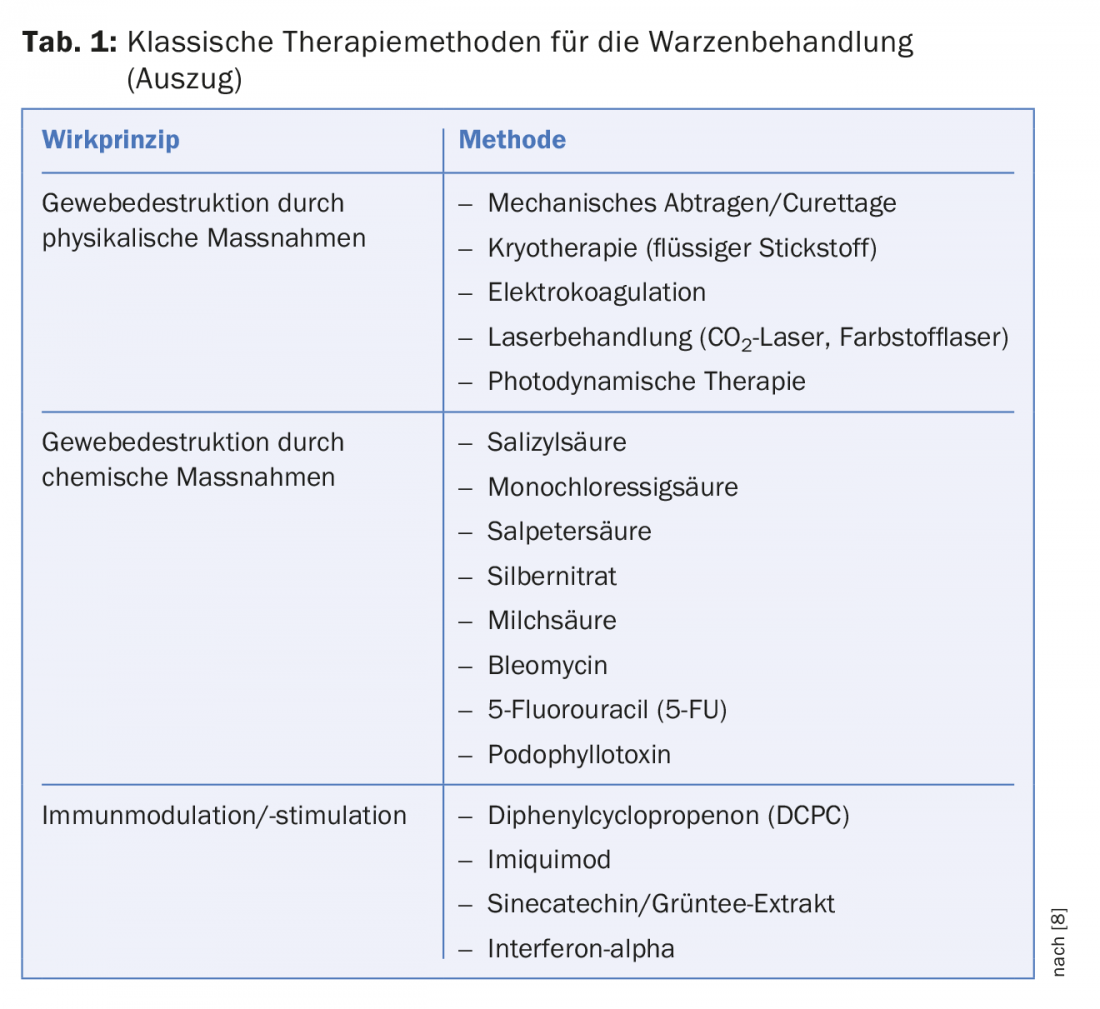
Skin lesions caused by HPV viruses are usually benign lesions that manifest cutaneously or mucocutaneously. The risk of infection is high. Mechanisms of action include tissue destruction by physical or chemical means and immune modulation/stimulation. Laser treatments are also a treatment option. Vaccinations against HPV viruses have a prophylactic effect.
