Metabolic surgery is a promising therapeutic option for the treatment of morbid obesity. This is because there is high evidence that it is more effective than conservative therapy in poorly controlled type 2 diabetes mellitus and BMI even below 35 kg/m2.
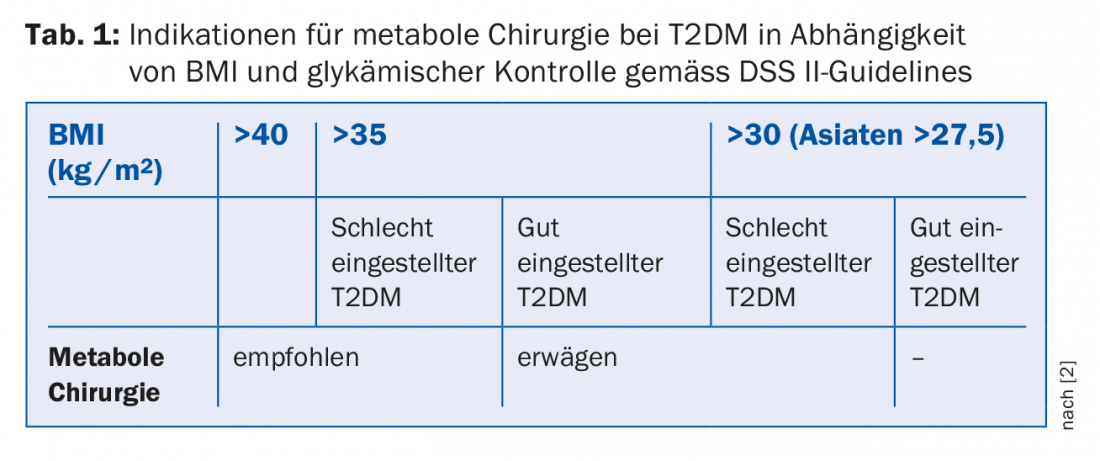
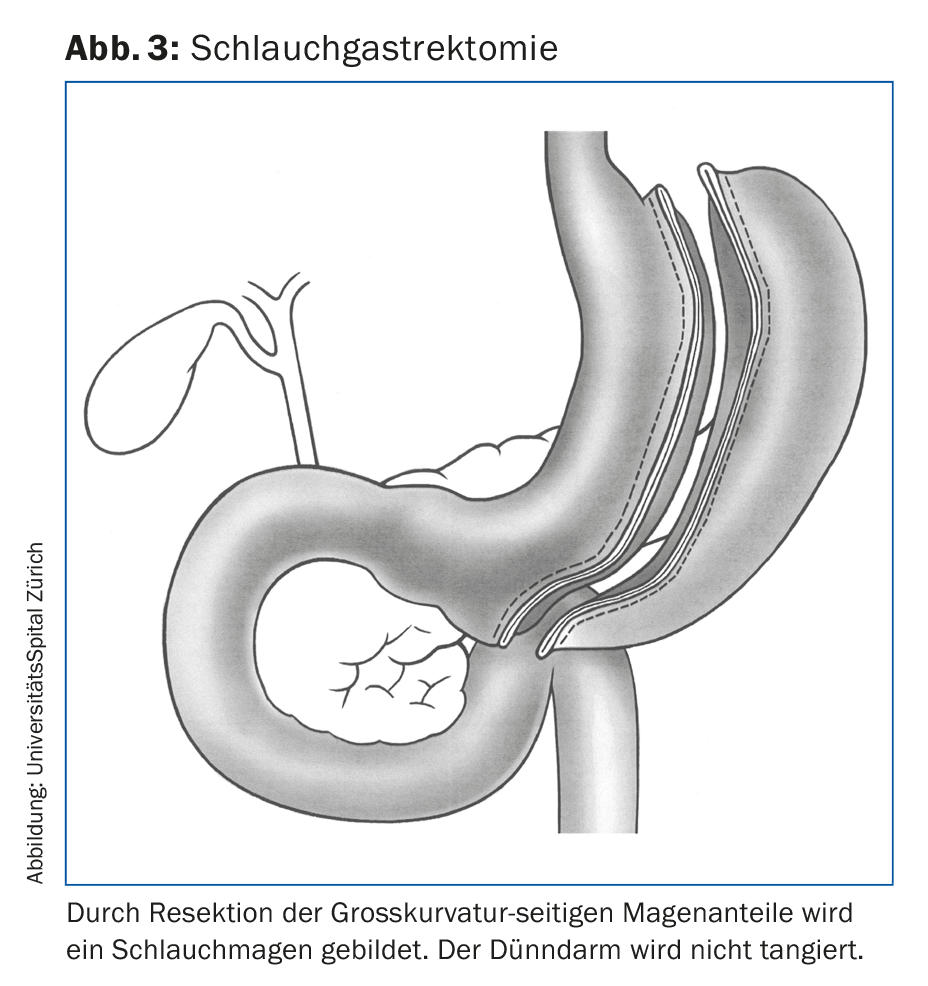
When the first gastrointestinal surgeries were developed over sixty years ago with the goal of treating morbid obesity, the primary goal was to reduce weight. Relatively quickly, however, it became clear that these surgeries also improved the comorbidities associated with obesity, life expectancy, and quality of life, which also had a long-term impact on health care costs. More than twenty years ago, there were already several reports of high rates of remission of type 2 diabetes mellitus (T2DM) after gastric bypass. Animal but also human data on the mechanisms underlying the weight-independent effect of bariatric surgical methods on glycemic control and lipid metabolism followed [1]. This gave rise to the term “metabolic surgery.” In 2015, international experts in endocrinology, surgery, gastroenterology, and members of the research community met in London for the second Diabetes Surgery Summit (DSS II) to evaluate the evidence available to that point on the success of metabolic surgery compared with conventional medical therapy in the treatment of T2DM. On the one hand, they formulated recommendations for the surgical therapy of T2DM in morbid obesity, but on the other hand also provided an assessment of the therapeutic options for diabetic patients with a BMI <35 kg/m2 ( Tab. 1). An entire issue of a hitherto very surgery-critical journal was dedicated to these DSS II guidelines [2]. Since then, the recommendations have been ratified by over fifty-five international professional societies.
Which operation for which patient?
