Data on therapeutic immunization for genital herpes were presented at the American Academy of Dermatology Congress in Washington. The effects on viral excretion are promising, but the compound has yet to prove its superiority over placebo in terms of symptom control. Another study examined factors that lead to acne stigma. The authors conclude that there is still a lot of misinformation circulating about the disease, which unfavorably influences the perception of affected individuals.
A randomized phase II study from the venereology field was discussed particularly extensively at the AAD congress. Herein, a therapeutic immunotherapy called GEN-003, composed of two recombinant HSV antigens (gD, ICP4) and a matrix adjuvant, was evaluated in 310 patients with symptomatic genital herpes infection (HSV 2). The issue was dose finding, so both the antigens (30 or 60 μg) and the adjuvant (25, 50, or 75 μg) were varied in amount. Vaccination was administered three times at three-week intervals. The goal was to elicit a robust T- and B-cell immune response with the antigens. In double-blinded fashion, placebo was additionally administered in each case. So there were seven therapy groups in total.
To determine virus excretion, genital swabbing was performed for 28 days prior to the first vaccine dose, then again immediately following the third vaccination, and then after either five or six months or after eleven or twelve months. Patients also kept records of the number of lesions they had during an outbreak.
Six months after vaccination, genital HSV 2 shedding was significantly reduced from baseline in all groups immunized with 60 μg HASV 2 antigen. The greatest reduction was seen in patients who received the 75 μg adjuvant dose at the same time (p<0.0001) – a reduction of 58% was observed. In the lower-dose groups, a significant decrease was found only in the 30/50 μg combination (50%, p<0.0001).
In addition to viral shedding, the researchers collected data on lesions, which decreased by 43-69% in almost all patients (except in the lowest antigen and adjuvant dose group) compared to baseline over the entire period (p<0.0001). However, the number of lesions also decreased in the placebo group (in contrast to viral shedding), suggesting either that patients expected a decrease and therefore recorded it accordingly, or that the follow-up duration of six months was simply too short to show clearer differences. Data after one year were not yet available at Congress. The safety profile was acceptable, according to the study authors. Most side effects were mild and included myalgia, fatigue, and redness or swelling at the injection site.
Placebo effects urge restraint
Vaccination in this area would represent a completely new therapeutic approach. Currently, there is no way to permanently eliminate the virus from the body, which can always lead to reactivation and thus painful genital lesions. The viruses can be shed in the asymptomatic phase as well as in the reactivation phase, leading to transmission. Antiviral drugs are used predominantly in the symptomatic phase, but sometimes also continuously in the sense of preventive suppressive therapy for recurrent forms. For the first time, a vaccination has now achieved a significant viral decline and symptom reduction over a period of six months after administration. The highest dose combination was the most effective. It should be noted that this is a therapeutic and not a prophylactic vaccination. At a later date, research into the prophylactic potential of the compound is also conceivable, the study authors said.
The reactions to the results were predominantly positive. However, some experts warned against overestimating the effects. A reduction of almost 60% in viral shedding is indeed clinically relevant, as it reduces the risk of transmission. However, for the patient, the symptoms and signs of the disease would be more important than asymptomatic viral shedding. The fact that the patients also showed a decrease in lesions under placebo is a clear limitation that must be eliminated in the future.
Acne – a stigma with profound psychosocial consequences
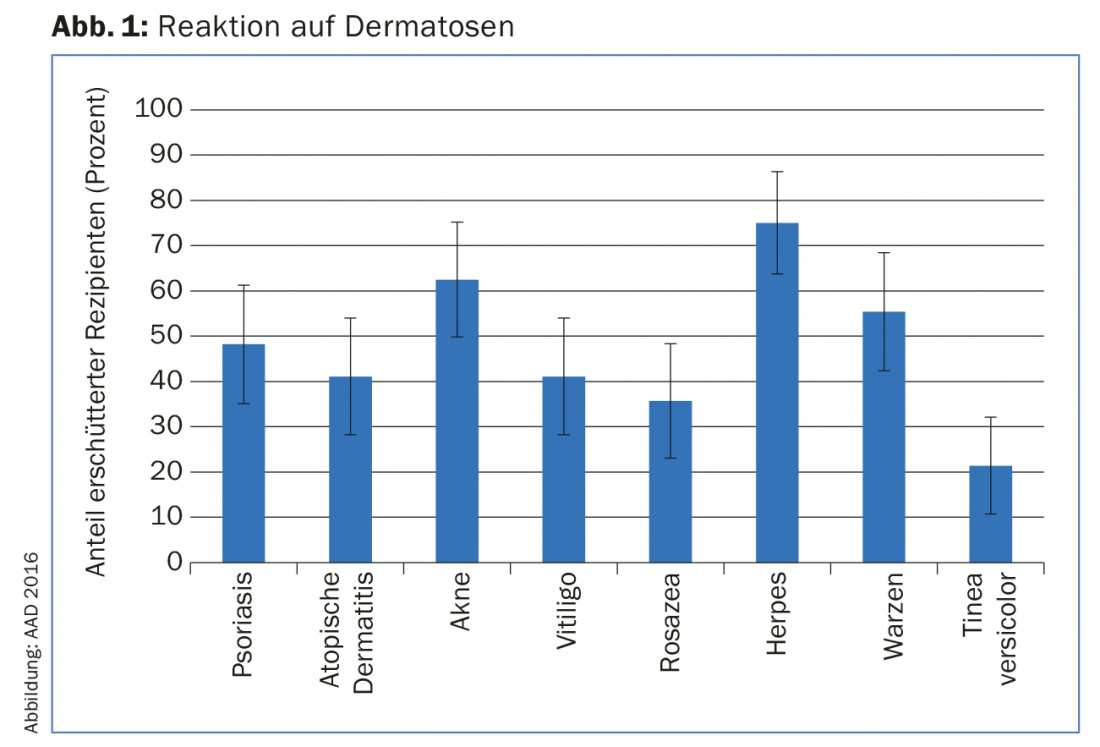
A lecture on acne vulgaris provided food for thought. Fifty-six healthy subjects were shown images of various dermatoses, including psoriasis, vitiligo, rosacea, herpes, warts, tinea versicolor, atopic dermatitis, and acne. Afterwards, they had to fill out a questionnaire describing their reactions to the pictures and their perception of the disease in general. The researchers were interested in examining the individual factors that lead to stigma.
