The earlier colorectal cancer is detected, the greater the chances of cure. Therefore, early detection examinations are very important, especially in the elderly population. Colonoscopy is recommended as a routine examination in patients over 50 years of age. This allows benign polyps to be detected and removed before a malignant tumor develops. With regard to medications for bowel cleansing, a newer preparation has been shown in studies to be equivalent to conventional products.
Colorectal cancer is one of the most common tumor diseases, with symptoms often developing insidiously. Cancers of the colon, rectum and rectum are grouped under the term “colorectal carcinoma” and manifest oligosymptomatically. The most common signs of an intestinal tumor include altered bowel habits and blood in the stool. Early diagnosis and treatment is crucial for the chances of cure [1]. It is estimated that it takes around ten years for a benign polyp in the intestine to turn into a malignant tumor. Ideally, colorectal cancer should be detected before symptoms occur.
Colonoscopy recommended as a routine check from the age of 50
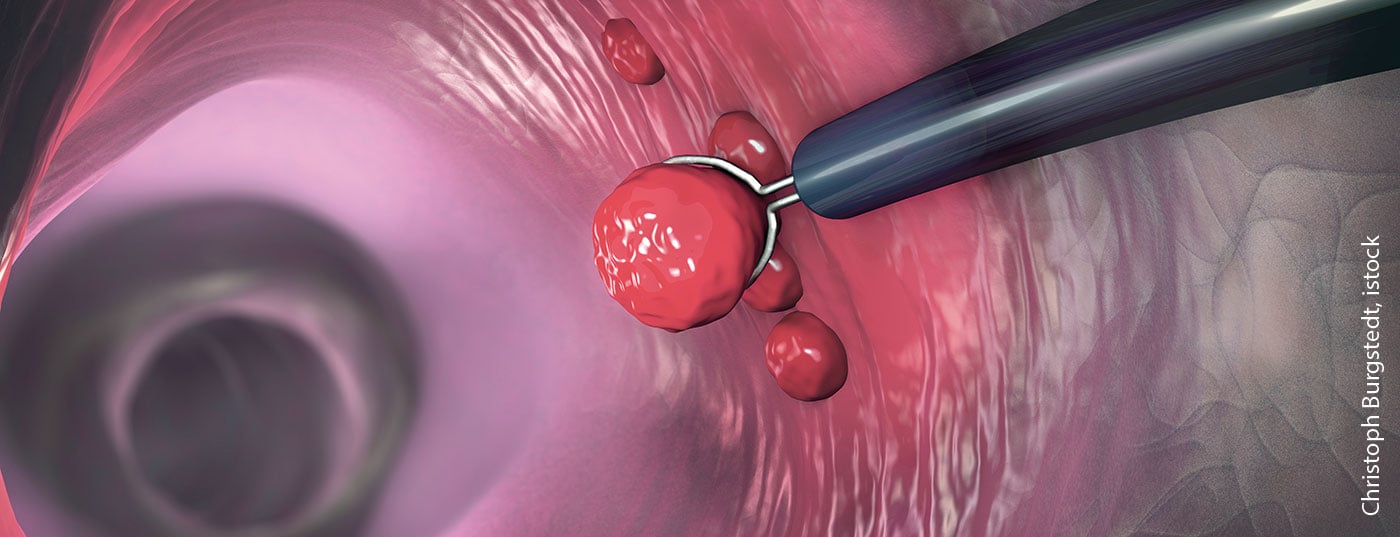
Colonoscopy can detect intestinal polyps and tumors with a high degree of certainty. Along with the blood-in-stool test (FIT), it is the most important examination method for the early detection of colorectal cancer [2]. In Switzerland, basic health insurance covers the costs of colorectal cancer screening examinations for individuals aged 50 to 69 years. A colonoscopy is paid for every ten years, and a blood-in-stool test every two years. By removing polyps directly during colonoscopy, it is possible to prevent them from becoming cancerous. In most cases, colonoscopy is a low-pain examination with a low risk of complications. In rare cases, polyp removal may result in injury to the bowel or bleeding. To ensure that the inside of the bowel can be assessed well, bowel evacuation is necessary before the examination. For this purpose, a strong laxative must be taken the day before and on the day of the examination itself, followed by drinking plenty of fluids.
