Due to the increasingly aging population, the number of those suffering from age-related eye diseases is also rising. The three most common causes of blindness in industrialized nations are age-related macular degeneration, glaucoma, and diabetic retinopathy.
Not all diseases cause classic and clear symptoms in the patient, so regular ophthalmologic check-ups are necessary as a precaution. However, even as a primary care physician, it is helpful to know the symptoms and complaint patterns of the various diseases in order to be able to ensure targeted and timely referral. We present selected clinical pictures.
Wet macular degeneration
Age-related macular degeneration is a disease of the central part of the retina, which is responsible for sharp vision. A distinction is made between a dry and a wet form of macular degeneration. The dry form is unfortunately not treatable, but usually progresses slowly. In wet macular degeneration, there can be a rapid, significant deterioration in visual acuity. Reading ability in particular is impaired in this clinical picture. A sudden onset of wavy vision (metamorphopsia) is the most common symptom here. Since there is the possibility of a treatment in wet macular degeneration by means of medication in the form of injections into the vitreous cavity of the eye to avoid the loss of central visual acuity, a prompt presentation to the ophthalmologist should be made here.
Glaucoma
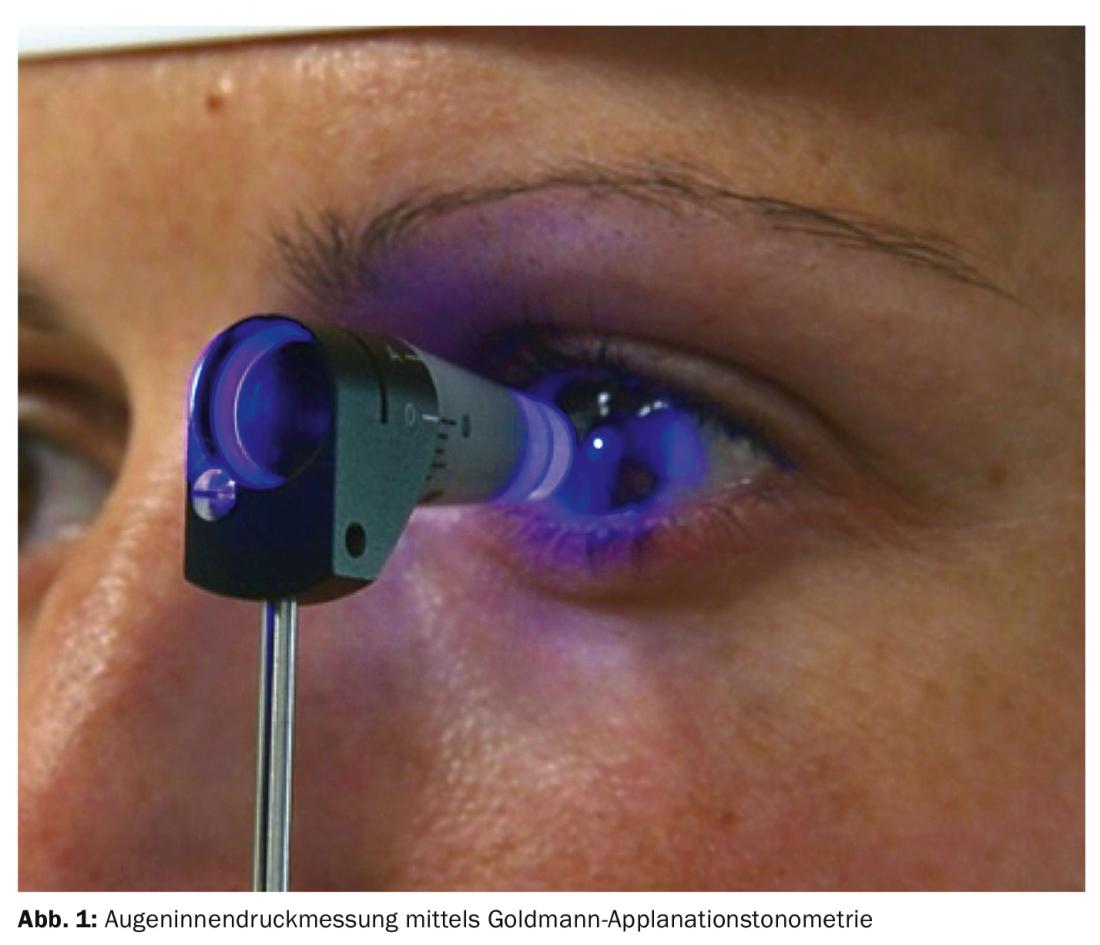
Glaucoma, popularly known as “glaucoma”, is a progressive optic nerve disease. Due to the loss of retinal ganglion cells, visual field defects occur in the course of the disease, which are not noticed by the affected person at first. If left untreated, there is a risk of going blind from glaucoma. In the past, glaucoma was equated with elevated intraocular pressure. However, the amount of intraocular pressure an optic nerve can tolerate varies greatly from individual to individual. Even patients with intraocular pressure within the statistical norm (10-21 mmHg) may have glaucoma. Therefore, a mere intraocular pressure measurement is not sufficient to make a diagnosis (Fig. 1) . An additional optic nerve examination by the ophthalmologist is required. Since the probability of developing glaucoma increases with age, regular check-ups by an ophthalmologist are recommended from the age of forty. If there is a family history or presence of other risk factors such as myopia, earlier examination is advisable.