Only persons with herpes provoked greater discomfort in the viewers than the acne images (Fig. 1). Herpes upset more than 70% of the recipients, acne 62.5%. Acne was thus significantly different from atopic dermatitis, vitiligo, rosacea, and tinea versicolor (p<0.05). More than half of the people (55.4%) believed that acne was caused by poor hygiene, 37.5% saw a link with diet, and 50% assumed a risk of infection. Recipients were most repulsed by localization, color, and open inflamed lesions. 44.6% would be uncomfortable touching the affected person, 41.4% would not like to be seen with the person in public. 67.9% of respondents said they would feel ashamed if they had acne and would find a counterpart with this condition unattractive. Over 80% felt sympathy for those affected. This value was significantly higher than in all other dermatoses except psoriasis.
Despite this information, only a minority (19.6%) would exclude acne sufferers from social activities, not consider them for employment (14.3%), or separate from them as cohabitants because of it (3.6%).
Eliminate misunderstandings
The authors conclude that acne is perceived as highly stigmatizing, which could be due to a lack of or incorrect knowledge about its etiology (and, surprisingly, the perceived risk of infection) on the one hand, and its localization on the face on the other. Rosacea, also located on the face, is significantly less stigmatizing. Of course, ideas about the disease also influence opinions about sufferers, e.g. people perceive them as “unclean”, unkempt or blame them for the disease because they eat poorly. Lastly, misconceptions transfer back to the sufferers themselves and can lead to a vicious circle, for example, when someone with acne believes they need to clean their skin and causes even more irritation to the skin with intense scrubbing and the use of certain cleansers. Therefore, patients should contact doctors and not retreat with their disease.
Little empathy despite high prevalence
The results are particularly concerning because acne usually develops during a highly vulnerable psychosocial developmental phase, adolescence, and is one of the most common dermatoses of all. Even in adulthood, acne can cause lowered self-esteem and thus problems in work and social life. In view of the high number of people affected, better education of the population about the disease therefore appears to be of central importance. Overall, the authors were surprised that empathy for acne sufferers was very low (except for the aforementioned pity), even though acne is so common and it can be assumed that many of the respondents have gone through the disease themselves.
Studies consistently show that acne may be associated with social dysfunction, psychological disturbance [1], and perceived stigma [2] – in many patients to a far greater extent than is the case with other chronic dermatoses.
News about atopic dermatitis
There was also interesting news to report at the congress in the field of atopic dermatitis (AD): A randomized-controlled phase II study with the monoclonal antibody nemolizumab (anti-interleukin-31-receptor-A) found promising efficacy in 264 patients with moderate to severe AD. Subcutaneously administered nemolizumab is the first therapeutic agent to target interleukin 31. This plays an important role in the pathophysiology of the disease, especially with regard to pruritus [3].
Thus, the substance administered four-weekly for three months reduced pruritus on the visual analog scale (VAS) by 41.5, 61.2, and 60.5% at week twelve, depending on the dose – a significant difference compared to placebo (-20.1%, for all: p<0.01). After only one week, the benefits of the Verum had become visible. On average, the Eczema Area and Severity Index reduced by 44.6% after three months (at the dose of 0.5 mg/kg) vs. 20.9% with placebo. A score on the Investigator’s Static Global Assessment (ISGA) of ≤1 was achieved by 20.9% vs. 4.7% (p=0.0488). The time to fall asleep was also reduced by half and the total sleep time was extended. The most common side effects included AD exacerbation and nasopharyngitis. Overall, however, the substance was well tolerated and caused neither more frequent nor more severe side effects than placebo.
Two Phase III studies on the topical PDE 4 inhibitor crisaborole also produced positive results. In a total of over 1500 patients with mild to moderate AD, the compound produced significant benefits in ISGA. In each case, about half of the patients on crisaborole achieved status 0 (“clear”) or 1 (“almost clear”) at day 29, whereas only 40.6% and 29.7% did so with vehicle (p=0.005 and p<0.001, respectively). Early and lasting effects were also seen with regard to pruritus. Very young patients were included in the study (minimum age 2 years).
Source: AAD 74th Annual Meeting, March 4-8, 2016, Washington D.C. (USA).
Literature:
- Tan JK: Psychosocial impact of acne vulgaris: evaluating the evidence. Skin Therapy Lett 2004; 9(7): 1-3, 9.
- Roosta N, et al: Skin disease and stigma in emerging adulthood: impact on healthy development. J Cutan Med Surg 2010; 14(6): 285-290.
- Szegedi K, et al: Increased frequencies of IL-31-producing T cells are found in chronic atopic dermatitis skin. Exp Dermatol 2012; 21: 431-436.
DERMATOLOGIE PRAXIS 2016; 26(3): 33-35











