Shoulder injuries are among the most common sports injuries and show a wide spectrum. Proper clinical and imaging assessment helps to detect structural damage and initiate appropriate therapeutic measures. It often makes sense to treat injuries promptly in order to achieve the best possible functional result in terms of reconstruction. A large number of injuries can be treated less invasively and often arthroscopically. Well-guided rehabilitation is important and can continue to bring improvements for up to a year after shoulder injury.
Depending on the sport, the shoulder is one of the joints most frequently affected by injuries. For many sports, the shoulder is the central element in the movement process and is therefore exposed to particular stresses. Due to the high mobility of the joint and the complex anatomy required for this, a wide range of injuries can be found. In principle, acute injuries must be distinguished from overuse injuries (“athlete’s shoulder”).
Medical history
Taking a history helps to understand common injury patterns to narrow down specific injuries. The orientation of the arm in space at the time of injury and the direction of the applied force are important. Furthermore, there are sports with typical injury and stress patterns.
Clinical examination
The examination is performed on the undressed patient and in lateral comparison. Often, asymmetries are already noticeable. Typical inspection findings include atrophies of the musculature as well as injuries of the acromioclavicular (AC) joint with prominent lateral clavicle and the so-called “Popeye deformity” in ruptures of the long biceps tendon.
A cursory examination of the pain-free range of motion of the cervical spine (C-spine) is recommended to rule out the major differential diagnoses of shoulder pain. Palpatorily, the AC joint is easily accessible (pressure dolence, “piano key phenomenon”), pressure pain in the sulcus bicipitalis indicates injuries of the long biceps tendon.
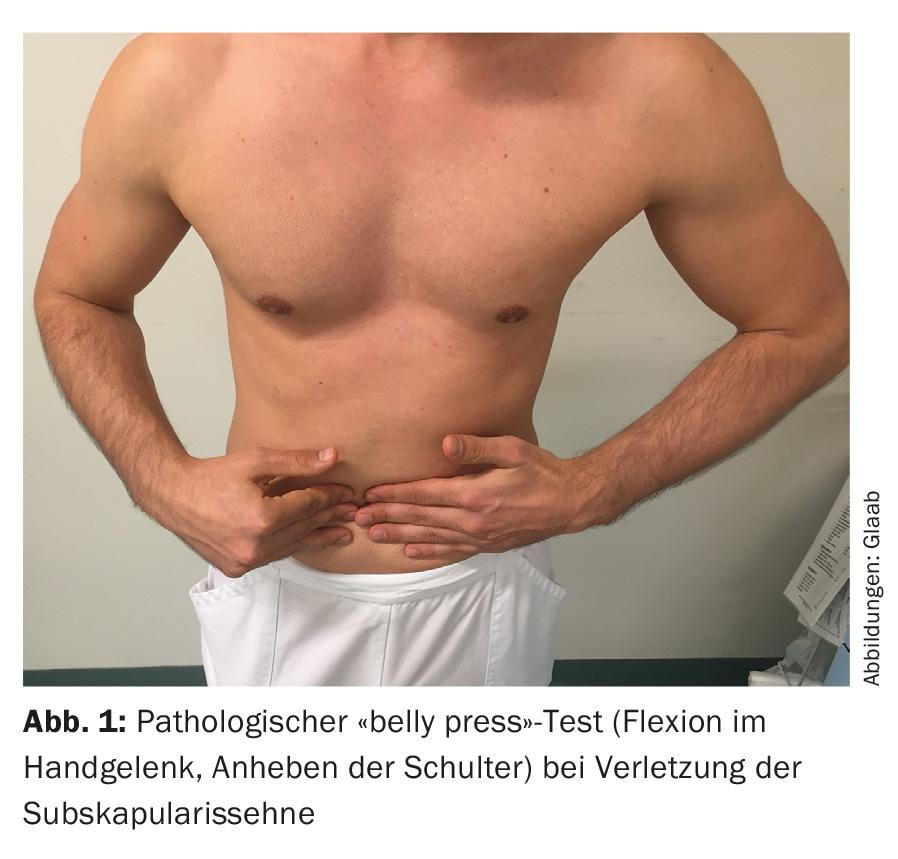
Testing of active range of motion in lateral comparison includes flexion and extension, abduction and adduction, and internal and external rotation. Limitations compared to passive range of motion or in lateral comparison are good indicators of a loss of function of the corresponding muscles. Functional testing of the musculature is performed for the deltoid muscle by abduction from adduction or holding the submaximal extension (“extension lag sign”), for the subscapularis muscle e.g. by the “lift off” (lifting the hand behind the back is not possible) or “belly press” (Napoleon) test. (Fig. 1). The supraspinatus muscle can be tested with the Jobe test (holding function in 90° abduction/30° horizontal flexion in internal rotation, “empty can” variant) and the 0° starter test (reduction in force during abduction); in the case of injuries to the infraspinatus muscle, the external rotation force (“lag sign” of external rotation) is limited. These tests actually describe a loss of strength and are often difficult to differentiate in the acute setting due to pain. Thus, they are sensitive but not very specific.
