The antisynthetase syndromes are a subgroup of the idiopathic inflammatory myopathies and account for approximately 35-40% of cases here. However, if detected in time, the long-term prognosis for affected individuals is relatively good. An expert explained what symptoms to look out for and what the treatment options are.
Antisynthetase syndromes (ASDs) are among the rare diseases with a prevalence of 1.5-9/100,000, and an incidence of 1.25 -2.5/1 million. The median age of onset ranges from 48 to 55 years, with a high spread at first manifestation (from 20 to 80 years). Women are affected more often than men.
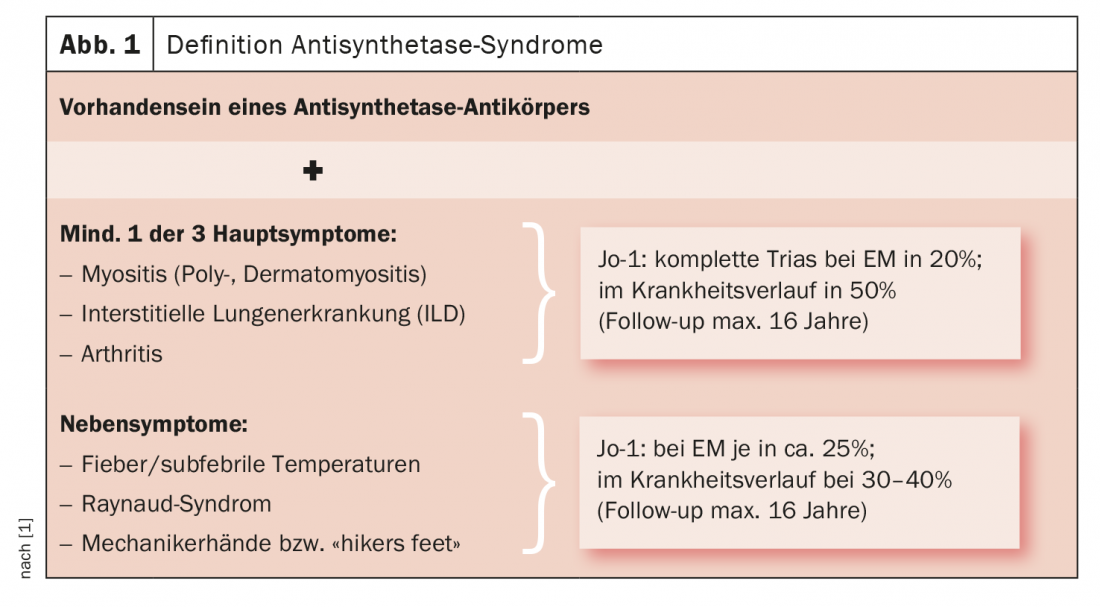
The disease is defined by the presence serologically of an antisynthetase antibody and clinically by a combination of at least one of the three major symptoms myositis, ILD, or arthritis, explained Dr. Jutta Bauhammer, Baden-Baden (D). In addition, secondary symptoms such as fever, Raynaud’s syndrome or skin signs such as the so-called mechanic’s hands may occur (Fig. 1) . At the beginning of the disease, often only some of these organ symptoms are present at the same time. A complete triad of myositis, pulmonary involvement, and arthritis is most common in Jo-1 syndrome, where it is present in only 20% of first manifestations. In the further course, about 50% are then affected, the follow-up is max. 16 years.
