Stimulative growth disturbances occur after any meta-diaphyseal fracture in childhood. They usually result in increased length growth and can last up to two years. Inhibitory growth disorders are more common in the lower extremities.
Most fractures in children are not dissimilar to adult fractures, although fractures on the growing skeleton have some unique features. Infantile bone is softer and breaks more easily than adult cortical bone. Accordingly, fracture also occurs more rapidly in low energy accidents. The periosteum is much thicker and stronger in the child and usually still holds the fractured bone ends together or facilitates reduction. In addition, due to the softer and more elastic bone, plastic deformity, greenwood fracture, and bulge fracture occur as additional features in childhood.
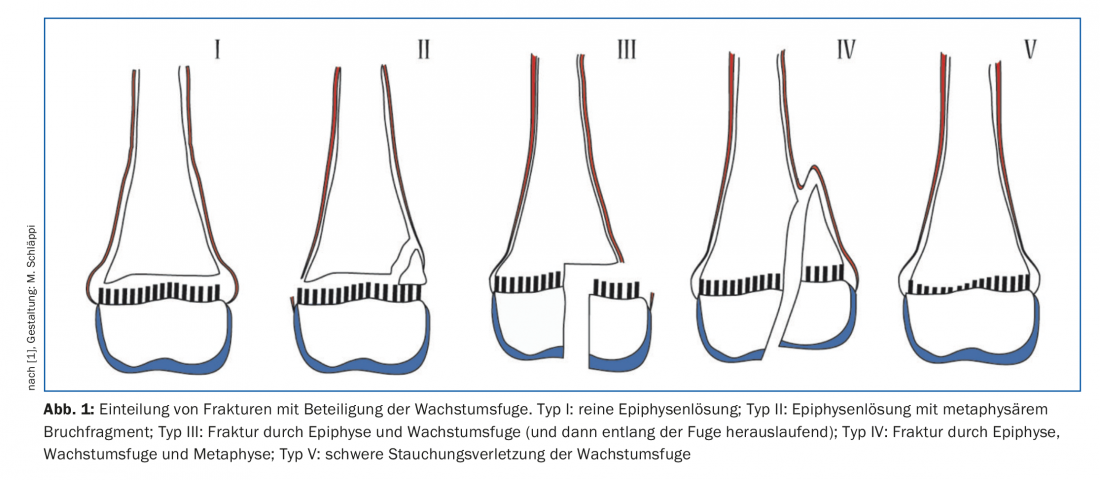
However, the greatest peculiarity of the infantile bone is undoubtedly the presence of cartilaginous growth plates. These are responsible for the longitudinal growth of the bone, while the periosteum is responsible for the appositional growth in width. The growth zones divide the long tubular bones into the respective epiphyses and the centrally connected bone part of the two metaphyses and the diaphysis. Since the growth plate is a site of reduced mechanical stability, a kind of predetermined breaking point, the connection between the epiphysis and metaphysis is additionally strengthened by the perichondral ring surrounding the plate. The growth plate protects the epiphyseal articular block in that metaphyseal fractures rarely have a spur into the joint, but extend laterally along the growth plate. Fracture forms in the region of the growth plates are classified according to Salter-Harris (Fig. 1) [1]. In accordance with what was previously said, type I and II fractures are significantly more common compared to types III and IV, in which the epiphysis is fractured along with the attached growth plate. The type V fracture is a special form in which a compression injury of the growth zone is retrospectively assumed in the course on the basis of an occurring growth disturbance.
After growth-age fractures, spontaneous correction may occur if consolidation occurs in malposition during growth. Depending on the fracture localization and the type of malposition as well as the residual growth still to be expected, malpositions can be tolerated to varying degrees accordingly [2,3]. However, growth does not always show only intentional effects following a fracture that has taken place. Growth disturbances also occur.
Stimulative growth disorders
Stimulatory growth disorder is defined as an excess growth of the bone due to stimulation of the adjacent growth plate. These are to be expected after all growth-age fractures in varying degrees. Pronounced stimulatory growth disturbances occur after performing delayed manipulations (repeated reduction maneuvers) or surgeries beyond day five, as well as when remodeling is prolonged, and may last up to a maximum of two years. Accordingly, to avoid protracted stimulation of the joint, no relevant malpositions (varus, valgus, ante- or recurvation, or lateral displacement) should be left to the corrective forces of further growth, if possible [2].