Conservative therapeutic measures for the treatment of morbid obesity are very rarely successful in the long term (<4%) [3]. In contrast, surgery with permanent effect is 90% successful [4,5]. Preoperatively assessing which patient needs which type of surgery is not a simple undertaking. Purely restrictive surgical procedures, such as. gastric banding surgery, lead to sufficient weight loss and reduction of comorbidities in the long term in only about 10%, as they show hardly any metabolic effects independent of weight loss [6]. Proximal Roux-Y gastric bypass remains the gold standard (Fig. 1) . In addition to its restrictive effect, this procedure also has a strong metabolic effect. It has a malabsorptive effect only as an undesirable side effect on micronutrients (vitamins and trace elements), but not on macronutrients, i.e. calories. Because no tissue is removed, the surgery is potentially reversible. Today, it is performed almost exclusively by laparoscopic means. Relevant complications occur in experienced centers in <1% of cases. Temporarily, the laparoscopic technique led to an increase in a classic late complication, internal hernias, a dislocation of small bowel segments between the mesenteric lacunae. Since these gaps are closed during the initial procedure, the rate of internal hernias has decreased significantly. Clinically, they manifest as postprandial abdominal pain, more rarely as acute abdomen with ileus. Other late complications include dumping complaints. Occasionally, therapy-refractory late dumping may occur, which in (rare) extreme cases may lead to the need to reverse the procedure. Even with consistent lifelong vitamin and trace element supplementation, deficiency symptoms can occur with all weight-loss interventions. Therefore, patients are urged to perform regular checks and, if necessary, to take additional supplements. Morbid obesity is a chronic disease that can recur in the form of secondary weight gain and recurrence of comorbidities. In approximately 5% of patients, a follow-up procedure is then performed after renewed interdisciplinary evaluation.
