The acronym ILD for Interstitial Lung Disease is widely known to pulmonologists. Much less familiar, on the other hand, are ILAs – Interstitial Lung Abnormalities. The term is applied when unusual changes are found on CT in individuals who do not have a clinical diagnosis of ILD at that time.
With age, there is an increased incidence of lung changes such as striated and reticular consolidations, centrilobular nodules, cysts, and discrete bronchiectasis. Are these incisional changes, termed ILA, without significance computed tomographically? Or should ILA be considered a very mild or early form of lung disease requiring therapy?
Although there is no clear definition, it is clear that ILA must involve more than 5% of the area of a lung segment of:
- Frosted glass,
- reticulated pattern,
- centrinular nodes,
- Cysts (no emphysema),
- Honeycomb pattern or
- Traction bronchiectasis
“These are the six morphologic patterns that provide the vast majority of these chronic abnormalities,” said radiologist Professor Gerhard Mostbeck, MD, of Vienna, Austria, at Pneumo Update 2019 in Mainz, Germany. “Even in recent years, serial CT studies have shown that progression of such an abnormality to full-blown disease is not that rare.” In this context, according to the expert, ILA has also been shown to be associated with rapid deterioration of LuFu and increased mortality.
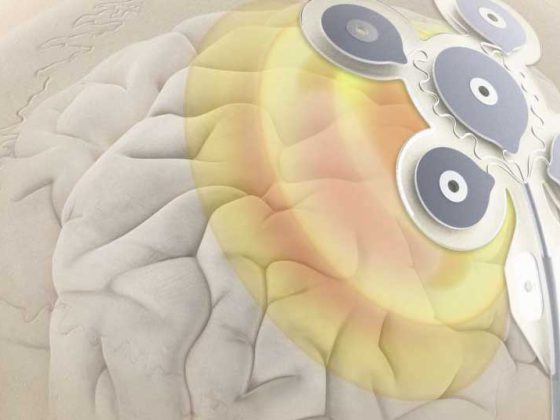
A recent study [1] examined the “patterns” of these ILA changes associated with progression to ILD and increased mortality. For this purpose, the authors used 5320 participants from the AGES-Reykjavik study, of whom 3167 were examined with CT and control CT at a mean interval of 5.1 years. Three independent radiologists and pulmonologists first defined the presence or absence of ILA (defined as change in more than 5% of a lung zone) in prevalence CT.
The result was revealing: 327 participants (10%) had ILA in at least one of the CT examinations. Of these, 73 individuals have shown progression in progression. Older age and a genetic mutation (MUC5b genotype) were statistically significantly associated with progression. Fibrotic changes had the highest probability of progression, but also increased mortality. The authors conclude that specific patterns of interstitial lung abnormalities can be used to prognostically estimate progression to ILD and increased mortality.
In addition to the increase in prevalence with age and higher mortality, a correlation with pulmonary fibrosis is particularly apparent. In particular, fibrotic patterns such as traction bronchiectasis and areas of honeycomb lung often progress to pulmonary fibrosis. Therefore, according to Prof. Mostbeck, “discrete changes”, if they are “fibrotic”, can also be communicated in asymptomatic individuals of an older age group. The possibility of progression should be noted, and the need for follow-up CT scans and pulmonary evaluation is evident.
“We should be familiar with the term ILA,” the radiologist concluded, “and also be aware of its possible significance regarding progression to ILD in fibrotic patterns.” He recommended refraining from ambiguously labeling small or insignificant changes as “hypostases,” “postinflammatory residuals,” or “positional compressions,” “as has been the fond custom in radiology.” The challenge for the pulmonologist, he said, is to recognize fibrotic lung changes in particular as an abnormality, describe them, and find a further workup and follow-up.
Source: Lecture “Thoracic Imaging” at the 16th Pneumology Update Seminar in Mainz (D), Nov. 15, 2019.
Literature:
- Putman RK, Gudmundsson G, Axelsson GT, et al: Imaging patterns are associated with interstitial lung abnormality progression and mortality. American journal of respiratory and critical care medicine 2019; https://doi.org/10.1164/rccm.201809-1652OC
InFo PNEUMOLOGY & ALLERGOLOGY 2019; 1(3): 25