Overall survival of patients with lung cancer has increased by approximately 15% over the past decade. This is primarily due to new therapeutic options, including targeted drugs. However, in order to use these therapies, molecular biomarkers must be determined on a patient’s tumor. The number of tests has therefore also increased significantly in the last five years. Just one exciting topic highlighted at the European Lung Cancer Congress.
Can smoking status determine the efficacy of therapy in EGFR-mutated non-small cell lung cancer (EGFR-NSCLC)? This question was investigated by a Greek research group. This was based on the results of the booster study, whose primary analysis did not demonstrate superiority of the osimertinib (osi)/bevacizumab (beva) combination over osi alone. However, an exploratory study showed an improvement in progression-free survival (PFS) in current or former smokers. Now, a systematic review and meta-analysis was performed to evaluate the relative effect of adding an angiogenesis inhibitor to EGFR TKI therapy in patients with advanced EGFR NSCLC according to their smoking status. All relevant randomized trials of osi/erlotinib (Erlo) with or without beva/ramucirumab (Ramu) published at major oncology meetings or in PubMed as of November 1, 2021 were reviewed. Hazard ratios (HRs) for the primary endpoint PFS by smoking status were used for analysis. Pooled HRs and interaction HRs were estimated with fixed-effect or random-effect models, depending on the degree of heterogeneity found. Seven randomized trials involving 1291 patients were included in the meta-analysis. Five of the studies included patients in first-line treatment (erlo/beva: 3; erlo/ramu and osi/beva: each 1) and two in second-line treatment (osi/beva). All studies had EGFR-TKI alone as the control group. In smokers (current or former, n=502), the pooled PFS HR estimate in favor of the combination was statistically significant (HR=0.55; 95% CI: 0.44-0.69; p<0.010), but not in nonsmokers (n=789) (HR=0.92; 95% CI: 0.66-1.27; p=0.60). The authors concluded that in advanced EGFR NSCLC patients who smoke, the addition of an angiogenesis inhibitor (beva, ramu) to EGFR TKI therapy (erlo, osi) provides a statistically significant PFS benefit. Whether this is due to a specific co-mutation pattern induced by tobacco exposure remains to be determined [1].
Detection of a rare clientele
RET fusions in non-small cell lung cancer (NSCLC) were addressed in a retrospective multicenter study. Nearly 1-2% of NSCLC patients have RET fusions. However, this rare population is not well characterized. Therefore, investigators evaluated clinical, pathologic, and biologic characteristics, as well as treatment outcomes (as assessed by investigators), including surgery, chemotherapy (CT), immunotherapy (ICI), CT-ICI, multityrosine kinase inhibitors (MTKi), and RET inhibitors (RETi) of NSCLC patients with RET at each stage. The molecular profile included DNA/RNA sequencing and/or FISH analyses. The median age of the 131 patients was 60 years, 57% were female, and 92% had adenocarcinoma. 44% smoked, 67% had metastases at diagnosis, 19% of which had brain metastases (BM). At the last follow-up, 30% of patients had BM. RET fusion partners were KIF5B (71%), CCDC6 (20%), others (19%). The mPD-L1 expression (n=101) was 5% (0-90), and the mTMB (n=18) was 3.50 mut/mB. The most common co-mutation was TP53 (21%). Overall survival was found to be higher in patients treated with RETi than without RETi. Progression-free survival (PFS) with RETi was 16.23 vs. 7.69 months in patients with and without TP53 mutations, respectively. In ICI-treated patients, mPD-L1 was numerically higher in responders than in non-responders (55% vs. 0%, p=0.059), and mPFS was 12.91, 7.94, and 2.18 months in patients with PR, SD, and PD, respectively, as the best objective response. The experts conclude that RETi treatment improves survival in pretreated patients and ICI may be effective, especially in patients with high PD-L1 [2].
