In Basel, experts from various fields of dermatology and allergology discussed, among other things, the innovations in the classification and therapy of urticaria, modern testing methods in the field of IgE-mediated food allergies, and the difficulties in the exact anamnesis of hypersensitive reactions to drugs.
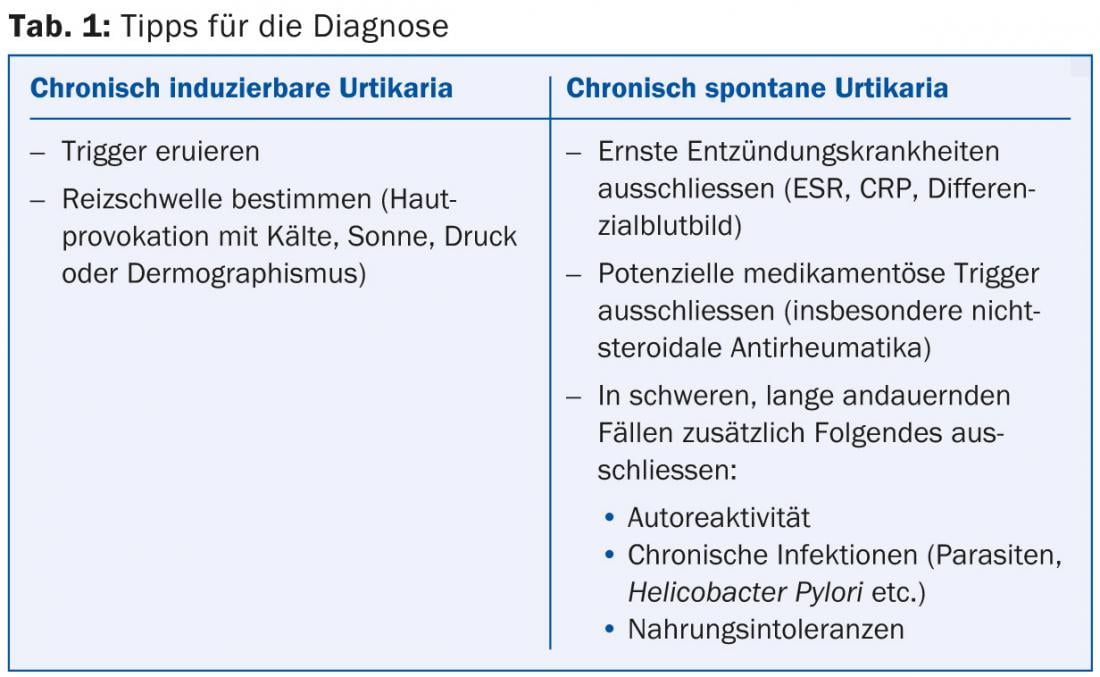
At the beginning, PD Dr. med. Kathrin Scherer Hofmeier from the Allergology Department at the University Hospital Basel spoke about urticaria and angioedema. Until now, spontaneous urticaria with the two subtypes acute and chronic had been distinguished from urticaria of physical origin (e.g., solar, cold-related, etc.) and from other types of urticaria such as the cholinergic form. The fourth international consensus meeting on this topic, held in November 2012, proposed a simplification of the classification: Acute urticaria with a duration of max. six weeks is distinguished from chronic, which may be spontaneous or inducible, making the term “chronic idiopathic urticaria” superfluous. The inducible type includes physical, cholinergic, contact, or aquagenic causes [1]. The diagnostic pathways of chronic spontaneous and chronic inducible urticaria are shown in Table 1.
Therapeutically, the goal in both forms (with or without angioedema) is to control symptoms to a large extent. The new treatment algorithm, unlike the previous guidelines, does not include H2 antagonists, dapsone, sedating agents, or a mix of different antihistamines (Fig. 1).

Food allergy
According to Peter A. Eng, MD, of the Cantonal Hospitals of Aarau and Lucerne, food intolerances can be divided into immunological and non-immunological forms, the former including the IgE-mediated immediate type, which was the main focus of the presentation. “The pathogenesis can be caused by allergen contact with the gastrointestinal mucosa, or it can be caused primarily by sensitization to inhaled allergens (e.g., pollen) and only secondarily to food,” said Dr. Eng. “After a positive food provocation test, immediate reactions (<2 hrs) are often seen: They include urticaria, gastrointestinal, respiratory and, in rare cases, cardiovascular symptoms. By far the majority react through the skin.”
