It’s only when you get into rheumatoid arthritis and all of its facets that you realize how multifaceted this disease can be and that it plays into dermatology in so many ways. Rheumatoid arthritis presents not only with its classic nodules and associated symptoms, but also associated neutrophilic dermatoses, autoimmune diseases, TH-1 weighted dermatoses, and lastly side effects of drug therapy ranging from allergies to intolerances to induced autoimmunity. The panorama is opened here.
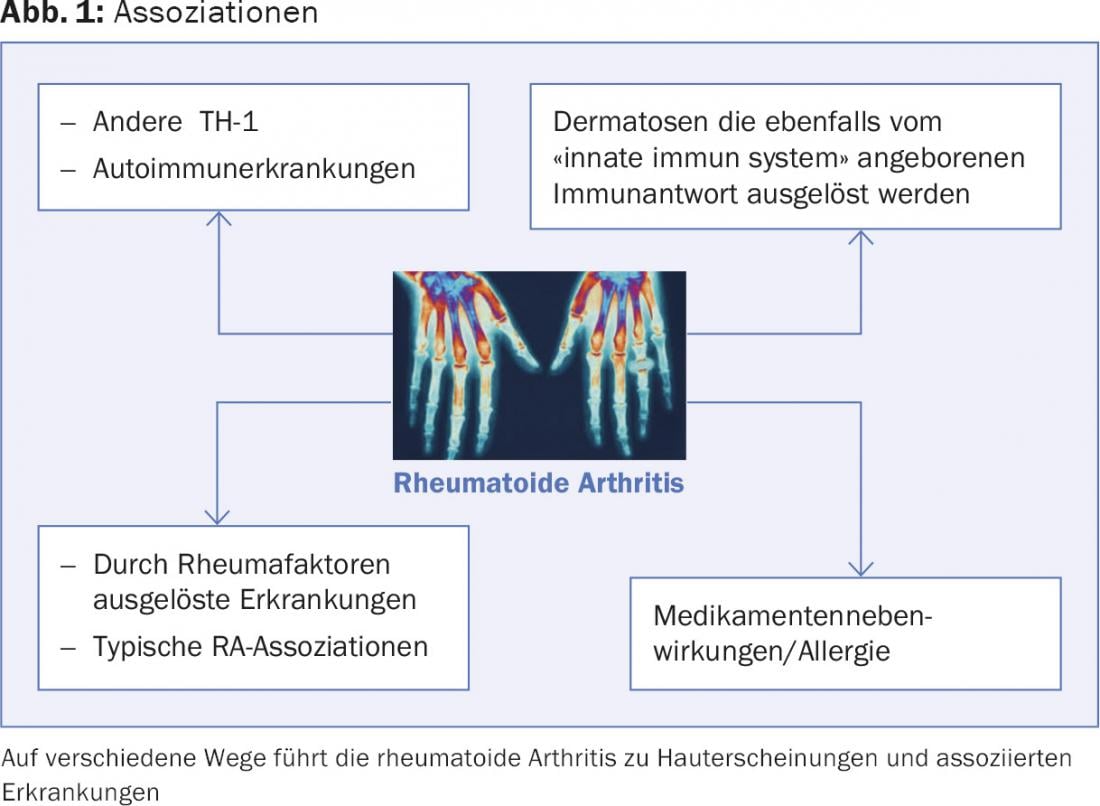
Rheumatoid arthritis (RA) is a multisystem disease that affects not only the musculoskeletal system, but also other organs, and contributes to systemic inflammation and skin inflammation through circulating antibodies. Classification and diagnosis are made using EULAR/ACR criteria that measure joint involvement and CCP antibodies, rheumatoid factors, and CRP, as listed in Table 1 [1]. However, the manifestations go individually strongly beyond this and the skin, autoimmunity, the innate immune system and the drugs or their immunosuppression play a large role (Fig. 1).

RA is a multisystem disease with a TH-1 shift and a cytokine pool that has increased IL-6, IL-1β, TNFα, and IL-17 [2]. In addition, there is already overlap on a genetic basis with psoriatic arthritis, type 1 diabetes, systemic lupus erythemathodes, less so with Crohn’s disease, ulcerative colitis, and multiple sclerosis. So-called susceptibility loci are shared with these autoimmune diseases (TNFAIP, IL-2/IL-21, PTPN22).
RA: TH-1 and other autoimmune diseases
RA not only shares genetic alleles with other diseases, but is also clustered with other autoimmune diseases because of a favorable TH-1 profile of the immune response.