Almost all people suffer from warts at some point in their lives. They are mostly hemispherical skin lesions on skin and mucous membranes that show a fissured surface. It is based on a viral infection with HPV viruses (human papilloma virus) or with certain poxviruses (molluscum contagiosum virus). Furthermore, the term wart is also used for non-infectious changes, namely for the seborrheic warts or age warts that frequently occur in old age.
The HPV virus
Most commonly, viral warts are caused by human papillomavirus (HPV) infection. It is a group of DNA viruses that only affect humans. Through the smallest injuries to skin or mucous membrane, the virus enters the epithelial cells, where it multiplies rapidly. Infection leads to reactive, tumor-like epithelial hyperplasia with widening of the epidermis (acanthosis) and papillomatosis (finger-like extended papillae). On the skin, there is also often marked hyperkeratosis with small blood inclusions.
To date, more than 100 HPV types are known. Most HPV-induced skin lesions are benign lesions. However, some HPV types can lead to malignant transformation with subsequent carcinoma development (e.g., cervical carcinoma in women).
Direct skin contact leads to infection with HPV viruses. Indirect transmission in swimming pools or gymnasiums is also possible. A prerequisite for virus transmission is a damaged epithelial skin barrier. The feet, fingers or the backs of the hands are most frequently infected (Fig. 1) . Through direct contact (smear infection), the viruses can also reach other parts of the body.

Clinical manifestations of warts
The main distinction is between cutaneous, non-genital warts and mucocutaneous warts, which affect the mucous membranes.
Cutaneous warts
Cutaneous warts are the most common type. Children and young people are particularly affected. It is estimated that up to 33% of primary school students suffer from such cutaneous warts, while the prevalence in adults is much lower, with an infestation of approximately 3.5% [1]. Immunosuppression is a particular risk factor. In renal transplant recipients, warts are found in 90% of individuals after more than five years of immunosuppressive therapy [2]. The most common is the vulgar wart (Verruca vulgaris) (Fig. 2).

Especially fingers, toes and back of the hand are affected. Clinically, there is a hemispherical skin change with a fissured surface. A special form are the periungual warts, which often appear grouped around the nail fold. Spreading under the nail plate can be painful and also complicate treatment. Nail biting is a risk factor for the development of periungual warts.
Another clinical feature is filiform warts, which are pedunculated and often occur on eyelids or in the beard area. Especially when shaving, autoinoculation can cause the latter to spread. Plantar warts (verrucae plantares) are a special form of vulgar warts on the soles of the feet. Due to the mechanical stress on the sole of the foot, such warts grow inward rather than outward papillomatous, resulting in the so-called plantar wart (Fig. 1). Depending on their location, such warts can be very painful when walking. If they are not treated, they can spread over a wide area. Regular beds of warts form (Fig. 3) . Plane warts occur mainly in children and adolescents. The hands, forearms or face are often affected. Flat, skin-colored papules with a rough surface are found. It is not uncommon for seeding to occur here as well.

Mucocutaneous warts
Certain HPV types preferentially infect the mucous membranes. The classic form of genital warts are genital warts or condylomata acuminata. These are mainly caused by HPV types 6 and 11. In most cases, these warts are harmless, showing a spontaneous remission rate of up to 30% [3]. The oral region, anal or genital region may be affected. Transmission usually occurs through sexual contact. Clinically, pink to whitish papules or plaques are found, which can lead to cauliflower-like growths. In men, genital warts are most commonly found on the shaft of the penis. Furthermore, the perianal region, the glans penis, the prepuce or the urethra may be affected. In women, the vulvar region is most frequently affected. Furthermore, condylomata acuminata are found in the vaginal, perineal and perianal regions. Rarely, the cervix and urethra are affected. Recurrences are often observed after treatment of genital warts.