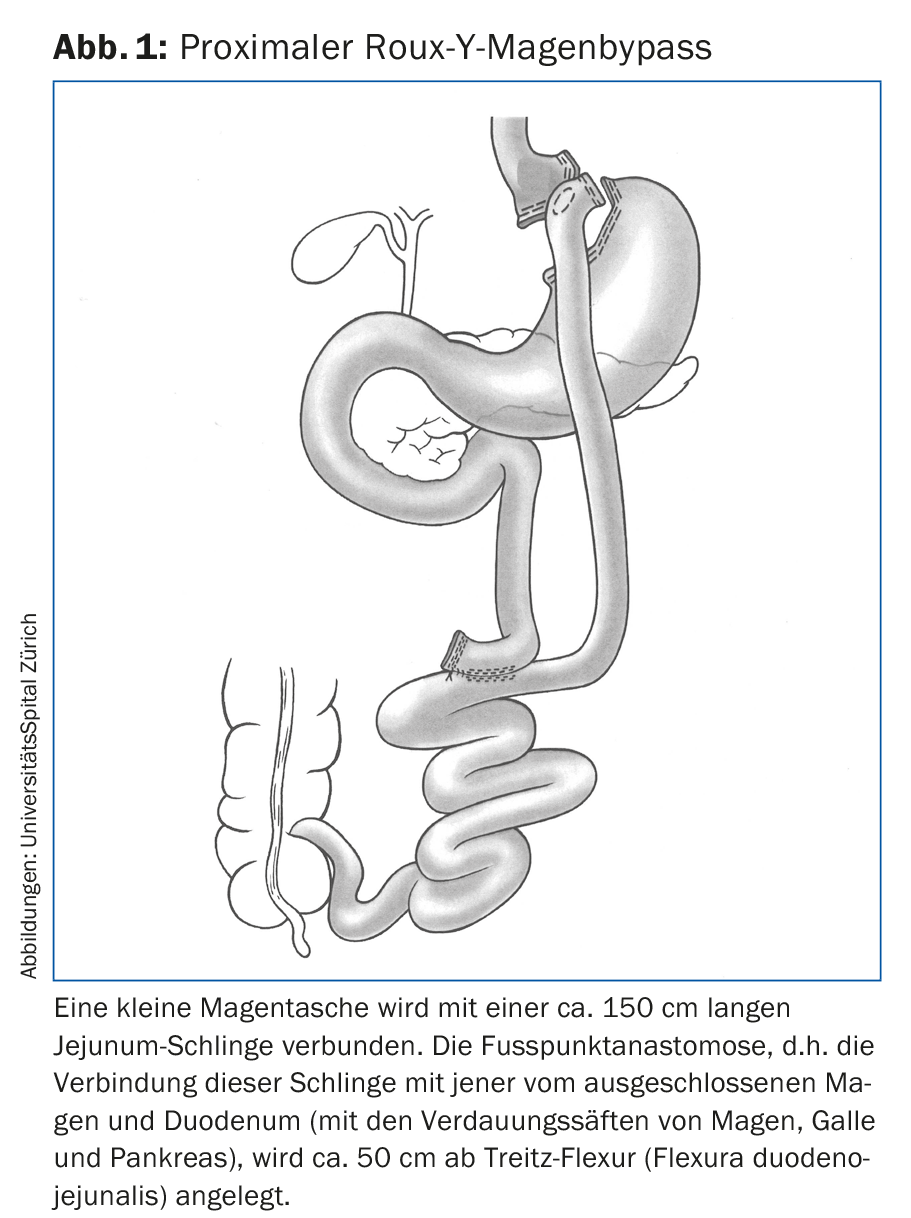
Biliopancreatic diversion surgery (BPD) (Fig. 2) has restrictive, malabsorptive, and metabolic effects and is arguably the most effective treatment modality today in terms of weight loss and T2DM remission rate (approximately 95%). The price, however, is quite high with significantly increased stool frequency, foul-smelling flatulence, and both micro- and macronutrient deficiencies. Therefore, this surgery is only under discussion when very high body weight and/or severe secondary morbidities do not respond to the simpler primary surgeries. In patients with extremely high BMI, this surgery is difficult to perform laparoscopically in one step. For this reason, a two-stage approach was developed consisting of primary tubal gastrectomy (Fig. 3) and gastric bypass or BPD 1-2 years later. However, after patients successfully lost weight with tube gastrectomy alone, in that this method showed similar metabolic effects to gastric bypass [7–9], the procedure has gained popularity as a sole primary intervention. It is already performed more frequently than gastric bypass in France, Germany, the Middle East, and the United States.
