The number of new infections and mortality rates have been declining for several years in Switzerland and globally, and an increasing number of HIV-infected individuals are receiving adequate therapy. However, disease management in HIV is quite complex and requires consideration of polypharmacy and multimorbidity, among other factors.
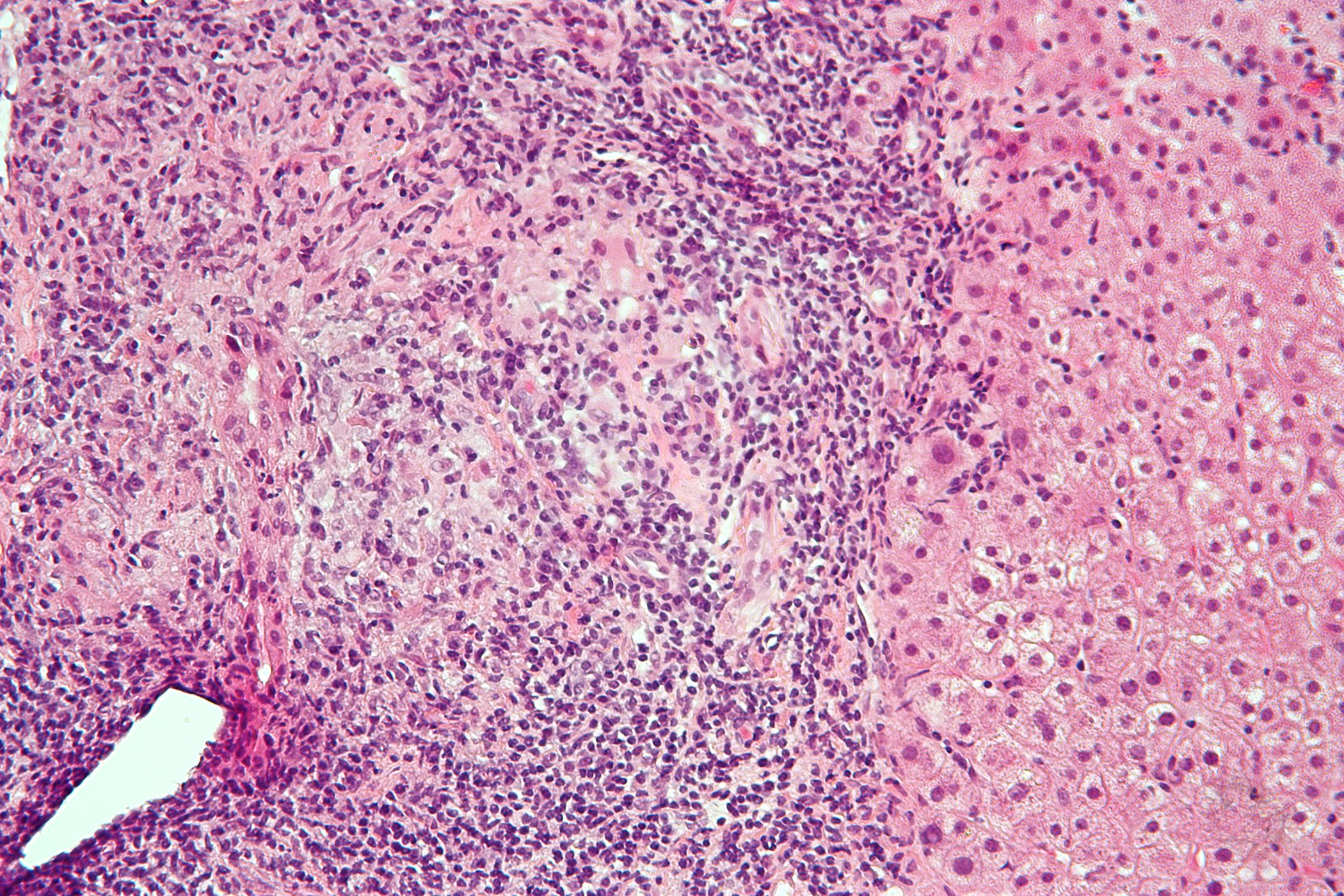
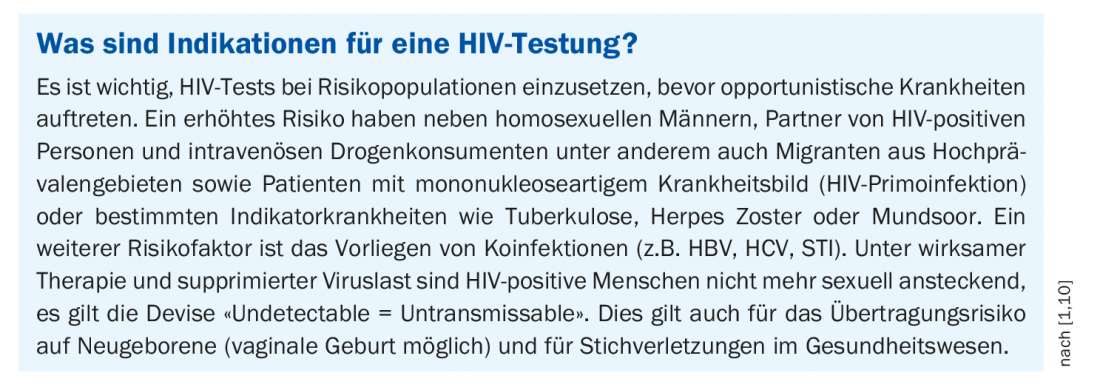
There are an estimated 38 million people living with HIV worldwide, with about half of them living in East and Southern Africa [1,2]. In Switzerland, it is estimated that there are 20,000 cases. In 1983, researchers succeeded in isolating HIV, which had first appeared a few years earlier, and HIV tests were available shortly thereafter [1]. An HIV-positive test result does not equate to AIDS. The diagnosis AIDS (“Acquired Immune Deficiency Syndrome”) refers to a specific symptom complex that represents the final stage of an infection with the HI virus. The T-helper cell count (CD4+ T-lymphocytes) in the blood of HIV-infected individuals serves as a measure of the destruction of the immune system. The immunodeficiency resulting from the demise of CD4 cells produces a high susceptibility to AIDS-defining opportunistic infections and/or tumors. Nowadays, HIV infection is a chronic disease that cannot be cured but is easily treatable, and the average age of patients is significantly higher than in the past, explained PD Anna Conen, MD, MSc, Senior Physician, Department of Infectious Diseases and Hospital Hygiene, Aarau Cantonal Hospital [1]. Prevention efforts remain a priority, at-risk groups should be tested (box) , and all HIV-infected persons should receive adequate therapy to prevent disease progression, improve quality of life, and prevent new infections.
With regard to treatment options for HIV infection, a breakthrough was achieved in the mid-1990s when the first active substances from the group of HAART (“Highly Active Anti-Retroviral Therapy”) came onto the market, the so-called protease inhibitors. Since then, a 70% reduction in mortality has been achieved [1]. Just a few years earlier, AIDS was among the leading causes of death among 25-44 year olds.
ART/HAART: increased convenience thanks to combination products
Currently available antiretroviral therapy for HIV infection uses a combination of agents from different classes and is lifelong (box) [3]. The goal of HIV therapy is complete virological suppression, so that the HI virus is no longer detectable in the blood. This should prevent disease progression and thus improve life expectancy and quality of life. At a virus level of <20 copies/ml blood, transmission is considered eliminated (“Undetectable = Untransmissable”). This is accompanied by a recovery of the immune system (increase in CD4 cells).