Dell warts
Dell warts, also known as Mollusca contagiosa, are nodular skin lesions caused by a viral infection. Transmission occurs through direct skin contact from person to person (contact infection). The risk of infection, for example within the family or within the daycare center/school, is high. The course is generally self-limiting, i.e. complete regression occurs within months. Children between the ages of two and six are most commonly affected. Especially children with atopic eczema tend to have a pronounced infestation. The dry skin and itching with subsequent scratching often cause the warts to spread (Fig. 4). Furthermore, molluscs are also found in sexually active adults and immunosuppressed individuals.

Diagnostics
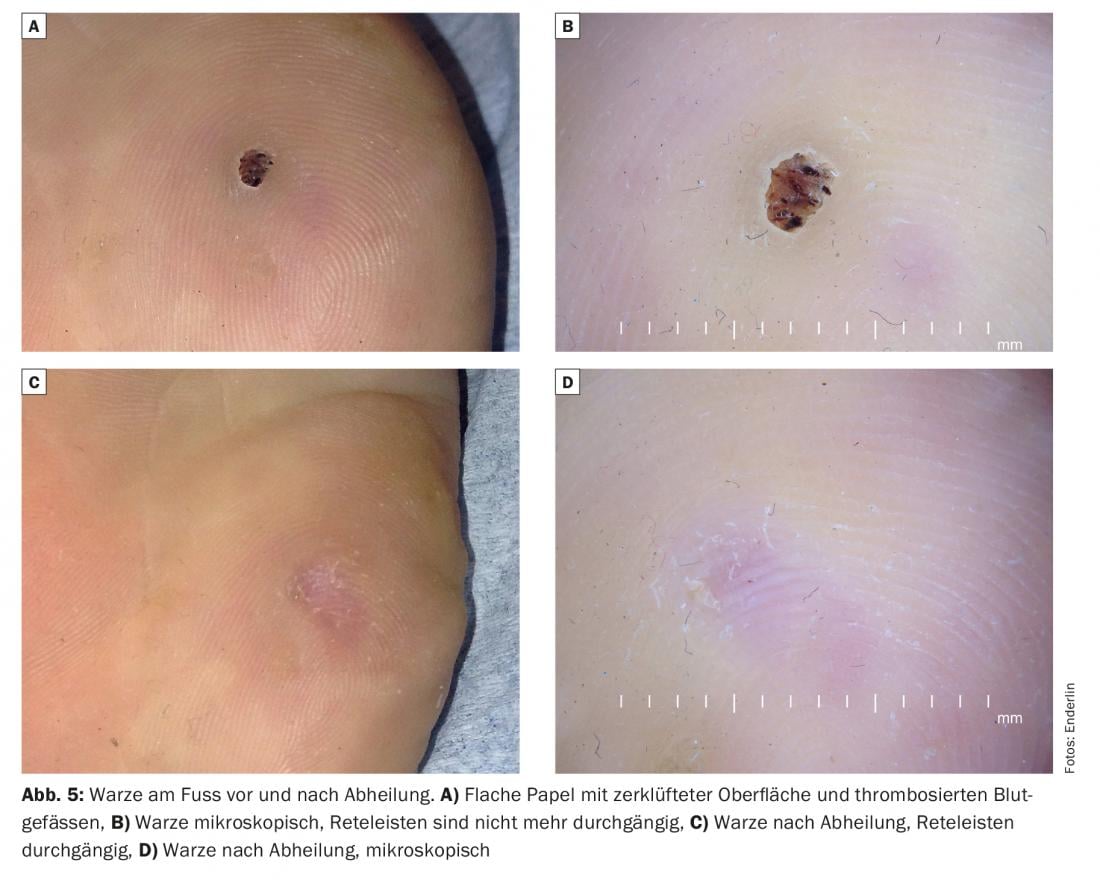
The diagnosis of warts is usually made clinically. In vulgar warts, a glance with the dermoscope is sufficient to detect the typical thrombosed blood vessels, which are perceptible as black dots (Fig. 5) . Typically, in warts on the hands and feet, the rete ridges are no longer continuous. Biopsy is useful in cases of differential diagnostic problems, particularly pronounced involvement, or lack of response to therapy. HPV typing should be considered only in individual cases.