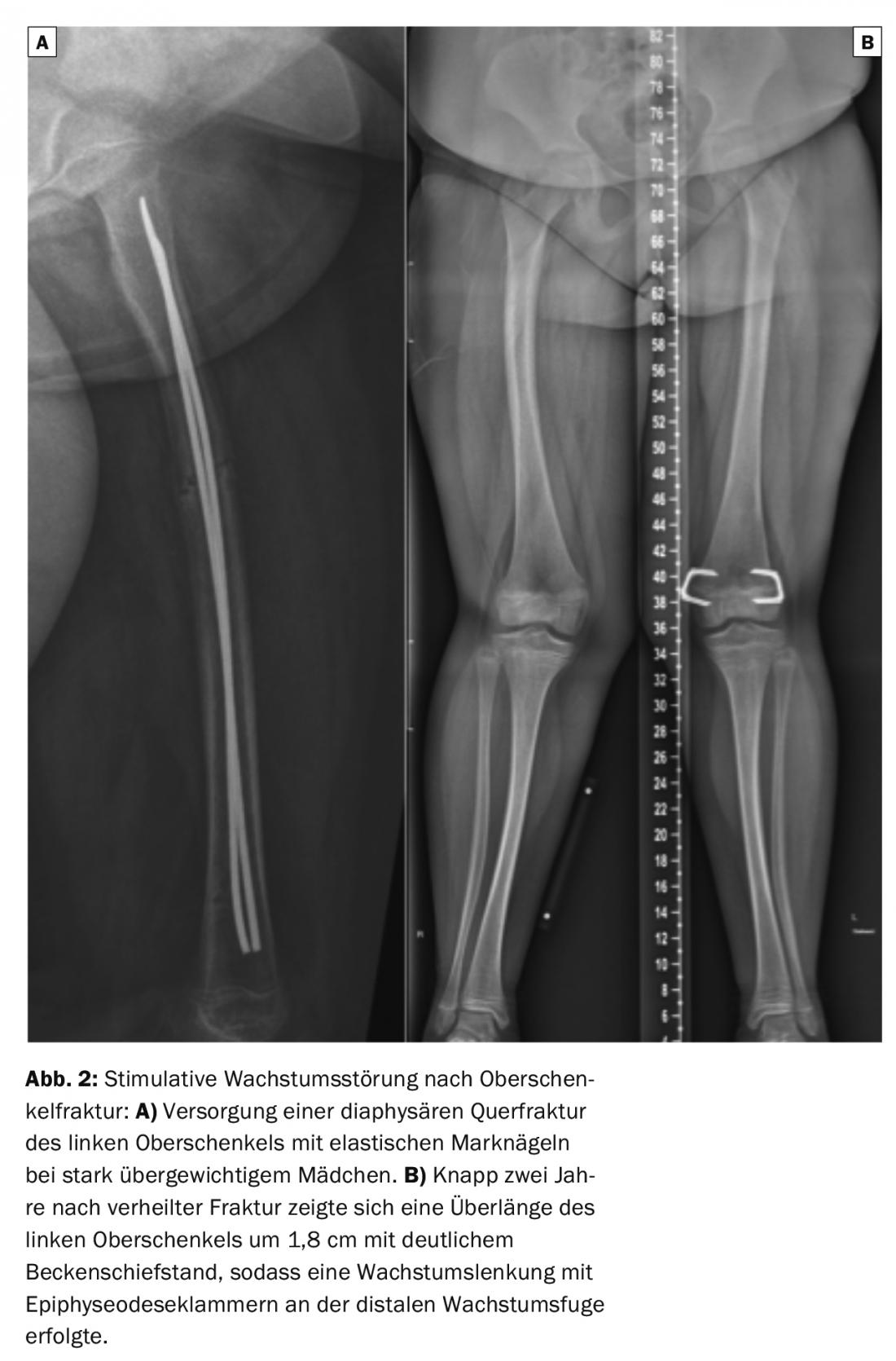
Shaft fractures of the femur at school age are now frequently treated with elastic intramedullary nails (Fig. 2) [4]. It has been shown that a smaller diameter of these elastic intramedullary nails is a risk factor for greater incremental growth. Probably, the protracted stimulation due to the less stable supply is also the reason for the stronger additional growth in this case [5]. The use of elastic intramedullary nails allows material removal after only four months [4] – at a time when no significant leg length difference is yet apparent. Unfortunately, further follow-up examinations are often not performed, and a leg length discrepancy that occurs in the course often remains undetected. Accordingly, it is useful and desirable if the general practitioner resp. pediatrician pays special attention to a possible leg length discrepancy in such situations on the occasion of screening examinations. Although an unfavorable load on the back must be assumed only from a leg length difference of more than 1.5 cm, it is less the absolute value than the functional effect on the spinal statics that is decisive. Functional examination with board pad under the shorter leg allows observation of the influence on the pelvic position and symmetry of the waist triangles. If there are clearly asymmetric conditions that only improve relevantly after underlayment of 1 cm or more, further orthopedic clarification is advisable.