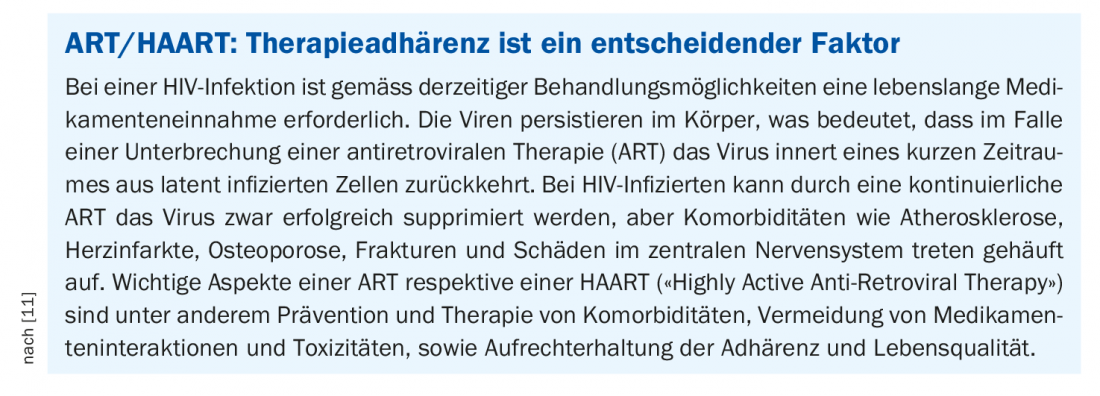
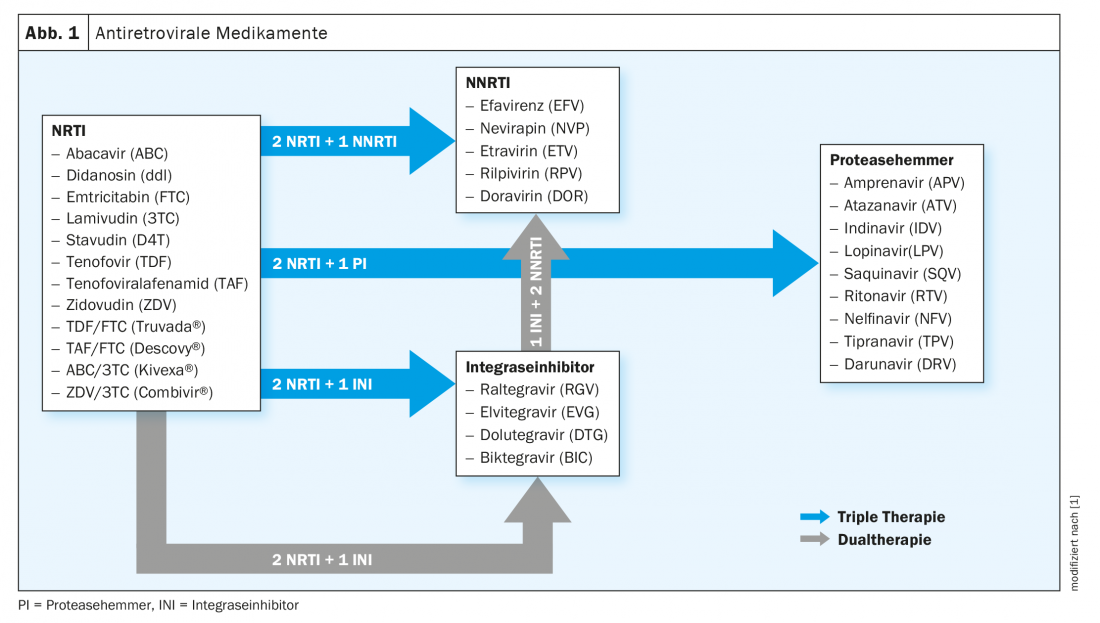
Over the years, antiretroviral agents with improved efficacy, tolerability, and more favorable pharmacokinetic properties have been developed. Nowadays, substances with different targets in the viral replication cycle are available (Fig. 1). Convenience of treatment has improved considerably with the introduction of combination drugs. In 2012, Atripla® was the first combination product to receive marketing authorization in Switzerland, followed by Symtuza® and Juluca® in 2019 and Delstrigo® and Dovato® [1,4] in 2020.
Timely treatment prevents disease progression
In the past, there was confusion about when to start treating patients using antiretroviral therapy (ART). Today, the rule is that every HIV-positive patient, regardless of immune status, receives such therapy, Dr. Conen emphasizes, pointing out that opportunistic infections are to be expected not only when CD4 counts are high, but also when therapy is delayed for a long time and the cut-off values of the CD4 cell count are set too low [1]. On the other hand, toxicity is lower with a longer therapy-free period. Since the HIV therapies available today are well tolerated, there is no longer any reason to delay treatment due to potential toxicity, she said.