If a shoulder dislocation is suspected, the apprehension sign (defense during abduction in external rotation) and the relocation test (Fig. 2) are helpful. Biceps tests are not considered very specific, but pain radiating into the upper arm is typical.

Imaging: X-ray, CT, sonography, MRI
Initial imaging after injury is performed using appropriate conventional methods in defined multiple planes. CT, (arthro-)MRI or ultrasound represent complements. The advantage of dynamic examination in ultrasound does not always compensate for the strong examiner dependence.
Proximal humerus fractures
Fractures of the proximal humerus are rare sports injuries and typical “high impact” injuries in healthy bone, e.g., in motocross, cycling, or skiing (Fig. 3). The diagnosis is confirmed conventionally radiologically by means of ap/Neer and, if necessary, axial image. In unclear, more complex situations, a computer tomography follows.
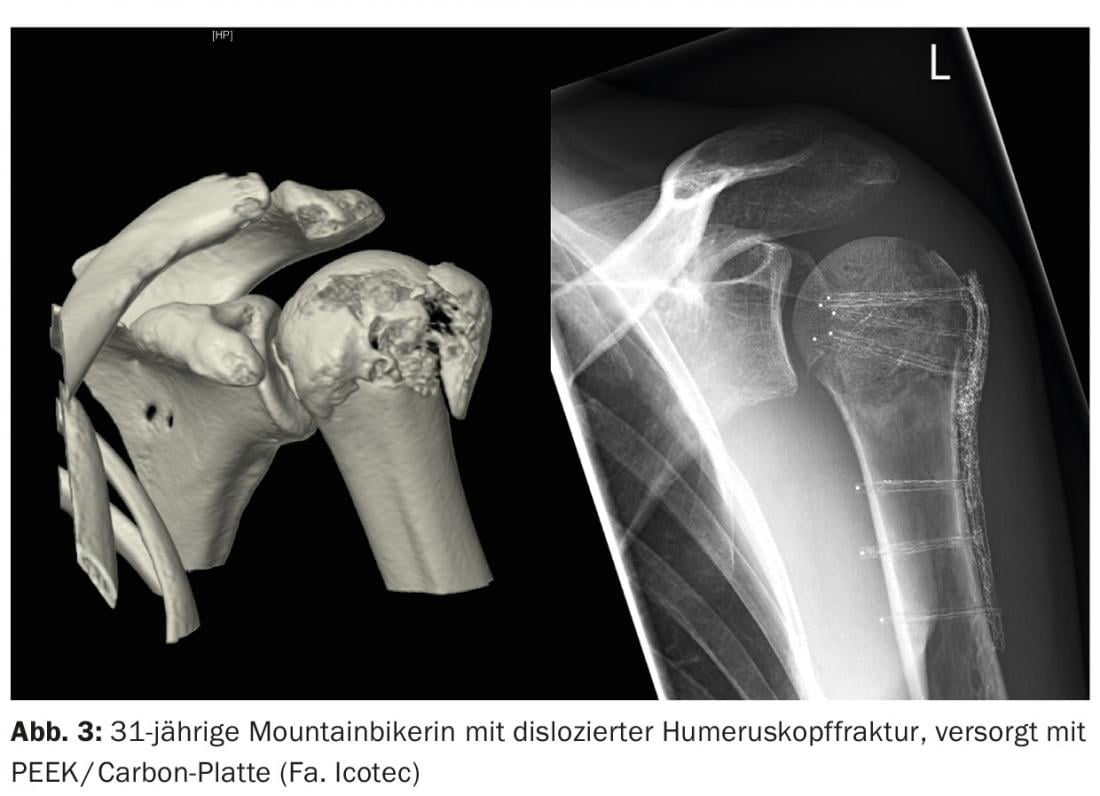
Undislocated or stably valgus-impacted fractures qualify for conservative therapy. After a short immobilization phase, passive mobilization (pendulum exercises) can be started. If the situation remains radiologically stable (follow-up after approx. ten days), active-assistive treatment without loading with gradually increasing range of motion can be continued for approx. six weeks. Dislocated and unstable fractures are usually treated with angular stable plate osteosynthesis and tension taping of the tubercula. Dislocated fractures of the tubercula correspond to osseous injuries of the rotator cuff and should be treated surgically.