Laboratory diagnostics
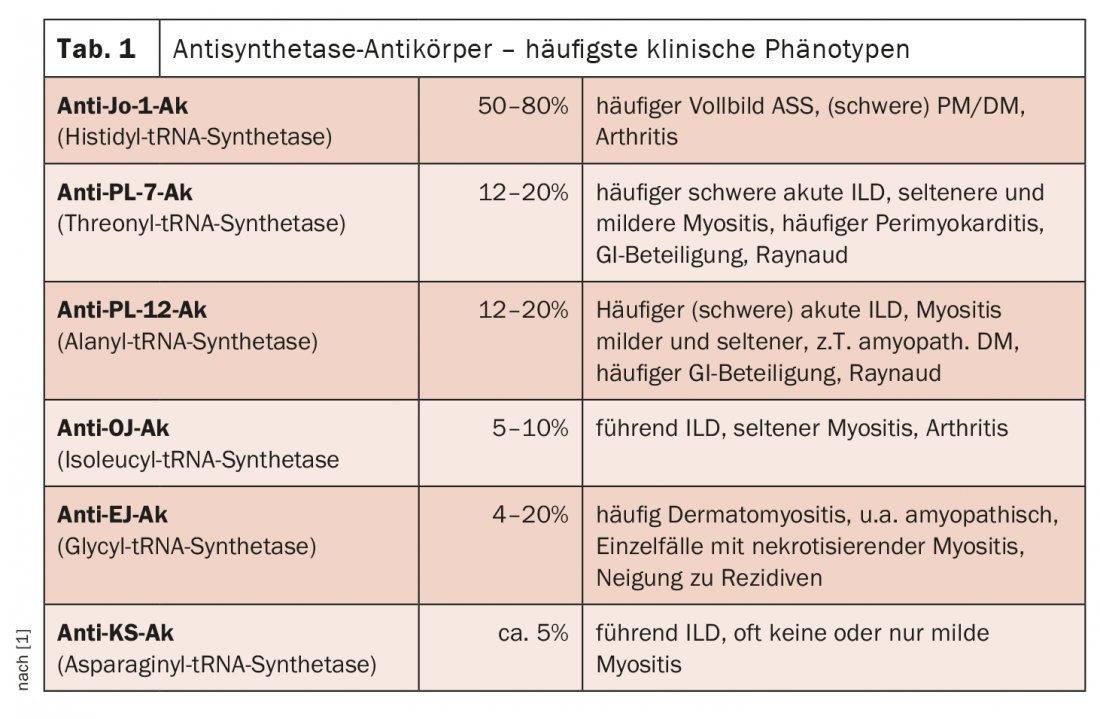
Laboratory chemically known are 11 antisynthetase antibodies (ASS-Ak), but so far only 8 of them have been assigned to the clinical picture of an antisynthetase syndrome (Tab. 1). Target antigens are the aminoacyl-tRNA synthetases, and depending on which one exactly represents the antigen, there are different antibodies. These synthetases are enzymes in the cytoplasm that are involved in translation; they catalyze the binding of an amino acid to its specific tRNA. Generally, there is only one ASS-Ak per patient, they are mutually exclusive. A simultaneous occurrence of several ASS-Ak is considered a rarity. The most common ASS-Ak in Caucasian patients is the anti-Jo-1 antibody, which is present in 50-80% of affected individuals and is directed against histidyl-tRNA synthetase. In this Ak, it is more common to see the full picture of an antisynthetase syndrome (i.e., that all three major symptoms are present with muscle, lung, and joint involvement) with often severe myositis and, in many cases, more severe joint involvement with manifest arthritis.
Organ shareholdings
Myositis is present in 75-80% of cases with Jo-1-Ak, and in about 60% with other antibodies (where the lung is often the leading organ). Clinically, the picture is often one of polymyositis, more rarely dermatomyositis, and concomitant myocarditis is seen in 3-4% of patients. Histologically, one typically sees a dominant inflammation of the perimysial connective tissue, which has an infiltrate of abundant CD68-positive macrophages as a hallmark (“macrophage-dominated myositis”); perifascicular necrosis may occur; capillary density is usually unremarkable. There are also single case reports of necrotizing myositis.
Joint involvement occurs in 70% of Jo-1-Ak and approximately 50% of non-Jo-1-Ak. For Jo-1 antibodies, it represents the first isolated organ manifestation in 20-35%. It is mostly polyarticular-symmetric (70%), also with involvement of the small and medium-sized joints, less frequently oligoarticular (30%). Some patients also have primary inflammatory arthralgias. In distinction to rheumatoid arthritis (RA), these patients are significantly more likely to have concomitant Raynaud’s syndrome (30-50%, RA patients about 10%). “Now it gets even more insidious,” Dr. Bauhammer cautioned, “In rare cases, patients with antisynthetase syndrome can also have positive anti-CCP antibodies, which are actually considered very specific for RA. In a French study, this was the case in 6-9%. When patients with isolated arthritis were examined, they had positive serology of RA in up to 30% (ACPA in 28%). These patients have 100% joint involvement, quite possibly with erosions.
