The incidence of tumors in the head and neck region is increasing. This is often caused by infections with the human papilloma virus 16 (HPV16). However, the prognosis of patients with HPV6-associated carcinomas is significantly better than that of patients with tumors caused by alcohol and tobacco abuse. This change in circumstance has also changed the demands on therapies: less toxicity and better tumor control are required. At this year’s ASCO Congress in Chicago, renowned speakers provided information on trends in screening and therapy of tumors in the head and neck region.
There are over 100 different types of human papilloma virus (HPV), of which about a dozen are oncogenic. These HPV are primarily responsible for cervical and genital cancers, and HPV16 also causes head and neck cancers (HNC). The incidence of HPV-associated HNC has been increasing significantly for several years: HPV-associated HNC will soon be more common than invasive cervical cancer in the US.
HPV-associated tumors have a better prognosis
Stephen Schwartz, MD, Seattle, USA, emphasized in his presentation the differences between HPV-associated HNC and HNC occurring independently of HPV (Table 1); the most important difference is probably the better prognosis of HPV-associated HNC.
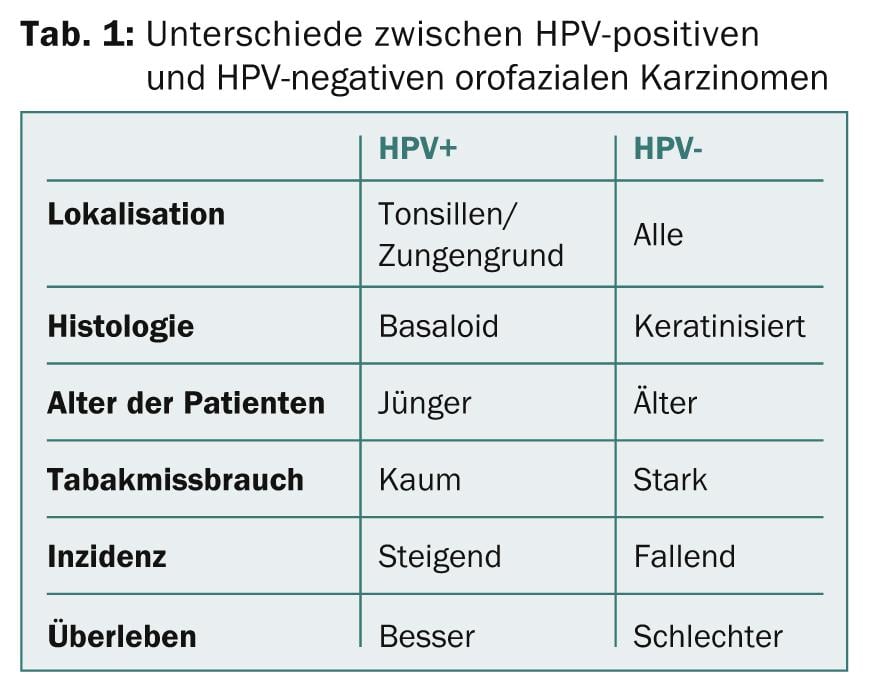
The association between HPV and better survival rates is very strong, for all treatments applied. The question arises as to how this “HPV advantage” can be used in the care of patients. The goal is to use less toxic therapeutic regimens without reducing patient survival.
Several studies are currently underway to test therapeutic regimens in patients with HPV-associated HNC. In the ECOG 1308 trial, patients were treated with low-dose radiotherapy + cetuximab or normal-dose radiotherapy + cetuximab after tumor resection. In the study arm with the low-dose radiation (n=62), overall survival (OS) was 90% and progression-free survival (PFS) was 80%; in the study arm with the normal dose of radiation, OS was 87% and PFS was 65%. Other studies have examined different drug therapies (cituximab vs. cisplatin), different radiation doses, or radiation plus chemotherapy vs. radiation without chemotherapy.
The speaker’s preliminary conclusion:
- HPV16 is a cause of HNC.
- HPV-associated HNC are the most common form of HNC in the United States.
- There is evidence that HPV vaccination can prevent oral infection with HPV. As a physician, one should therefore encourage patients to inform their children resp. Have grandchildren vaccinated against HPV.
- HPV16 infection is associated with a better prognosis of HNC.
- There is limited evidence to date from randomized-controlled trials that a patient’s HPV16 status should influence the choice of therapy. In the coming years, various clinical trials will provide more evidence in this regard. There is hope that HNC patients with HPF16 infection can be treated with reduced toxicity in the future.
Nasopharyngeal carcinomas: is screening useful in China?