Clavicle fractures
Fractures of the clavicle are among the most common injuries, especially in cycling, but also in winter sports. The cause is usually indirect trauma with a fall on the shoulder while the arm is applied. Approximately two-thirds of all fractures are localized in the middle third. Clinically, in addition to the local pressure pain and palpable steps, crepitus is often apparent. Radiological clarification is performed by an ap and a tangential image of the clavicle. Undislocated fractures are treated conservatively and functionally, at most in a sling to reduce pain.
Open fractures, threatening perforating fractures, and fractures with accompanying neurovascular lesions should be treated surgically. Other surgical indications include shortening greater than 15 mm and axis deviation greater than 20°. Patients after surgical procedures are free of pain faster and have less pseudoarthrosis. For simple fractures, minimally invasive procedures (e.g. elastic titanium nails, Fig. 4) are possible ; more complex fractures are treated with plate osteosyntheses.

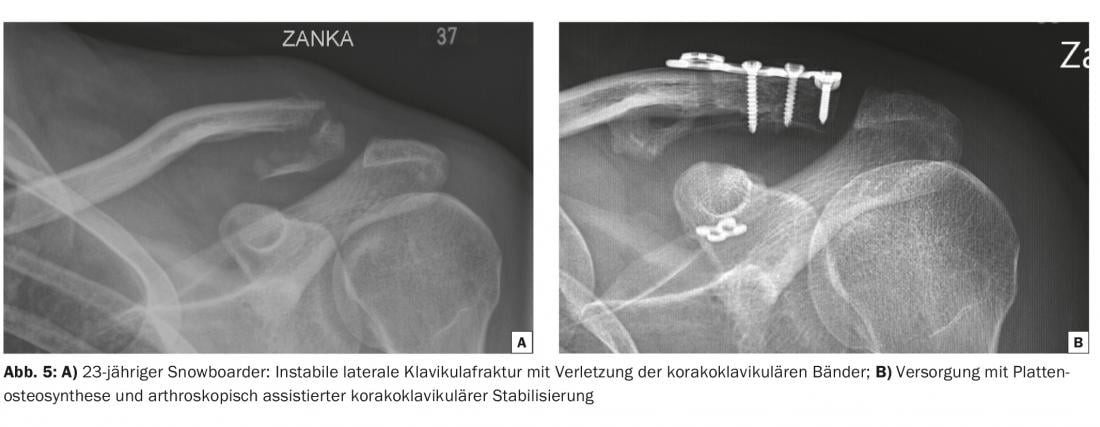
Up to 30% of clavicle fractures are located in the lateral third. An important anatomical detail here is the coracoclavicular ligaments, which secure the connection between the clavicle and the scapula. If these are also injured, dislocation occurs due to the weight of the upper limb. These fractures heal poorly and should rather be operated on – depending on the fracture type, surgery is performed with plates, hook plates or with arthroscopically assisted coracoclavicular stabilization at most ( Fig. 5).
Injuries of the acromioclavicular joint
Injuries to the acromioclavicular joint also usually result from a fall onto the applied arm, less commonly onto the extended arm. This can result in injury to the tight capsule of the AC joint, the coracoclavicular ligaments, and even injury to the surrounding muscle fascia. Clinically, the local pressure dolence and, in higher-grade injuries, the lateral clavicle end, which is prominent in a lateral comparison, with a vertical and often also horizontal instability is impressive. Vertical instability is confirmed radiologically in the shoulder/clavicle ap image, more specifically with a Zanca image. If anything is unclear, a side comparison image (panorama) under load can help. Horizontal instability can be at least partially visualized in axial radiographs of the shoulder. Classification is according to Rockwood (I-VI).