The KRAS mutation type in view
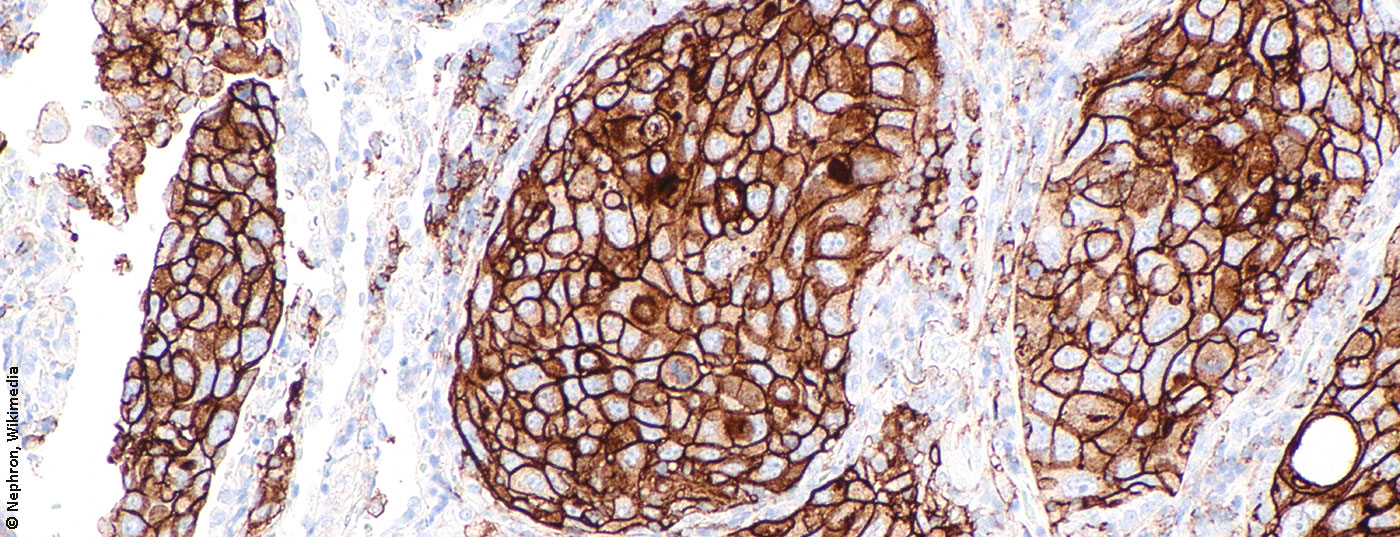
Approximately 20% of adenocarcinomas of the lung have KRAS mutations (mut). This is an oncogene that drives tumorigenesis and has the ability to alter the immunological microenvironment of the tumor. The most common mutation is KRAS G12C, accounting for approximately 40%, which has been associated with tobacco exposure. Despite the immunodependence of KRAS-related tumors, the efficacy of immunotherapy (IT) depending on KRAS mut type has not been adequately elucidated. Therefore, the aim of a study was to describe a cohort of patients with KRAS-mutated NSCLC and to evaluate the clinical outcomes of immunotherapy depending on the KRAS-mutated type. 120 predominantly male patients were included in the retrospective cohort. KRAS status was determined by the cobas® KRAS mut test, and PD-L1 status was determined by immunohistochemical assay. PD-L1 status in tumor cells was categorized as negative <1%, low 1-49%, and high 50-100%. 96% of those affected were current or former smokers. At diagnosis, 74% of patients had stage IV lung adenocarcinoma. KRAS status was determined in 107 patients: 46% carried KRAS G12C and 54% KRAS nonG12C. High PD-L1 concentration was detected in 37% of cases, predominantly in KRAS G12C versus non-G12C (56% versus 44%, p=0.2). A total of 65 patients (54%) were treated with IT for advanced disease-42% in the first line, 46% in the second line, and 12% in the third line. 81% received anti-PD-1, 16% anti-PD-L1, and 3% anti-CTLA-4. After a median follow-up of 63 months, median progression-free survival to IT was 10.1 months vs. 3.3 months in KRAS G12C vs. non-G12C (p=0.07); median overall survival was 17.9 months vs. 18.6 months in KRAS G12C vs. non-G12C (p=0.13). KRAS mutations represent a heterogeneous group of NSCLC. Although not statistically significant, patients with KRAS-G12C mut tended to have better mPFS after IT compared to patients without G12C mut – alleridngs without impact on OS [3].
Biomarker testing requires efficient strategy
In Spain, the situation of biomarker testing has been scrutinized more closely. This was based on the Thoracic Tumor Registry (TTR), a prospective, registry-based observational study that enrolled patients with lung cancer and other thoracic tumors from September 2016 to the present. 9239 patients with stage IV non-small cell lung cancer (NSCLC) were analyzed. 7467 (80.8%) were non-squamous and 1772 (19.2%) were squamous carcinoma. Tumor markers were tested in 85.0% of patients with non-squamous tumors versus 56.3% of patients with squamous tumors (p<0.001). Global testing of EGFR, ALK, and ROS1 was 78.9%, 64.7%, and 35.6%, respectively, in non-squamous histology. However, in recent years, there has been a significant increase in all determinations, and there are even nearly 10% of molecular determinations that have not yet received targeted drug approval, but will in the near future. 4115 cases had a positive result (44.5%) for either EGFR, ALK, KRAS, BRAF, ROS1, or PDL1. The situation in Spain is similar to that in other European countries. Given the growing number of different determinations and their high positivity, national strategies are urgently needed to implement next-generation NGS sequencing in lung cancer in an integrated and cost-effective manner [4].
Congress: European Lung Cancer Congress
Literature:
- Dafni U, Soo RA, Peters S, et al: Impact of smoking status on the relative efficacy of the EGFR TKI/angiogenesis inhibitor combination therapy in advanced NSCLC: A systematic review and meta-analysis. ID 5131.
- Marinello A, Duruisseaux M, Zrafi WA, et al: RET-MAP: An international multi-center study on clinicopathologic features and treatment response in patients with NSCLC and RET fusions. ID 5133.
- Rincon LN, Pous A, Lopez-Paradis A, et al: The immunotherapy role in patients (pt) with KRAS mutated metastatic non-small cell lung cancer (NSCLC): Differences between KRAS G12C and non-G12C. ID 5137.
- Calvo de Juan V, Cobo Dols M, Rodriguez-Abreu D, et al: Determination of essential biomarkers in lung cancer: A real-world data study in Spain. ID 5138.
InFo ONCOLOGY & HEMATOLOGY 2022; 10(2): 28-29.