First of all, I would like to mention the so-called rhupus syndrome, an overlap between rheumatoid arthritis and lupus erythemathodes, often also with antibodies of both diseases, photosensitivity and lupus specific involvement of internal organs especially of the heart and kidney incl. Vasculitis. However, in some cases, only skin involvement of lupus erythemathodes such as discoid lesions, the subacute cutaneous variant, or lupus panniculitis are found without meeting the criteria for systemic lupus [3].
Overlap of RA with other collagenoses is also not uncommon (anti-phospholipid AK syndrome, MCTD, Sjeogren’s syndrome). Also, association with psoriasis vulgaris, a typical representative of TH disease, is possible. In general, it is important to distinguish RA from psoriatic arthritis, whether radiologically with the typical involvement of the peripheral finger joints in psoriasis, or by looking for evidencing clinical signs of psoriasis vulgaris (oil spots on the nails; plaques extending beyond the hairline, histopathology).
Mention must also be made of the frequent association with autoimmune bullous skin diseases such as bullous pemphigoid, pemphigus vulgaris, and epidermiolysis bullosa acquisita.
Dermatoses that are also triggered by the “innate immune system”, the innate immune response
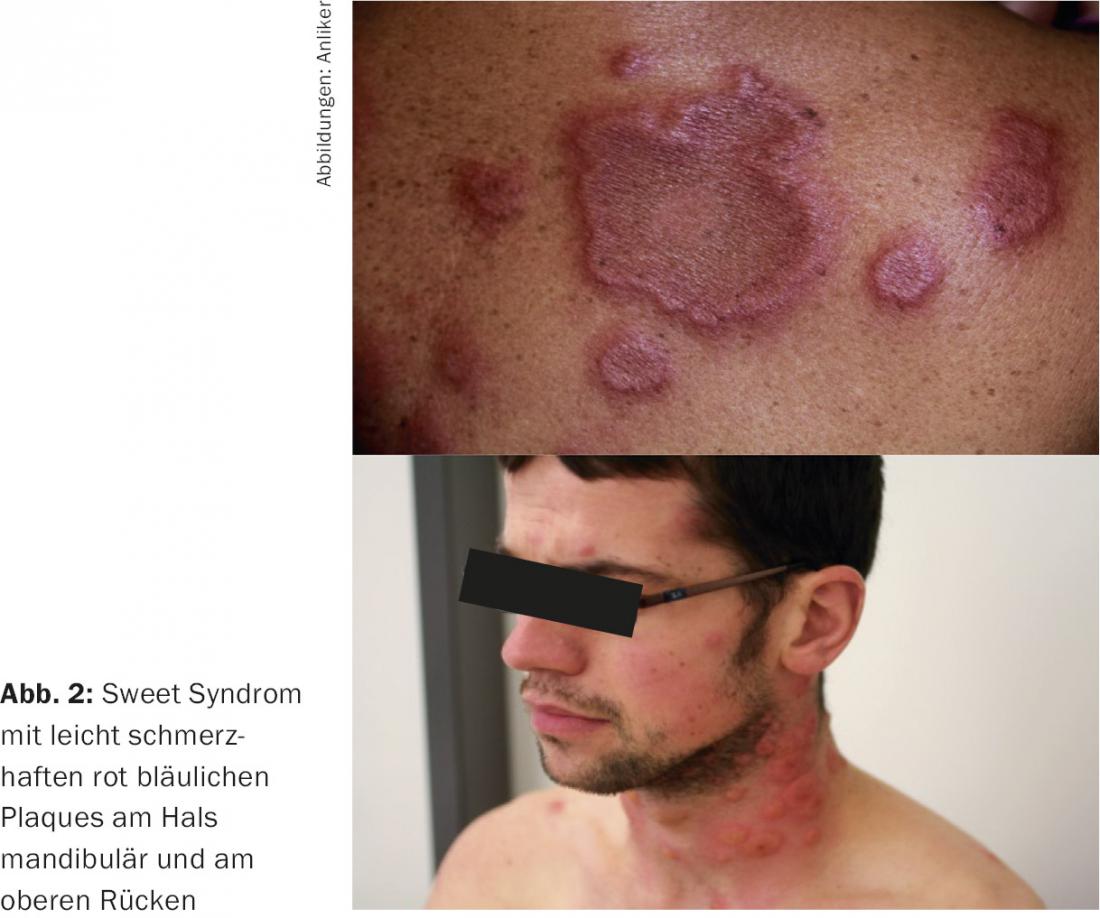
Since RA is strongly driven by the activity of the innate immune system, thus not only by autoantibodies, we find a frequent association with the so-called neutrophilic dermatoses, which are also readily referred to as autoinflammatory. These have mostly been classified accordingly in the recent past and include inflammatory dermatoses such as pyoderma gangrenosum, erythema nodosum, erythema elevatum et diutinum, and Sweet syndrome. In the latter case, which is not uncommon in RA patients, the affected person suffers from general symptoms such as fever, fatigue, swelling of the lymph nodes, greatly increased sedimentation and neutrophilia in the blood count, which is why an infectious process is often thought of. However, the appearance of strongly succulent, highly erythematous bluish plaques on the face, neck, and upper trunk are indicative (Fig. 2) . The diagnosis is made by histopathology, the combination of the various symptoms and the absence of infection. Sweet syndrome is very steroid sensitive.