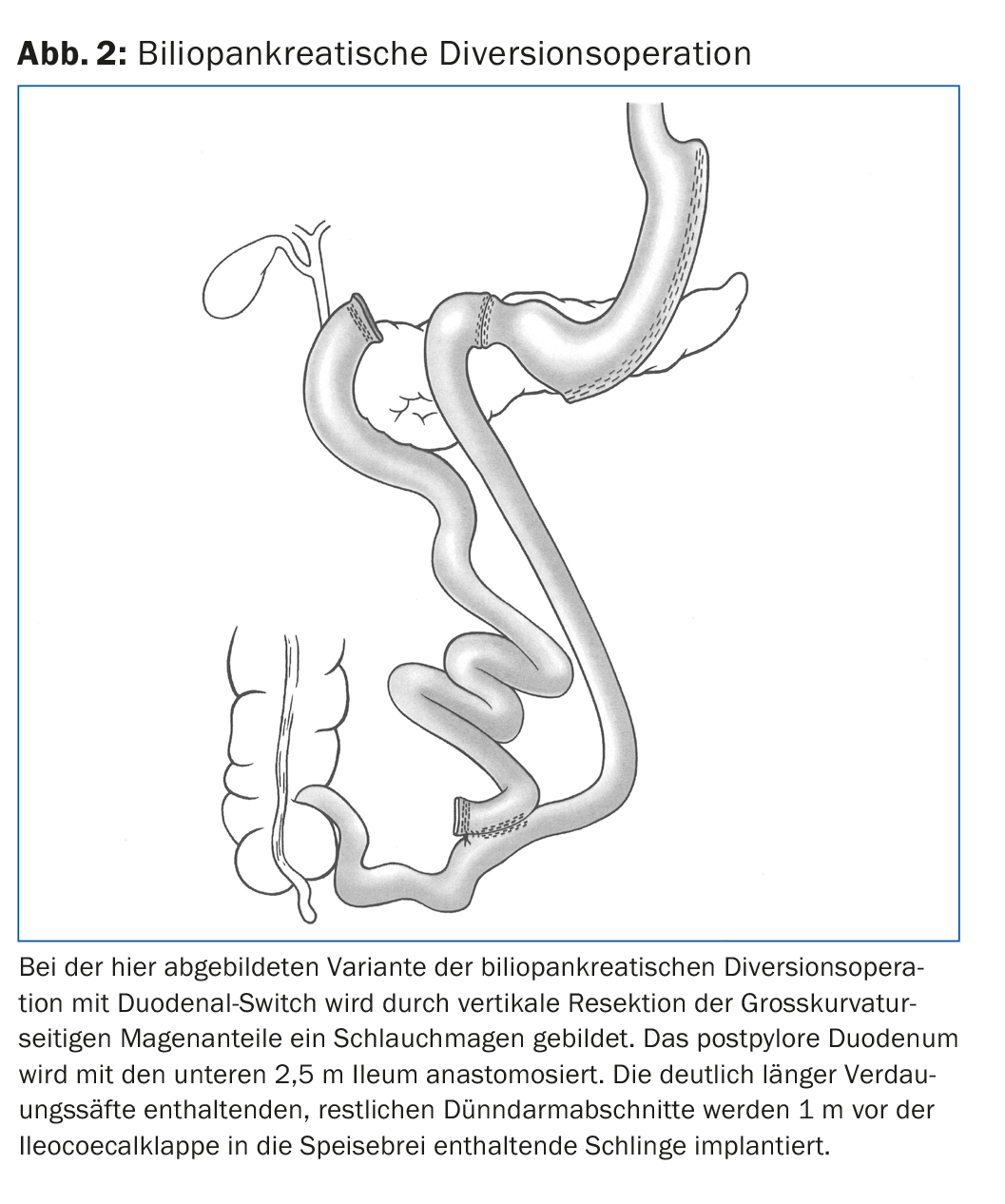
In a randomized Swiss multicenter trial, we were able to compare five-year outcomes of these two surgical methods (tubular gastrectomy and gastric bypass). There was no significant difference in weight loss with 61.5% excess weight loss by tube gastrectomy and 68% by gastric bypass. T2DM remission rates were 60% in both >, but dyslipidemia and gastroesophageal reflux disease were more successfully treated with bypass. Quality of life improved identically with both surgeries, and the rate of reoperation was not significantly different [10].
Other procedures (omega loop gastric bypass, endoscopic transgastric procedures, etc.) have yet to provide scientific proof of their effectiveness and safety, so they should not be used outside of studies in Switzerland at the moment.
Several factors influence the choice of the right procedure for the individual patient. Thus, extent of obesity, fat distribution, age, gender, type and severity of comorbidities, eating patterns, bowel habits, metabolism (basal metabolic rate, carbohydrate and fat burning), possibly genetic factors, understanding of dietary changes and expected reliability in terms of attending follow-up examinations, and patient wishes are important in the selection process. After interdisciplinary evaluation, the optimal intervention for the patient must be selected together with the patient, in the knowledge that an exact prognosis for the individual case is not possible. Gastric bypass is particularly indicated in patients with large hiatal hernia, severe reflux, T2DM, and dyslipidemia. Good candidates for tube gastrectomy are highly motivated patients with extremely high BMI in a two-stage approach, patients with multiple adhesions after previous surgery or large scar hernias, and possibly patients with chronic inflammatory bowel disease.
