Acute treatment of ischemic stroke has made tremendous progress in the past two decades. Clinical research milestones include intravenous thrombolysis (IVT) and mechanical recanalization. IVT is performed after ruling out hemorrhagic infarction and other contraindications. The time limit has now been extended to 4.5 hours. In 2015, several studies demonstrated the superiority of mechanical recanalization over conservative therapy in patients with proximal anterior circulation vascular occlusions. In both IVT and mechanical recanalization, the major challenge is to optimize structures and processes in order to realize rapid reperfusion in everyday clinical practice, even outside of trials.
In industrialized nations, stroke is the most common cause of acquired persistent physical disability. The cost to the health care system of the consequences of stroke is substantial. While only a small proportion of strokes are due to intracerebral hemorrhage, the vast majority have an ischemic genesis (85-90%).
Acute treatment of ischemic stroke has made tremendous progress in the past two decades. In this context, milestones of clinical research are mainly the demonstration of the efficacy of intravenous thrombolysis in 1995 [1] and mechanical recanalization in 2015 [2]. Rapid restoration of perfusion in the affected vascular territory is the goal of both strategies. Intravenous thrombolysis requires relatively little technical and personnel effort, whereas interventional treatment can only be performed by a well-established, highly specialized interdisciplinary team in a center hospital. The impressive results of the corresponding studies justify this effort in proximal vascular occlusions.
Intravenous thrombolysis
Intravenous thrombolysis (IVT) with tissue plasminogen activator (tPA) has been an integral part of acute therapy for ischemic stroke for 20 years. The efficacy of this therapy has subsequently been repeatedly confirmed [3–5]. Therapy is administered i.v. over 1 hour at a dose of 0.9 mg/kg body weight (maximum dose 90 mg) after ruling out hemorrhagic infarction (e.g., by native cranial CT) and other contraindications, with 10% of the dose given as a bolus at baseline. The original time limit of starting therapy up to a maximum of three hours after symptom onset has since been extended to 4.5 hours [4]. However, despite the extension of the time window, it should be remembered that the success of therapy is clearly time-dependent, and there should be no delay in therapy under any circumstances [5]. The more time that elapses from symptom onset to therapy, the less the patient benefits and the higher the risk of severe complications.
Recommendations of the DGN on IVT
Based on the current study situation, recommendations were added to the guidelines of the German Society of Neurology (DGN) [6]. These relate firstly to the use of IVT outside established approval criteria and secondly to mechanical thrombectomy. The most important recommendations will be briefly discussed below. What is new is that the recommendations for IVT no longer specify an upper age limit. In patients treated with oral anticoagulation, treatment outside of the approval criteria may be considered under certain circumstances when the risk of bleeding is acceptable:
- under treatment with vitamin K antagonists with an INR value up to 1.7;
- under new oral anticoagulants, if the diluted thrombin time or factor Xa level are normal or the patient has not taken the medication in the last 48 hours with normal renal function.
Starting therapy up to six hours after symptom onset does not seem to lead to a significant increase in the complication rate and can therefore be considered in individual cases (e.g., mismatch imaging, collateral imaging). Lysis therapy can also be performed in the presence of so-called early signs of infarction in the 4.5-hour time window.
In summary, IVT has few complications in the hands of a neurologist familiar with the therapy, in combination with acute care of the patient in a stroke unit, and with attention to absolute contraindications.
Endovascular therapy
Despite the undisputed success of IVT, the relatively low rate of vascular recanalization, especially in proximal occlusions, has prompted the search for alternative methods [3,7]. Following the established endovascular therapy procedures in cardiology, various attempts have been made to achieve a higher recanalization rate and thus a better clinical outcome by means of direct access to the thrombus. In the process, there were some setbacks, which, however, led overall to a significant improvement in the initially applied technique. Among others, local intra-arterial lysis using urokinase, which was first systematically studied in the PROACT trial, did not receive approval in the United States due to insufficient clinical benefit [8]. This process was subsequently abandoned in favor of purely mechanical methods. Permanent stent placement over the area of vessel occlusion increased the recanalization rate but led to increased hemorrhagic complications, mainly due to the dual antiplatelet therapy required following the intervention [9]. Intracranial stents are therefore only used in exceptional cases in clinical practice.
In 2013, three clinical trials were published that investigated recanalization procedures for proximal cerebral vascular occlusion in which the thrombus was removed mechanically (Interventional Management of Stroke III [10], MR RESCUE [11], SYNTHESIS Expansion [12]). These studies also failed to demonstrate superiority of endovascular therapy over drug therapy alone. Three weak points for the failure of these studies can be identified, which were not only avoided in subsequent (successful) studies, but from which implications for daily clinical practice can be derived:
- First, there were sometimes drastic delays until the actual vascular opening, which was probably mainly due to the fact that the processes from the arrival of the patient to the intervention did not work efficiently enough.