The treatment of warts
There is no one hundred percent effective therapy against warts. This is probably why there is a wide range of treatment methods – from classical-traditional therapy to home remedies and preparations from alternative medicine. Due to their often self-limiting course, treatment of warts is not always necessary. However, if warts multiply, become larger and cause pain or are cosmetically disturbing, therapy is advisable.
Mechanical removal of the warts is useful as a basic therapy. This removes the top layer so that the subsequent treatments can work better. Only by removing the cornea can the applied active ingredient reach the active part of the wart. Last but not least, removing the thorn in plantar warts can reduce pain. A scalpel blade or a curette is suitable for this purpose (Fig. 6). However, removal should only be carried out after instruction by a specialist, as otherwise the risk of injury is too great.

Painful scarring often occurs after surgical removal. Furthermore, chemical substances, such as acids or cytostatics, also come into play. Acids lead directly to tissue destruction via a corrosive effect. In the case of strong acids, care must be taken to ensure that the surrounding healthy tissue is not also destroyed. This can be protected with petroleum jelly, for example. The salicylic acid leads mainly to the dissolution of the horny layer (keratolysis). In particular, patches containing salicylic acid are well suited for chemical keratolysis (horn dissolution). These are cut to size and glued and fixed directly to the wart. After 12 to 24 hours, the tissue is softened and can be easily removed. Other acids, which are contained in wart remedies, are lactic acid, monochloroacetic acid or nitric acid and others.
The application of liquid nitrogen (cryotherapy) by spraying also leads to tissue destruction (Fig. 7). Depending on the intensity of treatment, this method is painful. Sensitivity to touch may be present one to two days after treatment. The wart treated in this way is much easier to remove after cryotherapy. This method can be used for both skin and mucosal warts. Over-the-counter cold sprays for self-treatment can be tried. However, the temperatures achieved are lower than those obtained in the open spray process with liquid nitrogen.
Other treatment methods try to make the wart disappear by stimulating the body’s own defenses. This includes forms of psychological influence.

Laser treatment with theCO2 laser is another treatment option for both cutaneous and genital warts. This results in coagulation of the tissue or tissue vaporization. Two to three treatments are often required, but the healing rate is high; certain studies report healing rates of up to 100% [4,5]. When treating vulgar warts withCO2 laser, the healing time is prolonged compared to other treatment methods and ranges from two to six weeks [6]. According to our experience, this method is only suitable for warts that are extremely resistant to therapy.
To date, there is no single treatment method that is one hundred percent effective. Experience shows that wart treatments need to be customized. A combination of different treatment methods (for example, mechanical removal of the wart, application of salicylic acid and cryotherapy) is also promising. Furthermore, the age of the patient plays a role. In children, one is more likely to choose a procedure that is as painless as possible and easy to perform at home. Certain treatments are contraindicated in pregnant women.
In general, warts that have been present for less than a year are easier to treat than those that have been in the same place for more than a year. Treatment is reasonable in the following cases: pain, risk of spread, malignant transformation risk, significant cosmetic impairment, urgent patient request.
Complications after wart therapy may include: Blistering (partly desired side effect), inflammation, pain, scar.