The diagnosis of pyderma gangrenosum and its therapy is also tricky because, first, the histopathology is poorly characterized and, second, appropriate laboratory tests are lacking. It is markedly inflammatory and occurs even though immunosuppression is often already present. Thus, it is often necessary to switch to high-dose steroids and/or cyclosporine with a very long phase-out period.
RA typical or RA specific manifestations
In the skin changes typical of RA, there are quite distinct skin diseases and changes triggered by rheumatoid factors themselves. Probably best known are the rheumatic nodules, which occur in 20% of patients, mostly on the elbow, ear, hands, sacral, in general mostly near the joints and especially in severe courses of RA. (Fig. 3). The rheumatic nodules are probably due to vasculitis. Histopathologically, they are characterized by a small zone of necrobiosis and much nuclear dust as well as neutrophil-rich inflammation; clinically, one usually finds nut-sized pink to skin-colored nodules. In addition, band-like subcutaneous fibrosis occasionally occurs in the immediate area.


Rheumatoid papules, on the other hand, are usually very small and can be found on the fingers. These are usually painless. Interstitial granulomatous dermatitis with plaques is characterized by large, faintly erythematous map-like fields with band-like borders. It is a typical association with rheumatoid arthritis (Fig. 4). It is treated topically with steroids and systemically with hydroxychloroquine and dapsone [4].
Another typically RA-associated skin disorder is palisade neutrophilic granulomatosis, which manifests with rather dusky maculopapules and plaques over the elbow hand edge or back; this dermatosis is not always easily distinguishable from the previously described disease. Again, as in interstitial granulomatous dermatitis, the overactivity of the innate immune system is triggering and the response to internal steroids is striking [5].
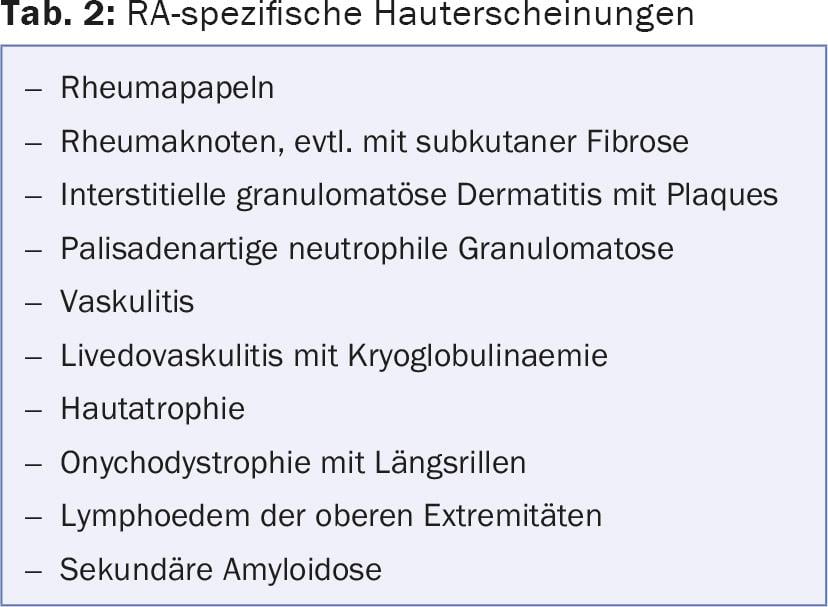
Other skin conditions in RA include skin atrophies that are not only steroid-related such as onychodystrophy with longitudinal grooves, but also with hyperpigmentation of the skin, lymphedema of the upper extremities, and secondary amyloidosis with involvement of the kidney, liver, and spleen (Table 2).