Low-grade Rockwood type I-II injuries characterized by isolated injury to the AC joint capsule can be treated functionally (sling only as pain therapy). Higher grade injuries (Fig. 6) involving the coracoclavicular ligaments cannot be retrained by the weight of the arm and should rather be operated. In order to achieve sufficiently tight healing of the injured ligaments, the operation should be performed quickly (max. 14 days after accident). Among the many surgical procedures, the hook plate (metal removal obligatory) and arthroscopically assisted coracoclavicular stabilization with pulley systems and possible acromioclavicular suture cerclage are most commonly performed today. Weight-bearing activities above head height are allowed again after four months at the earliest. Missed symptomatic injuries should be biologically augmented with tendon grafts.

Shoulder dislocation
Dislocation of the shoulder joint is one of the most common sports injuries. In most cases, there is an anterior-inferior dislocation due to a forced abduction-external rotation movement, followed by posterior dislocations (more common in seizure disorders, electrical accidents) and very rarely purely inferior dislocations (luxatio erecta). Clinically, the patient is characterized by a relieved posture with painful functional limitation and a prominent acromion (epaulet phenomenon). It is important to check and document the function of the axillary nerve (deltoid muscle), which is frequently also injured.
Before attempting reduction, one should exclude a fracture radiologically (ap/Neer). A posterior dislocation (Fig. 7) is often difficult to recognize; a precise medical history is also helpful. In addition to adequate analgesia, the patient and the surgeon need to be as relaxed as possible in order to reduce the shoulder.

Self-repositioning maneuvers such as those according to Stimson (Fig. 8) in the prone position with the arm hanging down or according to the Davos method are also possible.

Successful reduction is followed by immobilization on the body, re-testing of the deltoid muscle function and radiological documentation of the reduction. Any concomitant osseous injuries such as glenoid rim fractures (Fig. 9) or tears of the rotator cuff can already be identified in this way and, if necessary, further clarified with computed tomography. Soft tissue associated injuries such as labral and capsular lesions, biceps anchor injuries and rotator cuff injuries can be further clarified on MRI. We consider MRI to be indicated in patients younger than 30 years and in patients with pseudoparalysis or functional impairment during clinical controls in the course. In particular, patients under 30 years of age with a high functional demand above the horizontal have a high risk of reluxation and should therefore rather be treated surgically in case of corresponding injuries.

Immobilization with conservative therapy is performed for 7-14 days after analgesia. Physiotherapeutic exercise to balance the shoulder stabilizing muscles can be started immediately.
Today, arthroscopic reconstruction of the labrum and capsule with suture anchors is considered the standard procedure for shoulder stabilization in soft tissue injuries. The risk of recurrence after these operations is approximately 12%. In larger glenoid defects, which often occur after recurrent dislocation, bony augmentation with bone chip or coracoid transfer (after Latarjet) is often necessary.
Injuries of the long biceps tendon
Injury to the intra-articular long biceps tendon can occur by several mechanisms. The complaints, which are often described posteriorly and radiate into the ventral humerus, are difficult to assign, with pressured dolence in the sulcus, painful biceps function tests (supination/flexion), impingement symptoms, and even jumping of the tendon in the case of injuries to the biceps pulley. Arthro-MRI is only moderately reliable in detecting injuries to the biceps anchor (SLAP lesions: superior labrum from anterior to posterior) and biceps pulley, and they are often only confirmed arthroscopically. Reconstruction techniques are promising in young patients. More pragmatic is the tenotomy of the long biceps tendon. Complete ruptures of the long biceps tendon are usually the result of degenerative changes and are in the majority only a cosmetic problem; the function is taken over by the short head of the muscle. There is the possibility of tenodesis, which is then usually performed subpectoidally.