A special form of glaucoma is narrow-angle glaucoma or glaucoma attack. In this case, anatomical peculiarities lead to a complete obstruction of the aqueous humor outflow, which causes a sudden increase in intraocular pressure. The typical symptoms of this increase are visual disturbances and eye pain. However, general and rather difficult to classify vegetative symptoms such as nausea, vomiting, headache or even chest pain may also occur. These then often first take the patient to a general medical emergency room. To ensure prompt referral to an ophthalmologist, it is important that the treating non-ophthalmologist is aware of this differential diagnosis [1]. Rapid reduction of intraocular pressure is necessary to prevent permanent damage.
Cataract
The very similar sounding disease, “cataract”, on the other hand, is a clouding of the lens in the eye, called a cataract. In the Western world, cataract surgery is one of the most commonly performed procedures [2]. In developing countries, cataract remains the most common cause of blindness due to the lack of adequate surgical options [3]. Classic symptoms are a slow deterioration of vision, perception of a gray haze, and glare sensitivity. The necessity of cataract surgery depends mainly on the subjective feeling of the patient. However, it has also been shown that visual improvement after cataract surgery results in a decrease in the incidence of falls [4].
Diabetic retinopathy
Another common cause of visual deterioration is diabetic retinopathy associated with diabetes mellitus (Fig. 2). Poor glycemic control leads to hypoxia of the retina, which releases angioproliferative factors. These can lead to the formation of new vessels of poor quality, which can result in hemorrhages and, in the case of unfavorable growth, retinal detachments. A barrier disorder of the vessels can lead to fluid accumulation in the retina, which, in addition to the oxygen deficiency, can also result in a deterioration of visual acuity. Eye involvement in diabetes mellitus may go unnoticed for a long time. For this reason, diabetes patients should be examined by an ophthalmologist at least every two years. Depending on whether further risk factors are present or whether changes in the retina have already been detected, the time intervals have to be chosen more closely [5].

Retinal arterial vessel occlusion
Retinal arterial occlusion (RAV) is an infarction of the somata of the optic nerve axons, which are part of the central nervous system. There is an acute, marked visual deterioration in the affected eye [6]. In 90% of cases, RAV is the result of an associated internal disease such as hypertension, hyperlipoproteinemia, diabetes mellitus, carotid stenosis, or cardiac disease. A diagnosis regarding these diseases is therefore necessary to prevent further circulatory disorders in other organs as well. The likelihood of suffering a complication such as stroke or myocardial infarction within a week of an RAV is increased by a factor of 44.5 [7]. There is no assured therapy of the RAV.
An important differential diagnosis, although causative in only 5% of cases, is vascular occlusion in the setting of temporal arteritis. In this case, there is a risk that the other eye will also be affected within a short time. In addition to the deterioration of vision, other symptoms such as new headaches, thickened temporal arteries, fever, night sweats or an unwanted loss of body weight are also noticeable. The appropriate laboratory diagnostics should definitely be performed if this inflammatory genesis is suspected. Thus, after the diagnosis of RAV has been confirmed by an ophthalmologist, the primary care physician or internist in particular is called upon regarding the treatment of the underlying condition.
Conclusion for practice
Since many eye diseases are age-related and not all diseases lead directly to visual impairment, regular routine ophthalmologic examinations are necessary to avoid late complications. Acute, persistent, and significant visual deterioration must be evaluated promptly by an ophthalmologist to avoid late effects.
Literature:
- Nüssle S, et al: Diagnostic procedure in angle closure glaucoma by non-ophthalmologists. In: Poster contribution DOG 2019 Berlin; 2019.
- Wenzel M, et al: Survey of BDOC, BVA, DGII and DOG on outpatient and inpatient intraocular surgery: results for 2017. Ophthalmosurgery 2018; 30: 255-266.
- Pascolini D, Mariotti SP: Global estimates of visual impairment: 2010. Br J Ophthalmol 2012; 96(5): 614-618.
- Schwartz S, et al: The effect of cataract surgery on postural control. Invest Ophthalmol Vis Sci 2005; 46(3): 920-924.
- Hammes HP, Lemmen KD, Bertram B: Diabetic retinopathy and maculopathy. Diabetology 2018; 13(Suppl 2): 222-229. www.deutsche-diabetes-gesellschaft.de/fileadmin/Redakteur/Leitlinien/Praxisempfehlungen/2018/DuS_S2_2018_Praxisempfehlungen_16_Diabetische-Retinopathie.pdf, last accessed: 07/25/19
- Lang GE, Lang SJ: Arterial vascular occlusions of the retina. Klin Monatsblätter Für Augenheilkd 2018; 235(1): 109-120.
- Park SJ, et al: Risk and Risk Periods for Stroke and Acute Myocardial Infarction in Patients with Central Retinal Artery Occlusion. Ophthalmology 2015; 122(11): 2336-2343.e2.
FAMILY PRACTICE 2019; 14(10): 34-35