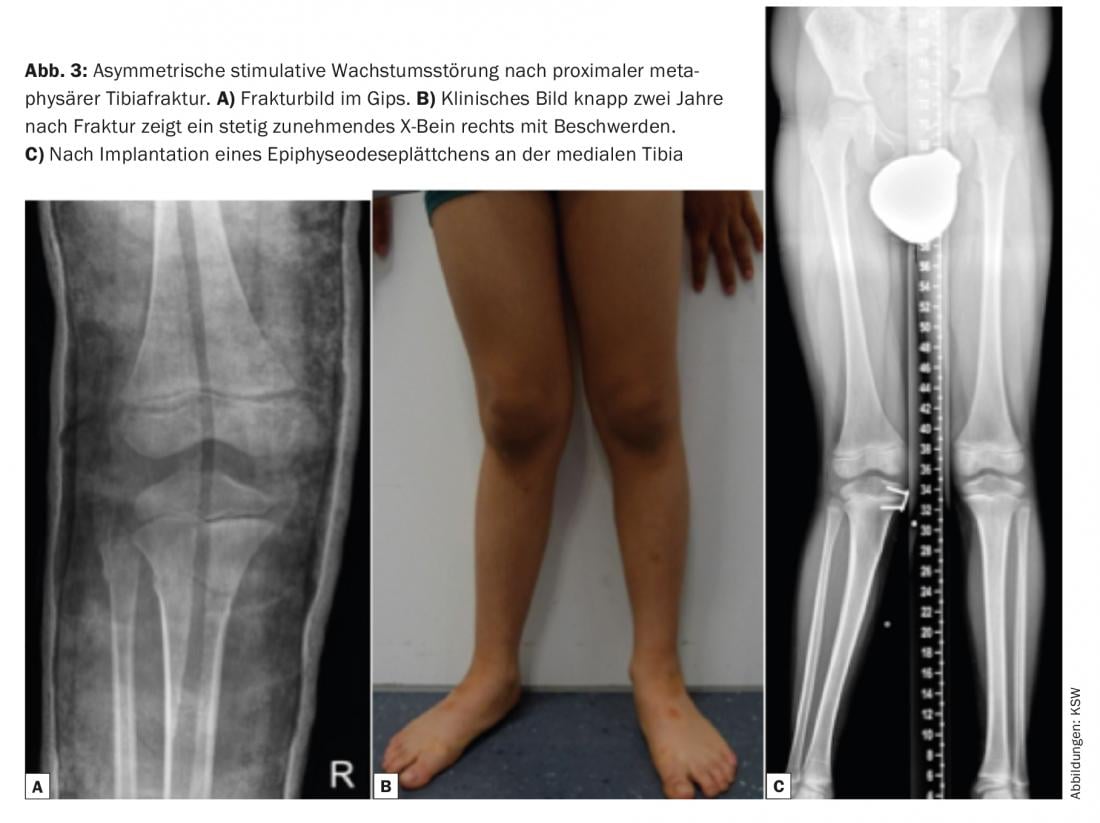
Asymmetric stimulatory growth disturbances may also occur with certain fractures. A prime example of this is the metaphyseal proximal tibia fracture, which actually appears trivial in the first instance (Fig. 3). In this case, stimulation of the nearby growth plate of the medial tibia can lead to the development of an increasing bow leg, which in many cases requires surgical intervention.
Inhibiting growth disorders
Inhibitory growth disorders may occur after fractures passing directly through the growth plate. This can lead to a partial closure of the joint or to a loss of adhesion. of a bone bridge bridging the joint, resulting in an axial defect. Complete closure of a growth plate is less common and is more likely to occur with joint injuries in children near the end of growth. The resulting shortening of the affected skeletal segment is therefore usually no longer clinically relevant. Such inhibitory growth disturbances occur significantly more often in the lower extremities (about 30%) than in the upper extremities (3%) after joint fractures. Accordingly, it is important to provide the patient resp. to inform his family about it in case of joint injuries of the lower extremity.