Distal biceps tendon rupture
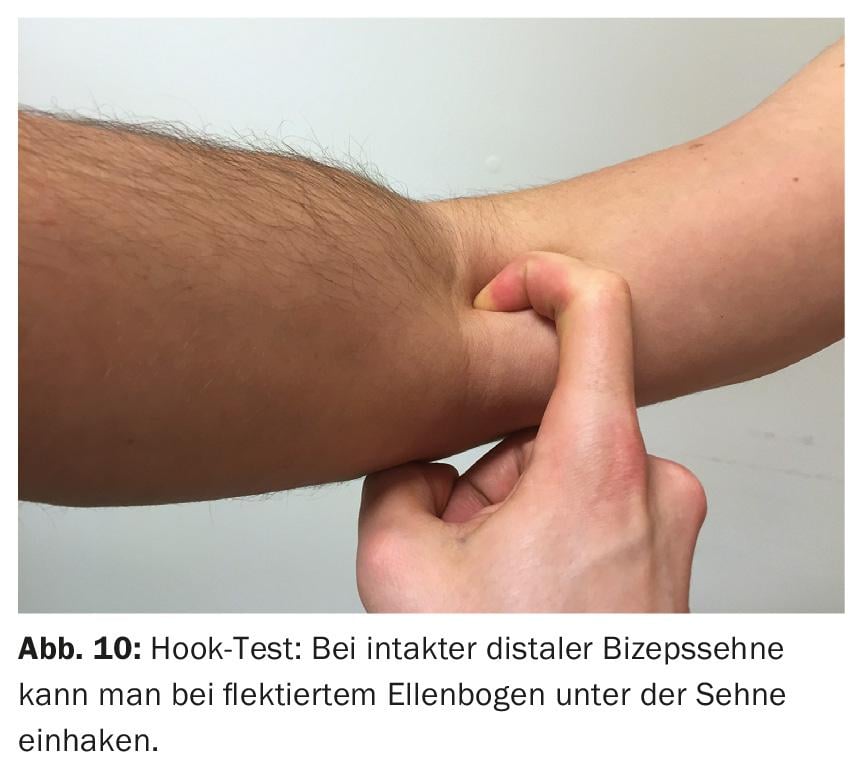
Most often, lifting a load under flexion and supination is the cause of a rupture of the distal biceps tendon (e.g., strength training). Patients experience an acute loss of strength and often hear a pop. Clinically, the tendon is no longer palpable; the Hook test is positive (Fig. 10) . Functionally, there is a reduction in force during combined flexion-supination in a lateral comparison. If the diagnosis is not clinically certain, MRI or sonography will help. Since the injury results in complete loss of function, the tendon should be reinserated promptly.
Rotator cuff injuries
With increasing age, injuries to the rotator cuff come to the fore; these are often associated with previous degenerative damage. Patients are often plagued by nighttime pain in addition to limited function. Important clues are provided by the clinical examination with the corresponding functional deficits. Osseous avulsions of the cuff can be adequately visualized by conventional radiology or computed tomography. Otherwise, arthro-MRI or sonography will help to confirm the diagnosis. For traumatic ruptures, prompt treatment is recommended to avoid progression, retraction, and muscle fatty degeneration. Arthroscopy is an elegant way of detecting and treating any concomitant injuries in the joint. The most important goal should be stable anatomical refixation, which can be achieved with suture anchors, for example (Fig. 11) . Restrained follow-up treatment – especially in the case of purely tendinous injuries – is a prerequisite for a good result.

“Terrible triad” of the shoulder
The “terrible triad” of the shoulder refers to a shoulder dislocation with rotator cuff injury and neurologic damage to the axillary nerve or superior brachial plexus. This injury occurs in up to 18% of anterior shoulder dislocations and is often initially overlooked. Up to 90% of neurological symptoms are reversible. With timely rotator cuff refixation, there is a chance of good shoulder function, even if deltoid function does not recover.
“Sportsman’s Shoulder”
The term classically refers to the complaints that occur in throwing athletes such as handball players. This is justified by an adaptation to the athletic load, which leads to hyperlaxity due to the maximum lunging movements. This results in decentering of the humeral head and consecutive combined impingement and instability symptoms. These overloads then lead to pathologies of the rotator cuff (affecting up to 83% of all handball players), the long biceps tendon and its anchor, and the labrum. These overuse injuries not infrequently end in acute complete lesions. Unilateral repetitive stress, such as swimming or climbing, can lead to entrapment and bursitis. Reducing the amount of training and appropriate balance training can help.
Initial therapy
If structural damage has been ruled out, it is usually possible to proceed in a functional, complaint-adapted manner. Immobilization should only be performed for a short period of time (7-14 days) to preserve range of motion as much as possible. Consistent analgesia is equally important. For immobilization, fixations close to the body are usually sufficient (Fig. 12). If the initial assessment is difficult, it is useful to monitor the patient during the course of the procedure. Physiotherapeutic exercise can help to restore coordination of movement and balance the shoulder muscles. Cortisone injections have no place in the initial therapy of injuries.

Further reading:
- Doyscher R, et al: Acute injuries and overuse injuries of the shoulder in sports. Orthopäde 2014; 43(3): 202-208.
- Doyscher R, Scheibel M: Clinical examination of the shoulder – a structured overview. Dtsch Z Sportmmed 2013; 61: 260-266.
- Gyftopoulos S, