Consistent basic therapy helps restore impaired barrier function and relieves xeroderma and itching. It is indicated at all stages regardless of the severity of atopic dermatitis. In long-term management, this allows for a prolonged relapse-free interval and recent studies show a protective effect of basic therapy in neonates at risk of atopy.
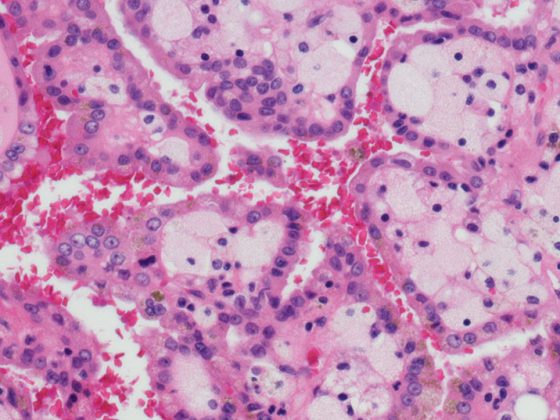
A defect in the barrier function of the skin is a characteristic of atopic dermatitis and is further exacerbated by a cutaneous inflammatory response [1,2]. Restoration of impaired barrier function is central in the therapeutic management of atopic dermatitis. Therefore, basic therapy in all stages and severities of atopic dermatitis is included in national and international guidelines [3,4]. An important component of this is emollients – externals, which are traditionally free of active ingredients and have refatting properties.
| Emollients containing urea have been shown to significantly improve pruritus and long-term control [15], but even low concentrations can cause burning of the skin (stining effect), particularly in children up to the age of five. Therefore, urea is not recommended in infants and young children [7]. Glycerin-containing basic care products without urea are a well-tolerated alternative in these cases [16]. Glycerin is a moisturizing active ingredient and a component of rehydrating moisturizers for basic care. |
Why regeneration of the barrier function is so important
Empirical findings show that the skin of neurodermatitis patients has, among other things, a characteristically altered composition of epidermal lipids [4]. In addition, altered expression of filaggrin due to genetic mutation, exogenous influences, or inflammation-related cytokines has been observed in atopic patients [4–6]. These factors contribute to impaired epidermal barrier function, which in turn increases the risk of irritant, allergenic, or nonspecific trigger factors. Filaggrin is cleaved in the stratum corneum to amino acids, which act as natural moisturizing factors (NMF) to hydrate the cornea and reduce transepidermal water loss (TEWL) through their water-retentive effect. An elevated TEWL characteristic of atopic dermatitis is associated with a disrupted skin barrier. Parched skin is a common problem in atopic dermatitis and can promote inflammation and lead to itching and burning.
Protective function in newborns at risk of atopy
The regulation of TEWL is an important function of the skin, especially in neonates and infants, which is disturbed at increased risk of atopy [7]. A non-invasive method for determining TEWL is the use of a Tewameter® TM 300 [8]. Emollient creams counteract TEWL and strengthen the skin barrier in the long term. It is considered scientifically proven that reduced epidermal barrier function at birth and two months of age is a predictor of clinically manifest atopic dermatitis at 1 year of age and this can be favorably influenced by consistent basic therapy [9]. A randomized controlled trial in the US and UK (n=124) demonstrated that daily emollient therapy from birth had a protective effect, resulting in a relative risk reduction of 50% in the cumulative incidence of atopic dermatitis six months after baseline (RR 0.50; 95% CI, 0.28-0.9; p=0.017). [10]. Study participants were neonates 0-3 weeks of age at high risk for atopic dermatitis, meaning that at least one parent or sibling was affected by diagnosed atopic dermatitis, asthma, or allergic rhinitis [10]. Atopy in first-degree relatives is considered to be a significant risk factor [11,12]. In the treatment arm, infants were treated with emollients at least once daily; in the control condition, no emollients were used at all. The results of this study are consistent with reports of previous research that the use of emollients in neonates is a protective factor with respect to the development of inflammatory skin lesions [13,14]. The conclusion is that emollient therapy in infants at increased risk of atopy is a safe and effective way to promote skin barrier function through exogenous lipids and prevent inflammatory skin lesions.
Literature:
- Volz T, et al: On the role of the innate immune system in atopic dermatitis. Dermatologist 2015; 66: 90-95.
- Biedermann T, et al: Regulation of T Cell Immunity in Atopic Dermatitis by Microbes: The Yin and Yang of Cutaneous Inflammation. Front Immunol 2015; 6: 353.
- Eichenfield LF, et al: Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol 2014; 71: 116-132.
- Werfel T, et al: S2k guideline neurodermatitis (atopic eczema, atopic dermatitis) – abridged version. J Dtsch Dermatol Ges 2016; 14: 92-106.
- Irvine AD, McLean WHI, Leung DYM: Mechanisms of disease. Filaggrin Mutations Associated with Skin and Allergic Diseases. N Engl J Med 2011; 365: 1315-1327.
- Vickery BP: Skin barrier function in atopic dermatitis. Current Opinion in Pediatrics. 2007; 19 (37): 89-93.
- Deutsche Apotheker Zeitung: www.deutsche-apotheker-zeitung.de/daz-az/2018/daz-38-2018/hochempfindlich
- Tewameter® TM 300, https://courage-khazaka.de/de
- Kelleher M, et al: Skin barrier dysfunction measured by transepidermal water loss at 2 days and 2 months predicts and predicts atopic dermatitis at 1 year. J Allergy Clin Immunol 2015; 135(4): 930-935.e1.
- Simpson EL, et al. Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol 2014; 134(4): 818-823.
- Apfelbacher CJ, et al: Determinants of eczema: population-based cross-sectional study in Germany. Allergy 2011; 66: 206-213
- Eichenfield LF, et al: Guidelines of care for the management of atopic dermatitis: Section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014; 70: 338-351.
- Odhiambo JA, et al. (ISAAC Phase Three Study Group): Global variations in prevalence of eczema symptoms in children from ISAAC phase three. J Allergy Clin Immunol. 2009; 124: 1251-1258.e23
- Simpson EL, et al: A pilot study of emollient therapy for the primary prevention of atopic dermatitis. J Am Acad Dermatol 2010; 63: 587-593.
- Lindh JD, Bradley M: Clinical Effectiveness of Moisturizers in Atopic Dermatitis and Related Disorders: A Systematic Review. Am J Clin Dermatol 2015; 16 (5): 341-359.
- Wolf G, Höger PH: Basic dermatological therapy with hypoallergenic and noxigen-free topical preparations in children. JDDG J Dtsch Dermatol Ges 2009; 7 (1): 50-61.
DERMATOLOGY PRACTICE 2020; 30(2): 20