The lungs are one of the organs that determine prognosis. Pulmonary involvement occurs in the form of interstitial lung disease (ILD), i.e. alveolitis or fibrosis, in 60-80% with Jo-1 antibodies, more frequently (>80%) in patients with non-Jo-1 AK. It can be clinically acute (10-30%) with (per)acute onset, rapid progression with possible deterioration within a few days to the need for intensive care or ventilation, frequent fever, and sometimes acute respiratory failure. 40-50% of cases are chronic, with insidious onset and slow progression until relief dyspnea, irritable cough, and pulmonary function limitations develop. 20-25% of patients are asymptomatic with only abnormalities in readings or CT findings. If affected individuals survive the acute phase, the long-term prognosis is the same for all three courses. It should not be ignored that pulmonary hypertension (PH) may also occur in antisynthetase syndromes. This occurs in just under 10% of cases with a Jo-1-Ak and in up to 20% of patients with a non-Jo-1-Ak and can also be independent of the ILD itself, e.g. as “out of proportion” PH, in some cases also as primary PH.
The latency of diagnosis of PH compared to the initial diagnosis of antisynthetase syndrome is very high. In some cases, the diagnosis was not made until PH was well advanced. According to Dr. Bauhammer, this could be mainly due to the fact that physicians think too late about the possibility of pulmonary hypertension. Accordingly, the prognosis is poor when PH occurs. The 3-year survival rate here is only 58%. Compared with patients without PH, those with pulmonary hypertension have markedly decreased DLco/FVC and are more likely to have Raynaud’s and abnormal capillary microscopy.
The skin signs in antisynthetase syndromes are the so-called mechanic’s hands or – when the signs occur on the feet – the “hikers feet” (Fig. 2) . Approximately one third of patients are affected. They are characterized by hyperkeratosis and non-pruritic erythema, especially on the radial-palmar side of the fingers and the palms. In many cases, there are associations with (severe) ILD. The skin lesions regress under systemic therapy; specific local therapy is almost never necessary.
The secondary symptoms of ASA, i.e., Raynaud’s or fever, are present in 30-40% of patients each. Raynaud’s syndrome is generally not as severe as scleroderma, but there are case reports of digital ulcers and even severe acute digital ischemia. Fever is more common in patients who have acute pulmonary involvement. The expert also reported a study that scored a new onset of Raynaud’s, mechanic’s hands, or fever during the course of the disease as a harbinger of an acute episode and/or a new organ manifestation (4-fold risk in Jo-1-Ak).
Therapy
The therapy strongly depends on the organ involvement, i.e. imunsuppressants and steroids are selected according to which organ is affected and in which severity. Accordingly, there is also quite a wide range of drugs that can be used. In interstitial lung disease, which is a prognostically important organ, calcineurin inhibitors in particular have been shown to be very effective, with cyclophosphamide or rituximab also effective depending on severity. Similarly, there are case reports of good response to MMF or IV immunoglobulins, although data on the latter in pulmonary involvement are still scarce. TNF-alpha inhibitors have been used in joint involvement; however, myositis and interstitial lung disease may worsen under them (progression in ≥33%). Since 2020, there is a new option in Germany to use nintedanib in progressive pulmonary fibrosis, which has been approved since March for systemic sclerosis with lung involvement and since July also for chronic fibrosing, progressive other interstitial lung diseases and thus potentially also for antisynthetase patients. According to Dr. Bauhammer’s advice, good accompanying therapy (respiratory gymnastics, physiotherapy) should always be ensured.
Forecast
The myositis course is generally considered milder compared to, for example, the myositis course with SRP antibodies. Those patients who have pulmonary involvement generally have a higher mortality than patients without. Affected individuals with pulmonary involvement in an ASD-even if fibrosis develops-have significantly better survival compared with patients with idiopathic pulmonary fibrosis, even with a UIP pattern on imaging or histology.
Take-Home Messages
- Remember that patient may have ASA, often mono-/oligosymptomatic onset
- Indicative of ASA in isolated arthritis: including Raynaud’s syndrome, anti-Ro52 AK, and/or mechanic’s hands/feet.
- New onset of Raynaud’s, skin signs, fever may predict relapse or new organ manifestation
- Selection of immunosuppression depending on organ involvement, proven in ILD: Calcineurin inhibitors, RIX.
- Do not forget PH screening
- Forecast relatively good
– FomF Rheumatism Nephro Refresher (online), Oct. 29-31, 2020.
Source:
- Lecture “Antisynthetase syndromes“ in the context of the FomF Rheuma Nephro Refresher (online), 29.10.2020.
InFo PAIN & GERIATRY 2020; 2(2): 42-43 (published 10/12/20, ahead of print).











