In the case of colorectal carcinoma, surgery is still the only way to cure the disease. Primary therapy of colon carcinoma consists of oncologic resection of the tumor-bearing bowel segment. In rectal cancer, neoadjuvant radiochemotherapy is an integral part of the treatment concept for advanced tumors. The prognosis of patients with rectal cancer was revolutionized by the introduction of the surgical technique of total mesorectal excision (TME) by Sir Bill Heald. The same concept must be applied to colon carcinomas.
Preoperatively, every patient with colon carcinoma should undergo adequate staging, which includes determination of CEA levels in addition to clinical examination. To determine the local tumor extent and to exclude a second carcinoma, a complete colonoscopy or, in case of a stenosing tumor, a colon contrast enema or a virtual colonoscopy should always be performed. An ultrasound of the liver should be performed to exclude metastasis, as well as an abdominal CT (and thoracic CT if necessary).
Surgical therapy of colon carcinoma
Primary therapy for colon carcinoma is local R0 resection with a safety margin of at least 5 cm with oncologic lymph node dissection [1]. Because lymphatic drainage follows the course of the arterial vessels, the close interposition of the arterial vessels is an essential component of radical tumor resection with central oncologic lymph node dissection (Fig. 1).
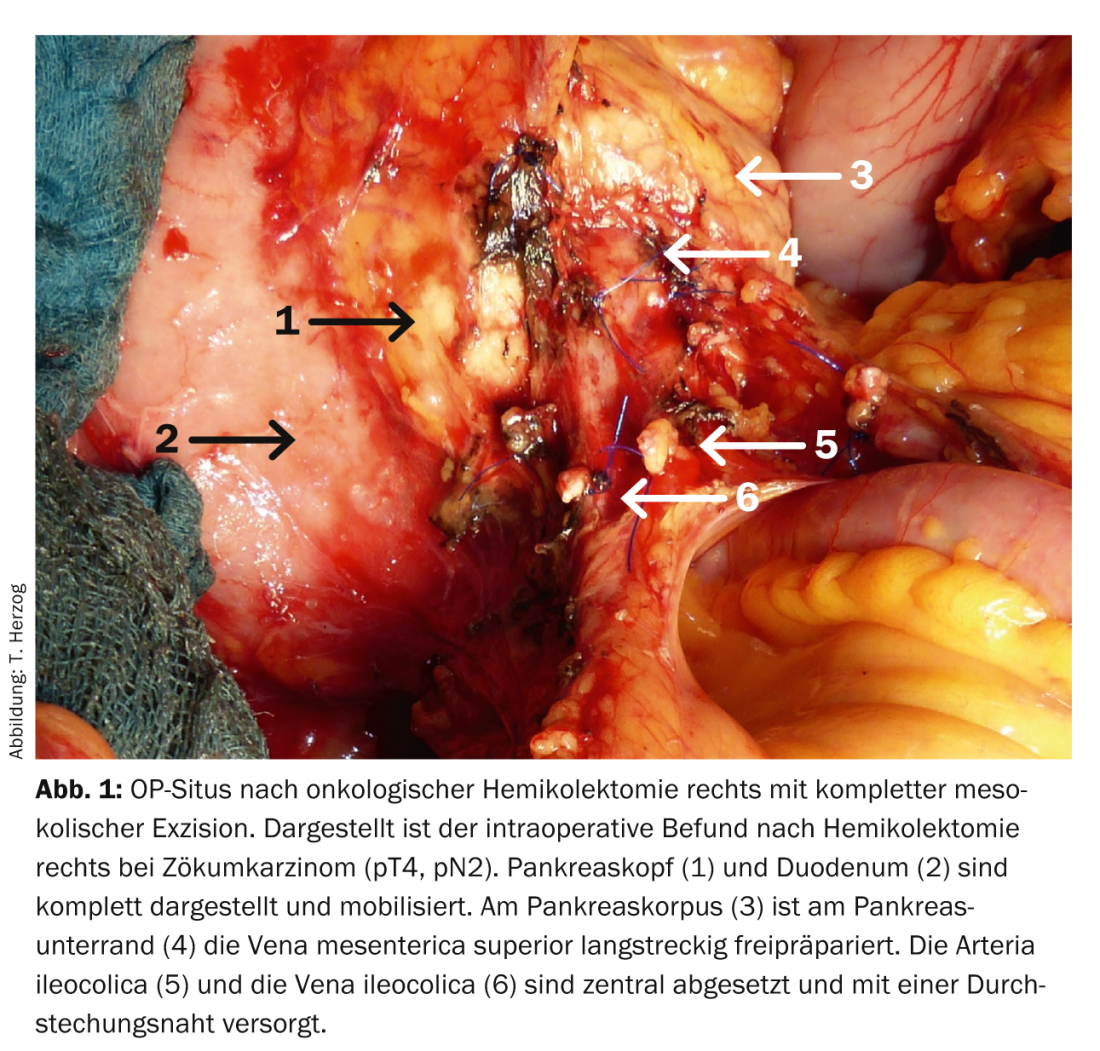
Furthermore, resection should be performed with preservation of the embryonic envelope layers, i.e. with intact integrity of the mesocolon analogous to total mesorectal excision (TME) for rectal cancer as so-called “complete mesocolic excision” (CME) [2]. For adequate staging, at least twelve lymph nodes should be removed and examined histo-pathologically, which is virtually always warranted with central vascular ligation [3].