Developments in Switzerland
Before bariatric surgery became a recognized mandatory service in Switzerland, the Federal Council, via the Federal Office of Public Health, mandated the Swiss Society for the Study of Morbid Obesity and Metabolic Disorders (SMOB), an interdisciplinary professional society, to formulate guidelines for the treatment of morbid obesity. When the guidelines came into effect in February 2011, bariatric surgery was recognized as a mandatory service for patients with BMI >35 kg/m2 after unsuccessful conservative therapy for a total of two years (one year for BMI >50 kg/m2 ). Furthermore, quality criteria regarding selection, preparation, treatment and aftercare were defined and criteria were developed as to who is allowed to perform which operations. Primary centers for the simpler interventions and secondary centers for more complex interventions were defined (www.smob.ch). The guidelines have been revised several times. Earlier this year, treatment of adolescents was also implemented in collaboration with the Society of Pediatrics. This patient group in particular must be selected and cared for with the utmost care.
Following the introduction of bariatric surgery in Switzerland, a “Health Technology Assessment” was conducted by the Swiss Medical Board and published at the end of 2016. The objective of this HTA report was to evaluate the efficacy, safety, cost-effectiveness, and budgetary impact as well as the legal and ethical effects of bariatric surgery compared with conservative treatments. This showed a statistically significant advantage of surgery over conservative treatment in terms of weight loss, body function, reduction in HbA1c and T2DM remission, and improvement in hypertension and dyslipidemia. In addition, surgery was judged to be more cost-effective compared with conventional treatment. It was also noted that the Health Insurance Act has a tendency to favor conservative treatments, which is not justified according to the Swiss Medical Board report [11].
After an initial increase in the number of procedures, these have leveled off at about 5000 operations per year throughout Switzerland (75% gastric bypasses, 20% tubular stomach and a few gastric band and BPD operations). This number represents less than 4% of the 140,000 patients who would qualify for bariatric surgery according to the criteria.
Together with the Swiss Society of Endocrinology and Diabetology, the SMOB is currently in the process of making metabolic surgery accessible to patients with poorly adjustable T2DM and BMI 30-35 kg/m2, as is already possible in England, India, Israel and Spain. This is because BMI is less decisive as a criterion than metabolic state. The Conference of Health Directors is also seeking to regulate complex bariatric surgery as part of highly specialized medicine. Bariatric surgery in Switzerland is characterized by very high quality. Early morbidity is a few percent and mortality is less than 1‰. Fortunately, the follow-up rate in our country is very high in international comparison. This is important not only for the individual patient in terms of successful treatment of the chronic disease obesity, but also for the treating center, which can continuously optimize its treatment strategy by analyzing its own results.
Take-Home Messages
- Bariatric surgery has many weight-independent metabolic effects, which is why it is called “metabolic surgery.”
- The goal of metabolic surgery, in addition to weight loss, is to improve to remission of comorbidities, extend life expectancy, and improve quality of life, which contributes to cost-effectiveness.
- There is high evidence that metabolic surgery is more effective than conservative therapy for poorly controlled type 2 diabetes mellitus and BMI also <35 kg/m2.
- In Switzerland, metabolic surgery is regulated by SMOB guidelines. The treatment of patients should always be interdisciplinary.
- Approximately 5000 operations are performed annually throughout Switzerland – with a low morbidity and very high follow-up rate compared to other countries.
Literature:
- Batterham RL, Cummings DE: Mechanisms of diabetes improvement following bariatric/metabolic surgery. Diabetes Care 2016; 39: 893-901.
- Rubino F, et al: Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care 2016; 39: 861-877.
- Sjöström L, et al: Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004; 351: 2683-2693.
- Adams TD, et al: Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med 2017; 377: 1143-1155.
- Sjöström L, et al: Bariatric surgery and long-term cardiovascular events. JAMA 2012; 307: 56-65.
- Vinzens F, et al: Long-term outcome of laparoscopic adjustable gastric banding (LAGB): results of a Swiss single-center study of 405 patients with up to 18 years’ follow-up. Surg Obes Relat Dis 2017; 13: 1313-1319.
- Peterli R, et al: Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg 2009; 250: 234-241.
- Peterli R, et al: Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, prospective trial. Obes Surg 2012; 22: 740-748.
- Wölnerhanssen B, et al: Effects of postbariatric surgery weight loss on adipokines and metabolic parameters: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. A prospective randomized trial. Surg Obes Relat Dis 2011; 7: 561-568.
- Peterli R, et al: Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA 2018; 319: 255-265.
- Swiss Medical Board: Bariatric surgery vs. conservative treatment for obesity and overweight. Assessment. Final report 16 june 2016.
HAUSARZT PRAXIS 2018; 13(10): 26-29