Specifically, since 2013, the cut-off value for initiation of therapy according to WHO has been a CD4 cell count <500/µl, regardless of clinical stage [5]. This is based on data from cohort studies, which have shown that the benefits of starting therapy at this time outweigh the potential risks by slowing disease progression and the associated risk of mortality. In addition, early initiation of ART was shown to reduce the risk of sexual transmission to an HIV-negative sex partner [5]. Patients with certain comorbidities such as tuberculosis, hepatitis B (HBV), and pregnancy are advised to initiate ART regardless of clinical presentation or CD4 cell count.
Pre-exposure prophylaxis also provides effective protection
Taking HIV medications prophylactically is also an effective method. The fact that pre-exposure prophylaxis (PrEP) is very effective when taken reliably is considered proven . For HIV PrEP in negatively tested persons at significant risk for HIV, either tenofovir diproxil (TDF) or emtricitabine (FTC) can be used as a combination pill [1,6]. Pre-exposure prophylaxis (HIV PrEP) is recommended for at-risk individuals, and post-exposure prophylaxis (HIV PEP) can be administered within 48 hours of high-risk situations.
The incidence of newly diagnosed HIV cases among homosexual men has decreased markedly since PrEP was introduced. The efficiency of daily PrEP is estimated to be 99% when taken correctly [1,7,8]. According to Chow et al. in studies, the number of treatments needed to prevent one HIV infection is in the range 12-60 [9].
PrEP protects only against HIV, but not against other STIs. Simultaneous use of condoms is recommended, but this does not correspond to reality, the speaker said. Regular screening for STI (gonococci, chlamydia, syphilis, hepatitis C) is advisable. Drug-related side effects of PrEP include proximal tubulopathy, osteoporosis, gastrointestinal distress, and headache. If PrEP is taken with an existing HIV infection, resistance to TDF/FTC may occur.
Manage comorbidities and drug interactions
HIV-infected individuals have a clustered prevalence of lymphoma, anal carcinoma, liver carcinoma, cardiovascular disease, chronic renal failure, osteopenia, and osteoporosis [1]. “We manage cardiovascular risk factors, we optimize calcium and vitamin D supplementation to prevent osteoporosis, we try to manage metabolic complications through therapy adjuncts and secondary medications,” explained Dr. Conan [1]. Quite a few HIV patients present with hepatic complications due to multiple substance use, including alcohol, or prior hepatitis B or C.
Pharmacokinetic interactions of antiretroviral drugs must be kept in mind because metabolization occurs via the cytochrome (CYP) system of the liver. This implies a potential for interaction with psychotropic drugs, statins, anticoagulation, hormonal contraceptives, antibiotics, herbal drugs, among others. Because absorption of antiretroviral agents occurs with the help of gastric acid, PPIs should not be prescribed when taking rilpivirine (Eviplera®, Odefsey®) or atazanavir (Reyataz®). To review potential drug interactions, the following database can be consulted: www.hiv-druginteractions.org
Literature:
- Conen A: HIV today. PD Anna Conen, MD, MSc. FOMF Internal Medicine Update Refresher (Livestream), Dec. 03, 2020.
- BAG: www.bag.admin.ch
- Stellbrink H-J: Antiretroviral therapy of HIV-1 infection. The Internist 2012; 53: 1157-1168.
- Swiss Drug Compendium, https://compendium.ch
- WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations or a public health approach. 2013.
- Swissprepared.ch, www.swissprepared.ch
- Molina J-M, et al: On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med 2015; 373: 2237-2246. DOI: 10.1056/NEJMoa1506273.
- Mc Cormack S, et al: Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet 2016; 387; 10013: 53-60.
- Chow EPF, et al: Decline in new HIV diagnoses among MSM in Melbourne. The Lancet 2018; 5(9): E479-E481.
- Tarr P, et al: HIV infection. Switzerland Med Forum 2015;15(2021): 479-485.
- Behrens G: The future of HIV medicine: a critical appraisal. Dtsch Arztebl 2015; 112(23); DOI: 10.3238/PersInfek.2015.06.05.04
HAUSARZT PRAXIS 2021; 16(1): 24-25 (published 1/25/21, ahead of print).