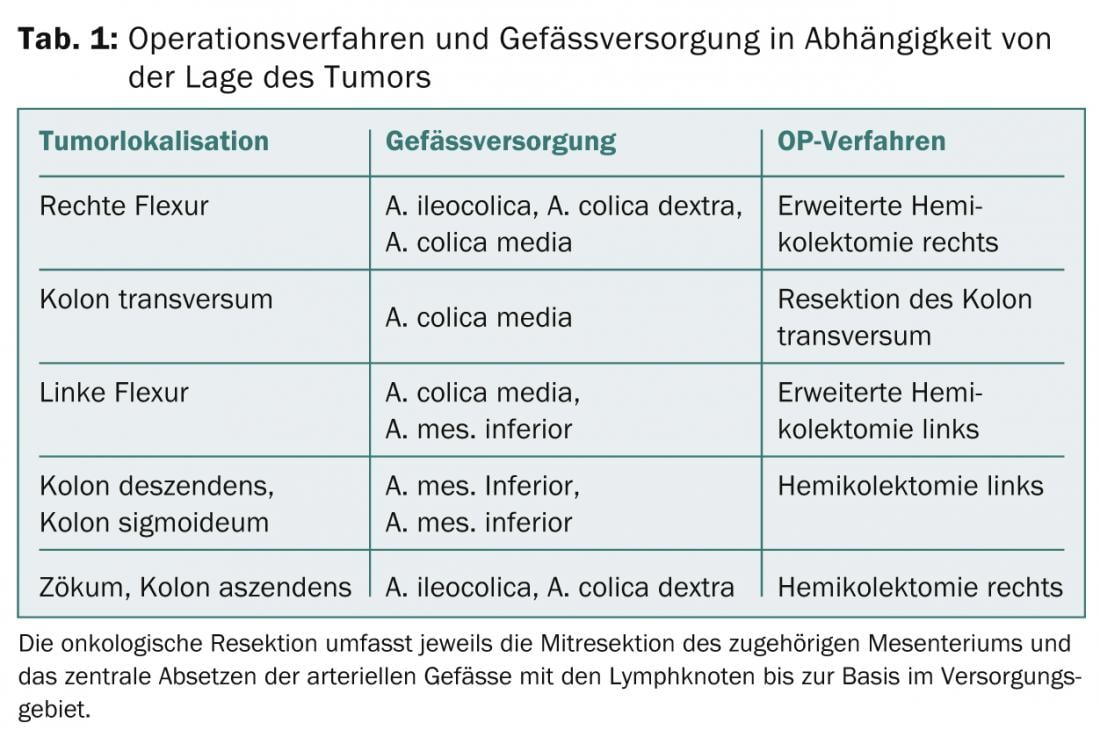
Due to the arterial vascular supply, the tumor location determines the surgical procedure (Tab. 1). In order to achieve a local R0 situation, resection of infiltrated neighboring organs is necessary and oncologically useful for T4 tumors. Patients with isolated hepatic or pulmonary metastases should be presented to a surgeon with appropriate expertise and discussed in interdisciplinary tumor conferences.
In the palliative situation, hepatic metastasis is usually the prognostically decisive factor, so that primary tumor resection is not always necessary in the absence of obstruction. However, it is important to avoid emergency surgery for tumor perforation or obstruction with ileus because emergency surgery is associated with a worse prognosis [4]. In this respect, palliative tumor resection for the prophylaxis of ileus is quite reasonable, provided that the resection is performed with a low morbidity. Alternatively, the minimally invasive creation of a stoma for ileus prophylaxis may be useful. Endoscopic placement of intraluminal bowel stents may be appropriate in exceptional cases of left-sided obstruction, but it also carries numerous risks and therefore cannot be generally recommended [5,6]. After endoscopic ablation of a T1 carcinoma in histologically carcinoma-free (R0) polyp base and low-risk situation (G1, L0), a postresection may be omitted, but in the high-risk situation, radical oncologic surgical treatment should be performed.