Finally, the rheumatoid factors themselves lead to vasculitis, which may manifest on the skin and may also appear as a livedovasculitis and palpable purpura due to cryoglobulin properties of the rheumatoid factors.
Drug side effects, allergy and intolerance
The side effects of the drugs taken or injected vary, of course, from the mode of action of these substances. First and foremost is the side effect of immunosuppression, which can be manifold with the older preparations such as methotrexate and azathioprine and primarily affect the cellular defense system including the defense against skin carcinomas.
With the so-called biologics, the risks of infection are lower, although a particular weakness against the defenses of tuberculosis and lymphoma should be noted, and this is especially true for the TNFα-blockers. These can also induce a whole range of other side effects. The first to be mentioned is certainly paradoxical psoriasis under TNFα-blockade (Fig. 6) [6], which is due to the sudden overweighting of the innate immune system and may also have a strong neutrophilic even pustular touch. In addition, the triggering of dermatomyositis has also been described. In addition, veritable allergic reactions of the immediate type up to anaphylaxis occur repeatedly. Ultimately, the triggering of lupus erythematosus by these substances is not uncommon. This applies in particular to infliximab and adalumimab. From the last preparation, I examined eight affected individuals, all of whom had very atypical and sparse lupus symptoms; photosensitivity and vasculitis were predominant, but the development of lupus panniculitis was also observed. Frequent detection of anti-histone antibodies has been successful [7].


Certainly more frequent is the intolerance reaction to non-steroidal anti-inflammatory drugs (NSAIDs), especially the Cox-1 inhibitors, which can lead to urticaria, bronchial asthma and anaphylaxis in affected individuals and according to the genetic predisposition. This occurs because of a weighting of the degradation of these preparations via the cycloxigenase pathway with accumulation of bradykinins. Typically, all analgesics of this group can cause symptoms depending on the quantity: Aspirin, diclofenac, ibuprofen, novamine sulfone, and mefenamic acid. In general, Cox-2 inhibitors (e.g., celecoxib) and acetaminophen, which has only 10% Cox-1 activity (however, 4% of NSAID intolerants cannot take acetaminophen either), as well as the opiates and opioids, go. However, these should be tested out.
Allergic reactions to analgesics are also possible, mostly as a late-type drug reaction: to antirheumatic drugs, methotrexate, less so to biologics.
In addition, photoallergic reactions have also been described with various immunosuppressants (MTX, azathioprine) (Fig. 8); however, these are also known for diclofenac, ibuprofen, piroxicam, and dapsone and are usually found only after almost detective allergological work and testing with UV provocation.

Conclusion
Rheumatoid arthritis shows manifold overlaps with dermatology and allergology, which come to bear in quite different ways, either by induction of the innate immune system with the development of neutrophilic diseases, or by overlaps and associations with other autoimmune diseases and autoimmune dermatoses. In addition, skin symptoms and infections occur due to immunosuppression and intolerance or allergy in the treatment.
Literature:
- Müller R, et al: Criteria for the classification or diagnosis of rheumatic diseases. Pharmacum healthcare marketing gmbh, Druckerei Emmensee. 2nd ed. 2011.
- McInnes IB, et al: Cytokines in the pathogenesis of rheumatoid arthritis. Nature Reviews Immunology 2007 June 7: 429-442.
- Panush RS, et al: “Rhupus” syndrome. Arch Intern Med. 1988 Jul; 148(7): 1633-6.
- Tomasini C, et al: Interstitial granulomatous dermatitis with plaques. J Am Acad Dermatol 2002;46:892-9.
- Sangueza OP, et al: Palisaded neutrophilic granulomatous dermatitis in rheumatoid dermatitis. J Am Acad Dermatol 2002;47: 251-7.
- Joyau C, et al: Anti-tumour necrosis factor alpha therapy and increased risk of de novo psoriasis: is it really a paradoxical side effect? Clin Exp Rheumatol. 2012 Sep-Oct; 30: 700-706.
- Anliker M, et al: Lupus-like features and lupus erythematosus induced by adalimumab. Characterisation in a series of 5 patients. Poster Annual Meeting SGDV 2011.
DERMATOLOGIE PRAXIS 2016; 26(5): 18-22