The diagnostic procedure for suspected food allergy proceeds via
- the careful anamnesis
- Skin tests/the in vitro diagnostics
- in special cases, a provocation test.
“On the second point, it should be noted that the skin prick test requires experience on the part of the attending physician. In addition, it requires intact skin in any case and is difficult to perform on young children. One advantage is the immediate results and low cost. Positive points of in vitro diagnostics are that it is not influenced by medication, does not require cooperation and is independent of the skin condition. The disadvantage is the expensive price,” Dr. Eng summarized.
“In any case, the test results must be related to the medical history and clinical findings. Moreover, sensitization does not necessarily mean allergy. Only if the relation to allergic symptoms is clear, allergen abstinence and subsequent re-evaluation after 6-12 months becomes necessary.”
New ways of diagnosis
In the field of cross-reactions, new diagnostic methods are under development: Component-based, molecular-specific diagnostics test more than one hundred allergen components purified from biological raw material or recombinantly produced in a microchip-based multi-immunoassay. Advantages are the accuracy (better differentiation allergy – immunological cross-reaction), the better prognosis (outgrowth or persistence, severity of allergic symptoms) and the thereby in certain cases avoidable provocation tests.
The composition of the more than one hundred allergen components is difficult. Different needs exist depending on the geographic region. “Individual components of the cockroach, for example, are of less interest in Switzerland,” explained Dr. Eng. Furthermore, evaluation of sensitivity, specificity and cut-off points of the individual allergen components is still missing. Moreover, questions of practicability remain: the flood of data may confuse rather than help. Therefore, the test should be prescribed only by allergists who have precise knowledge of the properties and significance of the various allergen components tested.
Drug allergy
“The management of hypersensitive reactions to drugs is one of the supreme disciplines of allergology,” said Prof. Andreas J. Bircher, MD, Chair of the course and Head of Allergology at the University Hospital Basel. A distinction must first be made between dose-dependent (“augmented”, type A) and -independent (“bizarre”, type B) Forms.
In type A, the side effects in question are directly related to the actual pharmacologic drug effects, i.e., they are partly predictable: for example, bleeding from an overdose with anticoagulants or skin atrophy from prolonged use of corticosteroids.
In type B, only sensitized or hypersensitive individuals react, and the dose plays a minor role, so the effect is not directly related to the drug action. Therefore, this form is unpredictable: for example, exanthema when taking antibiotics or urticaria when taking analgesic drugs.
What to consider?
The following five points are important in approaching a hypersensitive drug reaction:
- orphology as accurately as possible: clinical manifestation (analysis of lesions, distribution, development, etc.), possibly histology.
- Obtain current and past medical history as completely as possible
- Trace the chronology as accurately as possible
- Make an appropriate clinical diagnosis (consider differential diagnosis).
- In addition, if necessary, formulate a precise pathogenetic hypothesis (select and interpret adequate, relevant tests).
“Obtaining the patient’s medical history in particular is difficult, as it usually presents as highly unstable: The patient’s memory of past symptoms and episodes of illness may be inconsistent, incomplete, or even incorrect. Separate similar incidents are reflected as general facts mixed up [2].
Therefore, mentally recreating the medications taken offers pitfalls because certain drug names are generalized or confused. For example, the patient generally speaks of penicilin when taking any antibiotics, or aspirin when using any analgesics,” Prof. Bircher said.
Causes and danger signs
Drugs that frequently cause drug side effects are antibiotics and anti-infective drugs, but also non-steroidal anti-inflammatory drugs and analgesics (mainly pseudoallergy, rarely exanthema, photoallergy), anticonvulsants and antihypertensives. Finally, Prof. Bircher summarized the most important danger signs that the attending physician should perceive as alarming in any case (Tab. 2).

Source: 8th Dermato-Allergological Course of the SGDV, October 18, 2013, Basel.
Literature:
- Maurer M, et al: Revisions to the international guidelines on the diagnosis and therapy of chronic urticaria. JDDG 2013; 11(10): 971-978. Article first published online: 19 AUG 2013. DOI: 10.1111/ddg.12194.
- Barsky AJ: Forgetting, fabricating, and telescoping: the instability of the medical history. Arch Intern Med 2002; 162: 981-984.
Dermatology Practice 2013; 23(6): 21-24