Surgical therapy of rectal cancer
The multimodal therapy concept of patients with rectal cancer should be discussed in close cooperation with radiotherapists and oncologists in interdisciplinary tumor conferences. The goal of any surgical treatment of rectal cancer is a local R0 resection. For preoperative diagnosis, endosonography is essential to assess the lymph node status and pelvic MRI is indispensable nowadays to assess the circumferential resection margin. As in colon cancer, evaluation of distant metastases is best accomplished by sonography and contrast-enhanced CT scan. For advanced tumor stages (uT3 and uT4) and regional lymph node metastases (uN+), 5-fluorouracil-based neoadjuvant radiochemotherapy with a radiation dose of 50 Gray should be performed [1,7].
The introduction of total mesorectal excision (TME) has revolutionized the surgical management of patients with rectal cancer.This technique was introduced by Sir Bill Heald and is now established as the gold standard [8]. TME is based on the anatomical-embryonic enveloping fasciae in the lesser pelvis and consists of complete excision of the mesorectal fat body without injury to these enveloping fasciae from the lesser pelvis. This completely removes the tumor-surrounding lymphatic tissue that locally surrounds the rectum, significantly reducing the risk of local recurrence in the long-term to less than 5%.
For rectal carcinomas of the lower to middle rectal third (0-12 cm from anocutaneous line), TME should always be performed; for rectal carcinomas of the upper rectal third (13-16 cm from ano), partial mesorectal excision (PME) is sometimes sufficient. If this preparation layer is respected, the important sacral nerves can always be spared. The quality of the mesorectal excision is important because there is a direct correlation between the surgical quality of the TME preparation and overall survival [9,10]. To perform adequate lymph node dissection, the inferior mesenteric artery should be transected centrally approximately 2 cm downstream from the aorta, sparing the sacral nerve origin.
Continence-preserving surgery is possible for tumors up to 1 cm ab ano. Depending on the height of the tumor, reconstruction is performed as a descendo rectostomy or a coloanal anastomosis. Reconstruction should include the formation of a pouch, and the long-term results after transverse coloplasty (“Bernese pouch”) and J-pouch are equivalent [11].
Installation of an ileostomy reduces mortality
The creation of a temporary, protective double-lumen ileostomy should be performed in all rectal resections of the lower and middle thirds of the rectum, as this can reduce morbidity and lethality [12]. In sphincter infiltrating tumors, surgical radicality takes precedence over sphincter preservation. For patients with sphincter infiltration, abdominoperineal rectal extirpation with terminal colostomy is a reasonable treatment alternative. Functional outcomes after rectal resection depend on the level of anastomosis; patients with preoperative radiation and coloanal anastomosis have the highest risk of incontinence.
In early rectal cancer, the risk for lymphogenic metastasis depends on the depth of infiltration of the tumor into the rectal wall. For early carcinomas with infiltration of the upper or middle third of the submucosa (T1sm1 or T1sm2, respectively), local transanal endoscopic microsurgery (TEM) is an alternative to the open procedure with TME if this excision can be performed with an appropriate safety margin.
Prof. Dr. med. Waldemar Uhl
Literature:
- Pox C, et al: [S3-guideline colorectal cancer version 1.0]. Z Gastroenterol 2013; 51: 753-854.
- Hohenberger W, et al: Standardized surgery for colonic cancer: complete mesocolic excision and central ligation – technical notes and outcome. Colorectal Dis 2009; 11: 354-364; Discussion 364-355.
- Chang GJ, et al: Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 2007; 99: 433-441.
- Bass G, et al: Emergency first presentation of colorectal cancer predicts significantly poorer outcomes: a review of 356 consecutive Irish patients. Dis Colon Rectum 2009; 52: 678-684.
- Cirocchi R, et al: Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol 2013; 22: 14-21.
- Pirlet IA, et al: Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 2011; 25: 1814-1821.
- Sauer R, et al: Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004; 351: 1731-1740.
- Heald RJ, Ryall RD: Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1986; 1: 1479-1482.
- Maslekar S, et al: Mesorectal grades predict recurrences after curative resection for rectal cancer. Dis Colon Rectum 2007; 50: 168-175.
- Herzog T, et al: TME quality in rectal cancer surgery. Eur J Med Res 2010; 15: 292-296.
- Biondo S, et al: Long-term functional results from a randomized clinical study of transverse coloplasty compared with colon J-pouch after low anterior resection for rectal cancer. Surgery 2013; 153: 383-392.
- Ulrich AB, et al: Diverting stoma after low anterior resection: more arguments in favor. Dis Colon Rectum 2009; 52: 412-418.
InFo Oncology & Hematology 2014; (2)7: 7-9.











