who required osteosynthetic treatment and were diagnosed with osteoporosis [4]. In group 1, bisphosphonate treatment was started two weeks postoperatively, in group 2 only three months postoperatively. The clinical and radiological controls at two, six, ten, 16, and 24 weeks postoperatively showed no differences between the two groups with regard to fracture healing. For this reason, the authors strongly recommend early initiation of bisphosphonate therapy after osteoporotic fracture. The planned subgroup analysis of the placebo-controlled 3-year FREEDOM trial, which evaluated denosumab in postmenopausal women with osteoporosis, found 667 patients with nonvertebral fractures [5]. Again, there were no differences in fracture healing between the verum and placebo groups, leading the authors to conclude that denosumab at a dose of 60 mg every six months neither impairs fracture healing nor leads to increased complications, even when given at the time of fracture or shortly before or after.
Since many women are diagnosed with osteoporosis only at the time of a fracture, it is particularly important that the treating orthopedists do not withhold the proven effective treatment with denosumab or a bisphosphonate from these women for fear of impairing fracture healing, but rather consider osteoporosis drug treatment as an integral part of fracture treatment.
Long-term therapy
Postmenopausal osteoporosis is a chronic condition and requires long-term treatment to keep fracture risk in check. A literature review conducted by the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation (IOF) shows that there are only a few good studies that provide information on long-term therapy for osteoporosis [6]. The authors summarize the following findings:
- Calcium and vitamin D are effective with regard to fracture prevention. However, nothing can be said about benefits and risks after three years based on the current data.
- For the selective estrogen receptor modulators (SERM), nothing can be said about efficacy in terms of fracture prevention after more than five years of treatment, but bone density seems to continue to increase. The long-term safety of SERMs is good, and they also protect against breast cancer.
- Bisphosphonates have been shown to reduce fracture risk for three years, and there are also corresponding 4- and 5-year data for alendronate and risedronate. Bone density appears to continue to increase when therapy is continued for more than five years. The safety of bisphosphonates, with the exception of atypical subtrochanteric femur fracture, appears to be maintained over time.
- For denosumab, there are 5-year data showing that the monoclonal antibody steadily increases bone density over time with good safety.
Treatment of corticosteroid-induced osteoporosis.
Steroid-induced osteoporosis is the most common secondary form and the most common form of osteoporosis of all in young adults. Bone loss begins shortly after steroid administration begins and depends on the dose and duration. Preventive osteoporosis treatment is therefore indicated in all patients receiving a daily equivalent dose of ≥7.5 mg prednisone for at least three months. According to current studies, both bisphosphonates and the anabolic parathyroid hormone teriparatide are suitable for this purpose. Calcium and vitamin D should be supplemented only in cases of deficiency. General osteoporosis preventive measures for patients starting at least three months of steroid therapy are summarized in Table 1.
A Finnish group investigated the efficacy and safety of ibandronate in the prevention of steroid-induced osteoporosis in postmenopausal women with inflammatory rheumatic diseases in a double-blind randomized placebo-controlled trial [8]. In the ibandronate group, bone density in the lumbar vertebral bodies was significantly higher than at baseline six and twelve months after initiation of therapy, and also in the trochanter, femoral neck, and total hip after twelve months. At the same time, bone resorption markers decreased in the verum group compared to the placebo group. Side effects occurred with equal frequency in both groups, although the proportion of severe side effects was slightly greater with ibandronate. Thus, once-monthly administration of oral ibandronate is an effective and safe measure for the prevention of osteoporosis in postmenopausal women on low-dose steroids.

Osteoporosis in men
Osteoporosis is also an important cause of morbidity and mortality in men. Worldwide, 40% of those over 50 years of age who experience an osteoporotic fracture are men. In addition, mortality after osteoporotic fractures is higher in men than in women. These numbers show the importance of studying osteoporosis medications in men as well. To this end, Boonen and coworkers conducted a large, multicenter, double-blind randomized, placebo-controlled trial of zoledronic acid in 1199 men aged 50-58 years, with primary or hypogonadism-associated osteoporosis [9]. The rate of new morphometric vertebral fractures during the 24-month study was 1.6% in the verum group and 4.9% in the placebo group. This corresponds to a 67% risk reduction with zole-dronic acid. Men in the verum group also suffered significantly fewer moderate-to-severe vertebral fractures and significantly fewer height reductions than the placebo group. In addition, fewer clinical vertebral and nonvertebral fractures tended to occur in the zoledronate group, but the difference from the placebo group was not significant because of the small number of cases. Bone density increased significantly more and bone resorption markers decreased significantly more under zoledronic acid than under placebo. No differences were found between the two groups with regard to mortality and serious adverse events. Zoledronic acid is therefore also suitable for reducing the risk of fractures in men with osteoporosis.
CONCLUSION FOR PRACTICE
- Patients with normal vitamin D blood levels do not benefit additionally when bisphosphonates are supplemented with vitamin D supplementation.
- Osteoporosis therapy (bisphosphonates, monoclonal antibodies) do not have a negative effect on fracture healing, so there should be no delay in starting treatment after an osteoporotic fracture.
- Patients receiving low-dose corticosteroids for at least three months require osteoporosis prophylaxis.
- Osteoporosis is not only a problem of menopausal women. Men account for 40% of osteoporotic fractures in those over 50 years of age.
Literature:
- Lippuner K, et al: Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int 2010; 21: 381-3898.
- Rizzoli R, et al: Osteoporosis in Switzerland in 2008: a call to action. Switzerland Med Forum 2008; 8(Suppl.45): 1-11.
- Olmos JM, et al: Effects of 25-hydroxyvitamin D3 therapy on bone turnover markers and PTH levels in postmenopausal osteoporotic women treated with alendronate. J Clin Endocrinol Metab 2012; 97: 4491-4497.
- Gong HS, et al: Early initiation of bisphosphonate does not affect healing and outcomes of volar plate fixation of osteoporotic distal radial fractures. J Bone Joint Surg Am 2012; 94: 1729-1736.
- Adami S, et al: Denosumab treatment in postmenopausal women with osteoporosis does not interfere with fracture-healing: results from the FREEDOM trial. J Bone Joint Surg Am 2012; 94: 2113-2119.
- Cooper C, et al: Long-term treatment of osteoporosis in postmenopausal women: a review from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation (IOF). Curr Med Res Opin 2012; 28: 475-491.
- Briot K, Roux C.: Ostéoporosis cortico-induite. Rev Med Interne 2012. epub ahead of print.
- Hakala M, et al: Once-monthly oral ibandronate provides significant improvement in bone mineral density in postmenopausal women treated with glucocorticoids for inflammatory rheumatic diseases: a 12-month, randomized, double-blind, placebo-controlled trial. Scand J Rheumatol 2012; 41: 260-266.
- Boonen S, et al: Fracture risk and zoledronic acid therapy in men with osteoporosis. N Engl J Med 2012; 367: 1714-1723.