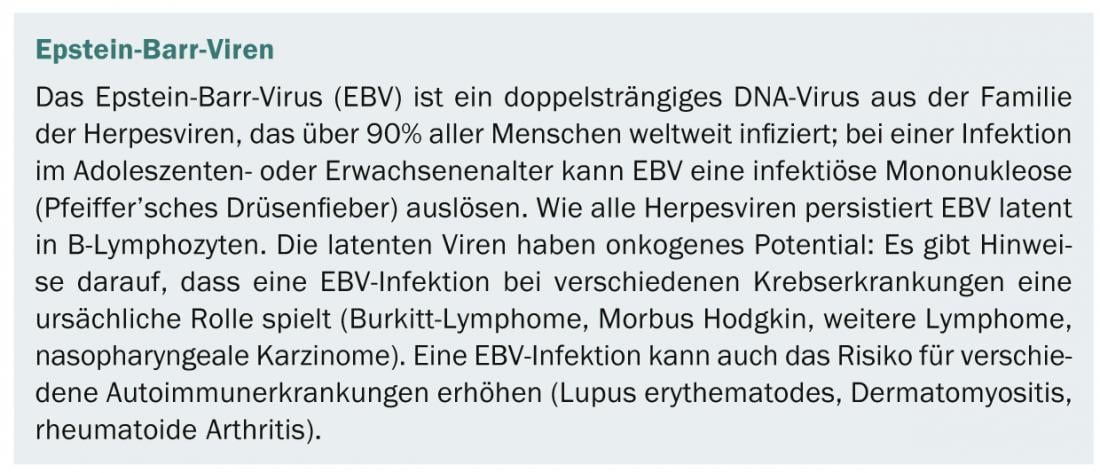
A lecture by Anthony Tak Cheung Chan, MD, Hong Kong, presented recent research on screening and treatment of nasopharyngeal carcinoma (NPC). NPC are endemic in southern China with an incidence of up to 30 /100 000 persons. Progress has been made in the treatment of localized disease in recent years (5-year survival 80-90%), but metastatic NPC is unfortunately still common. In southern China, NPC represent the seventh leading cause of death. More than 90% of all NPC worldwide are associated with Epstein-Barr virus (EBV) infection (box ). Great efforts are being made to decipher the pathogenetic links between EBV infection and carcinogenesis, with the aim of improving the treatment of affected patients in the future.
Because early diagnosis of NPC increases survival rates, different methods are being tested for NPC screening in high-risk patients. Serological EBV analyses are less suitable for this purpose, as false-positive results are relatively frequent. For this reason, screening is based on EBV DNA in plasma. EBV DNA is a sensitive marker for NPC because tumor cells continuously produce and release EBV DNA into plasma. A related study in Hong Kong with 1318 participants showed a positive screening result (persistently high or increasing EBV DNA titers over several weeks) in 96 (5.2%) individuals, and subsequent nasal endoscopy detected early-stage NPC in three of these.
To confirm these results, a much larger study involving 20,000 participants (men between the ages of 40 and 60) is now being conducted. If their EBV DNA titers are persistently high more than two weeks apart, they undergo nasal endoscopy. In addition, the men complete questionnaires on general health, and follow-up by telephone calls is planned for ten years. The study started in July 2013. To date, 5000 participants have been recruited, and 53 had persistently high EBV DNA titers. Ten study participants were found to have NPC (8 stage I, 1 stage II, 1 stage III).
The therapy of an NPC depends on the stage. Stage I tumors are usually treated with radiation only, stage II tumors are treated with radiation and/or additional chemotherapy, and patients with stage III and higher tumors receive chemoradiotherapy. Whether patients with higher tumor stage can benefit from adjuvant chemotherapy is not yet clear. A study from China showed no survival benefit of adjuvant chemotherapy. One research goal would be to identify patients who are at high risk for developing distant metastases and therefore could benefit most from adjuvant chemotherapy. Measurement of EBV DNA titers after chemoradiotherapy could possibly serve as a tumor marker here. One study showed that patients who had persistently high EBV DNA titers (>500 copies, indicating residual tumor disease) 6-8 weeks after chemoradiotherapy had significantly worse survival rates than patients with a value <500. A phase III trial is now underway in Hong Kong in which only patients with persistently high EBV DNA titers will receive adjuvant chemotherapy after chemoradiotherapy. Further studies are investigating EBV vaccines for tumor therapy.
Tumors in the oropharynx: What are the benefits of microsurgery?
About 13,000 cases of oropharyngeal cancer are diagnosed each year in the United States, John A. Ridge, MD, Philadephia, USA, said in his presentation. About one-third of disease is primarily due to tobacco and alcohol abuse; it has a poor prognosis, with a 3-year progression-free survival of 45%. Two-thirds of cases are caused by HPV infection. The prognosis of these patients is significantly better with a 3-year progression-free survival of 75%. Various methods are available for treatment – only tumor resection and radiotherapy can have a curative effect. Both methods have advantages and disadvantages (Table 2).