Evidence-based treatment methods
While many treatments are medically established, controlled trials are rare and for many treatments the evidence base is uncertain. In 2012, a Cochrane review on the treatment of cutaneous warts was published that included 85 studies (with nearly 9000 patients). Locally applied salicylic acid shows the best evidence of therapeutic success. In five randomized controlled trials, 73% of patients experienced healing at six to 12 weeks compared to 48% healing with placebo [5]. Compared with this form of therapy, cryotherapy is equivalent. The application of liquid nitrogen (by contact or spray method) freezes the wart for a short time. This leads to direct damage to the skin with subsequent necrosis. Furthermore, an inflammatory reaction occurs. The treatment is somewhat painful, sometimes blistering may occur. The treatment interval is usually three to four weeks. Intralesional bleomycin shows inconsistent evidence-from rapid therapeutic success to complete lack of effect [7,8]. It is a glycopeptide antibiotic (from Streptomyces verticillus) that inhibits cell division, cell growth, and DNA synthesis. Here, the diluted bleomycin solution is injected directly into the wart using a fine syringe or a special application device (Dermojet®) (Fig. 8) . Intralesional bleomycin is a therapeutic option especially for refractory plantar warts. Within a few days after application, necrosis occurs. This can sometimes be painful when walking. The resulting scab is usually removed after 10-14 days.

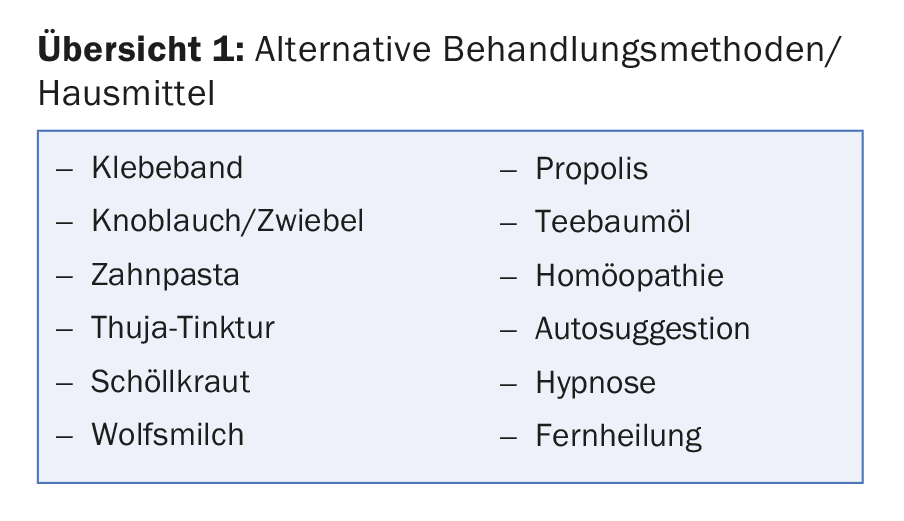
Alternative treatment methods
Home remedies are numerous. Warts are often taped off, rubbed with half a clove of garlic or an onion, or various means such as toothpaste, thuja tincture, tea tree oil, celandine or propolis are applied. It is worth mentioning that these home remedies probably show therapeutic success in some patients, but there are no controlled studies on them. Often the belief that the wart will disappear with this remedy is enough. Which then comes very close to the process of suggestion. Especially in children, the belief in the healing power of a therapy is often enough to achieve a cure for the wart.
The treatment of anogenital warts
Anogenital warts may also disappear spontaneously after one to two years. However, it is not possible to predict whether an anogenital wart will regress, persist, or increase in size [9]. Therefore, to prevent spread and transmission, anogenital warts should be treated. The standard treatment of genital warts is cryotherapy, laser therapy (CO2 laser) and curettage/excision. These lead to tissue destruction. Cryotherapy of genital warts shows healing rates of 50% with two treatment cycles [10]. Furthermore, various local therapeutic agents can be used (podophyllotoxin, imiquimod [Aldara®] or an ointment made from green tea extract [Veregen®]). Treatment of anogenital warts with imiquimod for 16 weeks showed healing of 50% (versus 16% on placebo) in men, and 72% (versus 20% on placebo) in women [11]. However, recurrence also occurs; Diamantis et al. Report 19% relapse after three months [12].