- Second, inadequate patient selection occurred, mainly due to inadequate imaging. In particular, there was a failure to expeditiously identify eligible patients with a main stem occlusion and to exclude patients with an extensive infarct core from the study.
- Third, recanalization success was relatively low even in suitable patients because of the use of older thrombectomy procedures. In particular, the stent retrievers that were later so successful were used only sporadically.
The aforementioned weaknesses were addressed in subsequent studies and led to impressive results in the trials finally published in 2015 (Figs. 1 and 2) . MR-CLEAN was the first randomized controlled trial to clearly demonstrate a benefit of mechanical thrombectomy [2]. As a direct consequence, interim analyses were performed in other ongoing trials (ESCAPE [13], EXTEND-IA [14], REVASCAT [15], SWIFT PRIME [16]), which led to study termination at all centers because mechanical recanalization was already clearly superior to conservative therapy at this point.
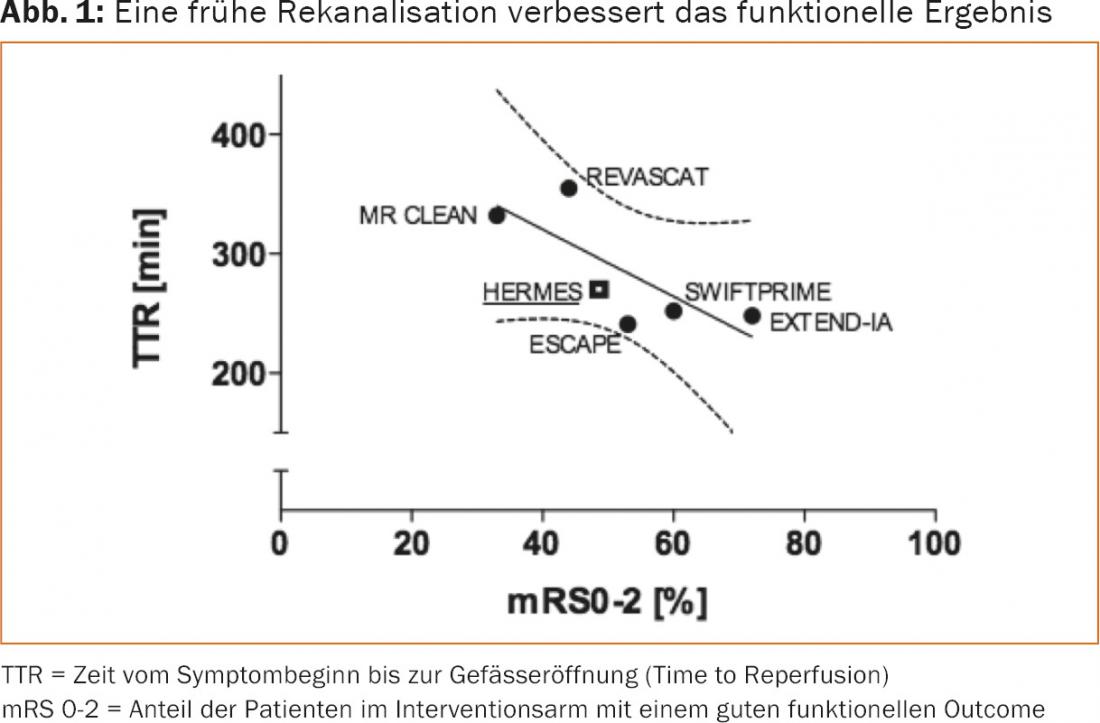
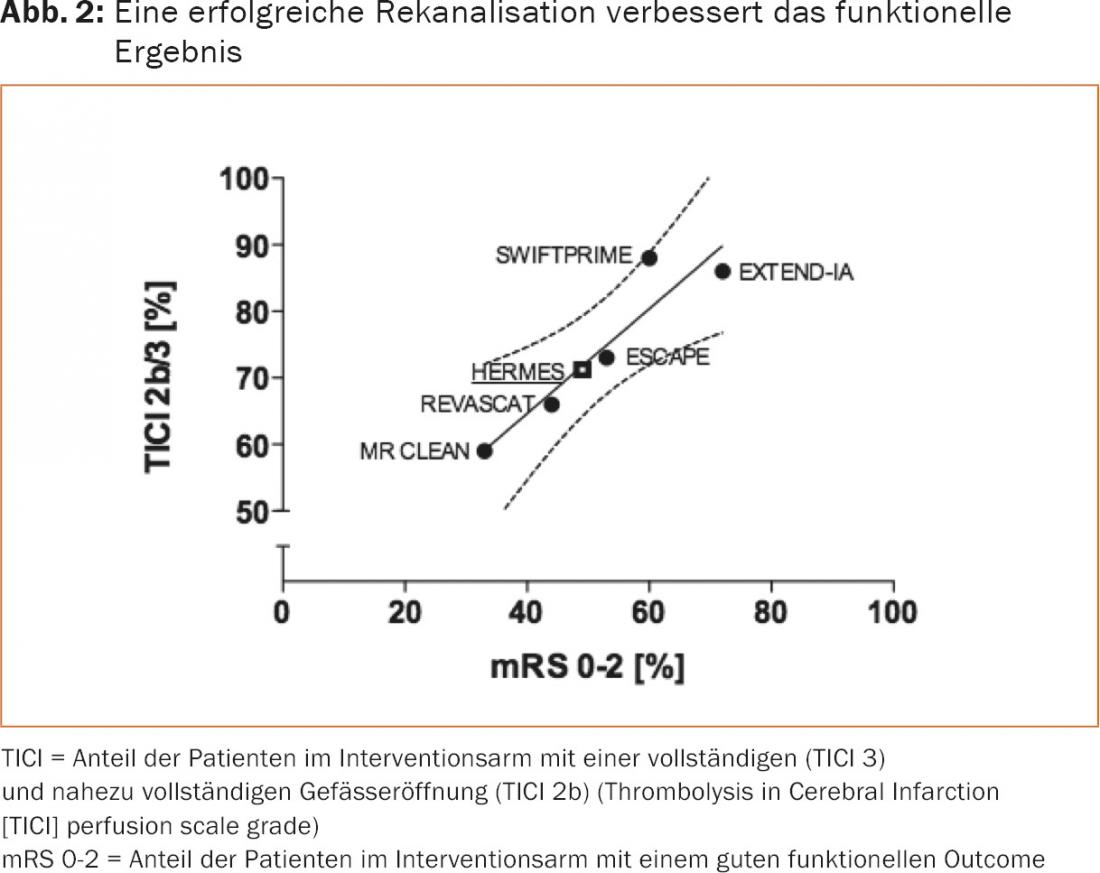