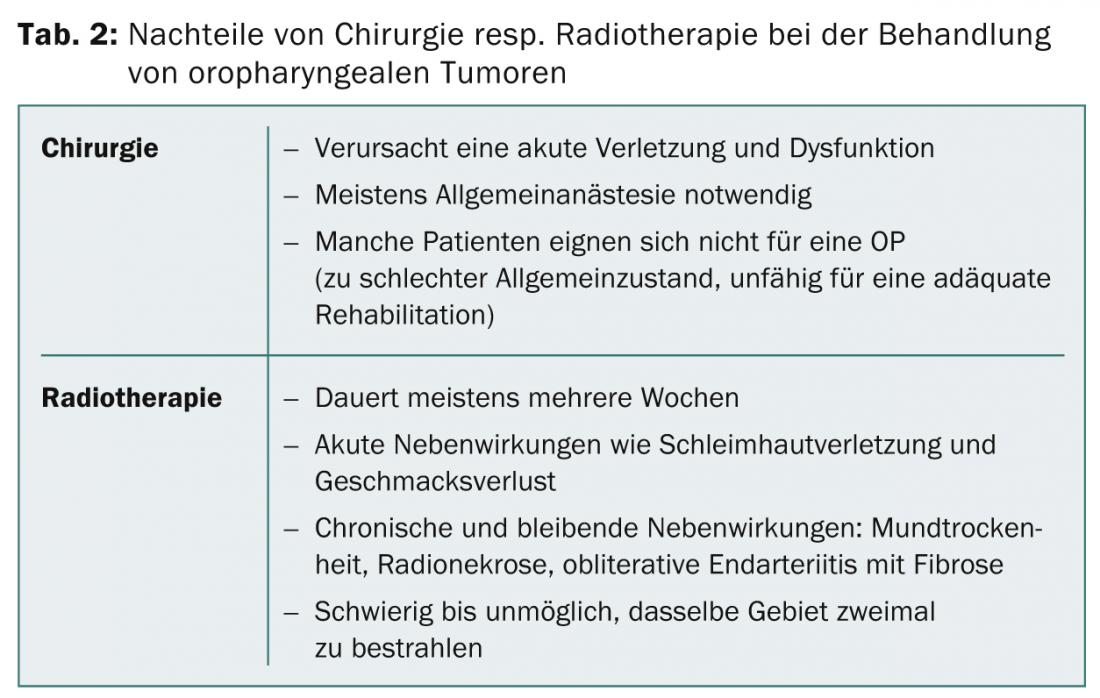
However, even successful therapy often leaves the patient with significant cosmetic and functional limitations. In an effort to treat with as little organ damage as possible, attention has been focused in recent years primarily on non-surgical methods. The side effects of radiotherapy resp. of combined radio- and chemotherapy are not insignificant for patients, however, and these forms of therapy are often unsuccessful in patients with tumors due to substance abuse. Therefore, in the search for optimal treatment regimens, two “new” goals should not be forgotten:
- Improving tumor control in HPV-negative disease: increased locoregional tumor role by resection; survival rates and functional outcome comparable with chemoradiotherapy.
- In patients with HPV-associated tumors, reduce toxicity of treatment without reducing survival: Reduce doses of chemoradiotherapy; limit the number of patients who need chemoradiotherapy; evaluate survival rates and functional outcome.
Transoral laser microsurgery (TLM) and transoral robot-assisted surgery (TORS) are two methods that can help achieve these goals. They allow the tumor to be removed through the mouth without damaging the mandible or swallowing apparatus. Currently, there are only a few small studies on TLM and TORS for the therapy of oropharyngeal tumors. Two studies show that quality of life and functional outcome are better after microsurgery followed by radiotherapy than after combined chemoradiotherapy.
TLM followed by radiotherapy can also achieve good local tumor control (5-year tumor control locally 92%, locoregionally 97%), which compares favorably with control by nonsurgical treatment methods. Bleeding is an important complication. A review of 2015 procedures performed by 45 surgeons lists six deaths, all a result of postoperative bleeding. Currently, several prospective studies are underway comparing microsurgical methods with conservative treatment approaches – it is hoped that these studies will confirm the good results of the preclinical studies. The speaker’s conclusion:
- Transoral resection of oropharyngeal tumors, when performed by an experienced surgeon, shows good to excellent oncologic and functional results.
- Optimal selection of appropriately treated individuals may eventually reduce the number of patients requiring treatment with three modalities.
- The benefits of transoral resection need to be confirmed by prospective multicenter studies.
Source: 50th Annual Meeting of the American Society of Clinical Oncology (ASCO), May 30-June 3, 2014, Chicago.
InFo Oncology & Hematology 2014; 2(6): 20-22.
CONGRESS SPECIAL 2014; 5(2): 27-29