In Salter-Harris type II fractures that do not cross the growth plate, inhibitory growth disturbances occur at the distal radius in 0-4% of cases depending on the study [6], but at the distal femur in more than half of cases [7]. One reason for this difference may be that the growth plates of the lower extremity must have greater strength against mechanical stress. Disruption of this growth plate therefore requires a trauma of higher energy with a correspondingly higher risk of damaging the growth plate. In these cases, the occurrence of growth disturbance must be viewed as “fated” and directly caused by the trauma. Whether anatomic reduction of these fractures that do not cross the joint can reduce the risk of growth disturbance is questionable based on the data available. Nevertheless, restoration of the correct anatomical axes and stable fixation in plaster or with wires or screws certainly seem advisable.
The situation is different for Salter-Harris III and IV type fractures crossing the growth plate. In these fractures, the joint is usually involved and a dislocated fracture therefore inevitably leads to a step in the joint (joint fracture). Dehiscence at the level of the growth plate can fill with bone during fracture healing and lead to a bridge. Very small bony bridges cannot slow growth or are blown up by growth. In the case of a vertical displacement of the two fragments, difficult-to-treat malpositions usually occur after healing. The prime example here is the Salter-Harris III/IV fracture of the medial malleolus (so-called McFarland fracture, Fig. 4) . The cranial displacement of the medial malleolar fragment forms a bone bridge on the inner side. Further growth on the outside of the tibia and fibula results in varus malalignment of the upper ankle, the most common upper ankle growth disorder [8]. Accordingly, for fractures crossing the growth plate, proper treatment can minimize, although not completely eliminate, the risk of inhibitory growth disturbance.

Fracture aftercare and therapy options for growth disorders
In contrast to fractures of the upper extremity, the author considers follow-up after meta-diaphyseal fractures of the long bones of the lower extremity after at least two years to be reasonable in order to detect any pronounced stimulative growth disturbance with resulting relevant leg length difference. In the case of growth plate fractures, the control intervals must be individually adjusted depending on the age of the patient. For early detection of a growth disorder, the so-called “Harris growth arrest lines” have proven to be helpful. These are radiologically well visible lines corresponding to multisclerosis of the bone. They occur regularly after trauma and should move away from the growth plate in parallel over continued growth (Fig. 4C) – if not, this may be an early sign of growth disturbance. It is useful to perform a CT scan to identify bone bridges. Small bone bridges can be drilled out and filled using bone cement or fatty tissue to allow regrowth if necessary. In the case of a large bone bridge, only the entire growth plate can be surgically closed to prevent a more pronounced axial malposition. For the correction of stimulative growth disturbances, growth guidance (epiphysiodesis) is often used, in which the growth plate is temporarily bridged with a platelet or a staple and thus slowed down (Fig. 2 and 3). In cases of pronounced shortening or axial malalignment, complex reconstructions with bone lengthening via an external ring fixator or an intramedullary nail are necessary.
Take-Home Messages
- Stimulative growth disturbances occur after any meta-diaphyseal fracture in childhood and usually result in increased length growth. They can last up to two years.
- Fractures directly affecting the growth plate are classified according to Salter-Harris. Following such a fracture, stunted growth may occur. These occur significantly more frequently in the lower extremities.
- Children should be checked for leg length discrepancy after a fracture of the long tubular bones of the lower extremity at two years. For growth plate injuries of the lower extremities, individual follow-up by a specialist is recommended.
Literature:
- Salter RB, Harris WR: Injuries Involving the Epiphysial Plate. J Bone Joint Surg Am 1963; 45(3): 587-622.
- Laer L, Kraus R, Linhart WE: Fractures and dislocations in growing age. 6th ed. Thieme-Verlag 2012.
- Flynn J: Rockwood & Wilkins Fractures in Children. Lippincott Williams and Wilkins 2014.
- Lascombes P: Flexible Intramedullary Nailing in Children: The Nancy University Manual. Springer 2009.
- Park SS, Noh H, Kam M: Risk factors for overgrowth after flexible intramedullary nailing for fractures of the femoral shaft in children. Bone Joint J 2013; 95-B(2): 254-258.
- Larsen MC, et al: Outcomes of Nonoperative Treatment of Salter-Harris II Distal Radius Fractures: A Systematic Review. Hand (N Y) 2016; 11(1): 29-35.
- Basener CJ, Mehlman CT, DiPasquale TG: Growth disturbance after distal femoral growth plate fractures in children: a meta-analysis. J Orthop Trauma 2009; 23(9): 663-667.
- Schneider FJ, Linhart WE: Posttraumatic complications of the pediatric ankle. Orthopaedic 2013; 42: 665-678.
HAUSARZT PRAXIS 2017; 12(10): 16-20