Newer preparation for bowel cleansing is similarly effective to conventional products
The drug Clensia® is composed of known active ingredients and is available in powder form for the preparation of an oral solution. By combining several salts, a great deal of water is drawn into the intestines in a short time, resulting in thorough evacuation and bowel emptying. Clensia® has been approved in Switzerland since October 2019 for the indication of bowel evacuation prior to intestinal interventions, such as endoscopic or radiological examinations, and has been included in the Specialty List (SL) of health insurance since March 1, 2020 [3]. In several clinical studies, Clensia® was found to be non-inferior to polyethylene glycol (PEG)-4 L and Moviprep® in terms of colonic cleansing (Ottawa scale) [3]. This is demonstrated by the results of the following two randomized-controlled phase III studies [4–6]:
Spada et al. 2017 [5] were able to demonstrate the non-inferiority of Clensia® compared to PEG 4 L, consisting of macrogol plus electrolytes. 422 patients between 18 and 85 years of age scheduled for colonoscopy were randomized 1:1 to Clensia® or PEG 4 L conditions. The proportion of patients with excellent or good colonic clearance assessed by the Ottawa scale was 68.1% under Clensia® and 69.2% under PEG 4 L. The mean difference was 1.2% (95% CI: -10.0; 7.7). With a confidence interval in the range of -15% to 15%, statistical evidence of equivalence of treatments is considered to be met. Regarding the following secondary endpoints, Clensia® performed significantly better compared to PEG 4 L: no discomfort while taking the preparation (72.8% vs. 63%), willingness to use the same preparation again for future colonoscopies (93.9% vs. 82.2). Clensia® also proved superior in terms of optimal mucosal visibility with 63% compared to 55% in the PEG 4 L condition, although the significance level was not reached.
Kump et al. 2018 [6] were able to demonstrate the non-inferiority of Clensia® compared to Moviprep®. The 389 study participants aged 18 to 85 years scheduled for routine colonoscopy were randomized 1:1 to receive Clensia® or Moviprep®. Excellent or good colonic clearance according to the Ottawa scale was achieved by 78.8% in the Clensia® group compared to 74.5% in the Moviprep® condition. The mean difference was 4.3% (95% CI: -4.2; 12.7), providing evidence of equivalence of treatments (confidence interval ranged from -15% to 15%). Clensia® proved superior to Moviprep® with respect to the secondary endpoint of optimal mucosal visibility (53.9% vs. 50.5%). Almost equal were the results regarding optimal compliance (93.4% vs. 94.8%) and willingness to use the same preparation again for future colonoscopies (90.2% vs. 90.7%).
Clensia®, which is one of the osmotically acting laxatives, is approved for adults 18 years of age and older. The side effect rates were comparable to those of the two comparator products PEG 4 L and Moviprep®. No clinically relevant changes in serum electrolytes, body weight, and vital signs were observed [4]. Dosage recommendations vshould be followed carefully to maximize efficacy and safety.
Literature:
- Colon cancer (colonic carcinoma): Early detection, symptoms, therapy, www.apotheken-umschau.de/Dickdarmkrebs
- Swiss Cancer League, www.krebsliga.ch/krebs-vorbeugen/praevention-und-frueherkennung/frueherkennung/darmkrebs/praevention-und-frueherkennung-von-darmkrebs
- Subject information, www.swissmedicinfo.ch
- Federal Office of Public Health FOPH: Directorate Health and Accident Insurance: (20958) CLENSIA, Alfasigma Schweiz AG: New inclusion in the list of specialties (SL) as of March 1, 2020.
- Spada C, et al: Evaluation of Clensia®, a new low-volume PEG bowel preparation in colonoscopy: Multicentre randomized controlled trial versus 4L PEG. Digestive and Liver Disease 2017; 49.6: 651-656.
- Kump P, et al: Efficacy and safety of a new low-volume PEG with citrate and simethicone bowel preparation for colonoscopy (Clensia): a multicenter randomized observer-blind clinical trial vs. a low-volume PEG with ascorbic acid (PEG-ASC). Endoscopy international open 2018; 6.08: E907-E913.
HAUSARZT PRAXIS 2021; 16(2): 26