Dell warts therapy
Due to the self-limiting course, few dell warts do not require treatment. If necessary, local therapy with ten percent potassium hydroxide solution can be applied. The solution is applied directly to the warts once a day for an average of one week. As soon as redness or first signs of inflammation are visible, the treatment is discontinued. Healing usually occurs within two to three weeks. In case of extensive mollusc infestation, curettage under local anesthesia (lidocaine gel) is useful. Prophylactically, good refatting measures help.
HPV vaccination
Since 2006, several vaccines have been developed that provide protection against papillomaviruses with high oncogenic risk. Most common in Switzerland is vaccination with the quadrivalent vaccine (against HPV 6, 11, 16 and 18) or nonavalent vaccine (against HPV types 6, 11, 16, 18, 31, 33, 45, 52 and 58). High-risk types 16 and 18, in particular, are blamed for more than two-thirds of all cervical cancers [13]. Since the introduction of these vaccines, a decrease in new cases (condylomata acuminata, cervical dysplasia) has been observed.
Take-Home Messages
- Most HPV-induced skin lesions are benign lesions. However, some HPV types can lead to malignant transformation with carcinoma development.
- Dell warts (Mollusca contagiosa) are caused by a viral infection. The risk of infection is high. However, the course is generally self-limiting.
- Mechanisms of action include tissue destruction by physical measures or by chemical measures, and immune modulation/stimulation.
- Laser treatment with theCO2 laser is another treatment option for both cutaneous and genital warts.
- Since the introduction of various vaccines against HPV viruses, a decrease in new cases (condylomata acuminata, cervical dysplasia) has been observed.
Literature:
- Cardoso J, Calonje E: Cutaneous manifestations of human papillomaviruses: a review. Acta Dermatovenerol Alp Panonica Adriat 2011; 20: 145-154.
- Leigh I, Glover M: Skin cancer and warts in immunosuppressed renal transplant recipients. Recent Results Cancer Res 1995; 139: 69-86.
- Wiley D, Masongsong E: Human papillomavirus: the burden of infection. Obstet Gynecol Surv 2006; 61(6 Supp. 1): S3-14.
- Mc Burney E, Rosen D: Carbon dioxide laser treatment of verrucae vulgaris. J Dermatol Surg Oncol 1984; 10: 45-48.
- Mueller T, Carlson B, Lindy M: The use of carbon dioxide surgical laser for the treatment of verrucae. J Am Podiatr Med Assoc 1981; 70: 136-144.
- Combemale P, Delolme H, Dupin M: Traitement de verrues. Ann Dermatol Venereol 1998; 125: 443-462.
- Kwok CS, et al: Topical treatments for cutaneous warts. Cochrane Database Syst Rev 2012; Sep 12; 9: CD001781. doi: 10.1002/14651858.CD001781.pub3.
- Streit M: Warts – clinical pictures and therapy. Switzerland Med Forum 2014; 14(35): 634-639.
- Berman B, Wolf J: The role of imiquimod 3.75% cream in the treatment of external genital warts. Skin Therapy Letters 2012; 17: 5-7.
- Mi X, et al: A randomized clinical comparative study of cryotherapy plus photodynamic therapy vs. cryotherapy in the treatment of multiple condylomata acuminata. Photodermatol Photoimmunol Photomed 2011; 27: 176-180.
- Edwards L, et al: Self-administered topical 5% imiquimod cream for external anogenital warts. Arch Dermatol 1998; 134: 25-30.
- Diamantis ML, Bartlett BL, Tyring SK: Safety, efficacy & recurrence rates of imiquimod cream 5% for treatment of anogenital warts. Skin Therapy Letters 2009; 14: 1-3, 5.
- Gillison ML, Chaturvedi AK, Lowy DR: HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer 2008; 113(10 Suppl): 3036-3046.
DERMATOLOGIE PRAXIS 2018; 28(3): 27-32