Apart from some differences in study design, which cannot be discussed in detail here, the studies show relevant similarities in essential points: Patients with proximal vessel occlusions (carotid T and M1) and severe clinical deficit were specifically selected, hospital procedures were optimized for rapid recanalization (median time to groin puncture 210-270 minutes), and stent retrievers (81-100%) were mainly used. In some cases, patients with early demarcated large infarcts were also excluded. These factors resulted in significant improvement in clinical outcome and reduction in mortality at 90 days compared with control groups due to the high recanalization rates (TICI2b/3: 59-88%) with few complications (symptomatic intracranial hemorrhage: 0-8% ) (Table 1).
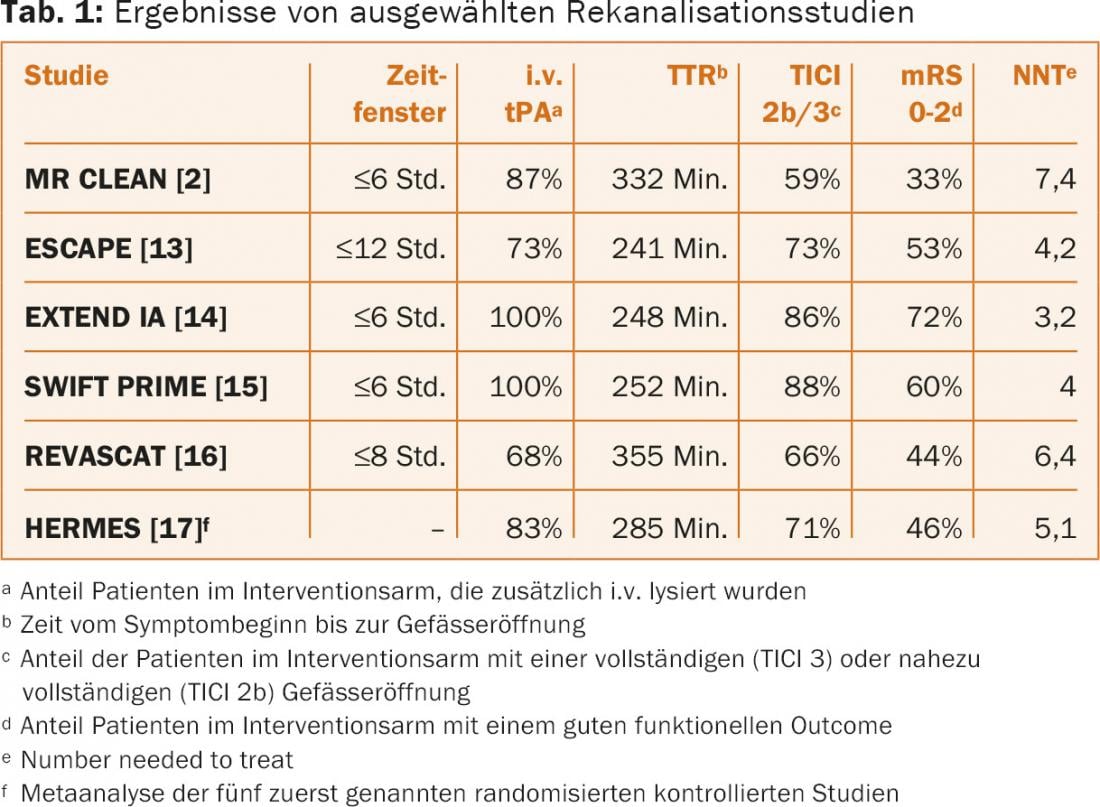
The results of the above studies were recently examined in a pooled meta-analysis [17]. This showed that mechanical thrombectomy has a clear benefit in almost all patients with proximal vascular occlusions of the anterior circulation regardless of other factors (such as age).
Recommendations of the DGN for mechanical recanalization
As a consequence of the above-mentioned studies, the DGN guidelines for the treatment of ischemic stroke have now also been supplemented by recommendations, which are briefly summarized below.
Vascular Imaging: Vascular imaging (CT-A or MR-A) should be performed immediately to allow rapid and meaningful selection of appropriate patients.
Time Frame: Mechanical recanalization is recommended for proximal anterior circulation vessel occlusions up to six hours after symptom onset. An extension of the time window beyond six hours may be considered in individual cases (e.g., with the aid of mismatch imaging or collateral imaging).
IVT: In the absence of contraindications, IVT should always also be used within 4.5 hours; if this is not possible, mechanical recanalization alone is the first-line therapy. The two therapeutic procedures should complement each other, if possible, and neither procedure should result in a delay of the other. In particular, do not wait for IVT success and delay preparations for mechanical recanalization.
Age limit: There is no general upper age limit.
Duration of clinical procedures: With regard to clinical procedures, it is required that the time from arrival to groin puncture (“door to groin puncture”) should not exceed 90 minutes and the time between groin puncture and vessel opening should not exceed 30 minutes.
Bridging: Patients referred to hospitals without the option of mechanical recanalization should undergo IVT after contraindications have been ruled out and should be promptly transferred to a center hospital for mechanical recanalization while therapy is ongoing (“bridging”).
Results: As a result of mechanical recanalization, complete or near-complete vessel opening should be achieved in more than 75% of patients (Thrombolysis in Cerebral Infarction [TICI]-perfusion scale of grade 3 or 2b).
Quality Assurance: Centers offering mechanical recanalization are required to participate in quality assurance programs and certification.
In conclusion, mechanical recanalization opens new perspectives especially for patients with proximal vessel occlusions in the anterior circulation. A major challenge remains the implementation of structures and processes to realize rapid reperfusion also outside of studies in everyday clinical practice. Above all, it is important to keep the friction losses resulting from the collaboration of three or more disciplines (including emergency medicine, neurology, neuroradiology and anesthesiology) as low as possible, because the one golden rule in the care of acute ischemic stroke remains unchanged: Time is Brain.
Literature:
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995; 333(24): 1581-1587.
- Berkhemer OA, et al: A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372(1): 11-20.
- Rha JH, Saver JL: The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 2007; 38(3): 967-973.
- Hacke W, et al: Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359(13): 1317-1329.
- Emberson J, et al: Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014; 384(9958): 1929-1935.
- Ringleb PA, et al: Acute ischemic stroke therapy-supplement 2015; Recanalizing therapy. www.dgn.org/images/red_leitlinien/LL_2015/PDFs_Download/030140_LL_akuter-ischaemischer-schlaganfall_final.pdf, 2015.
- Lee KY, et al: Early recanalization after intravenous administration of recombinant tissue plasminogen activator as assessed by pre- and post-thrombolytic angiography in acute ischemic stroke patients. Stroke 2007; 38(1): 192-193.
- Furlan A, et al: Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 1999; 282(21): 2003-2011.
- Chimowitz MI, et al: Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 2011; 365(11): 993-1003.
- Broderick JP, et al: Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013; 368(10): 893-903.
- Kidwell CS, et al: A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013; 368(10): 914-923.
- Ciccone A, et al: Endovascular treatment for acute ischemic stroke. N Engl J Med 2013; 368(10): 904-913.
- Goyal M, et al: Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372(11): 1019-1030.
- Campbell BC, et al: Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372(11): 1009-1018.
- Jovin TG, et al: Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372(24): 2296-2306.
- Saver JL, et al: Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke. N Engl J Med 2015; 372(24): 2285-2295.
- Goyal M, et al: Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016: 387(10029): 1723-1731.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(4): 17-20.
HAUSARZT PRAXIS 2016; 11(10): 20-23











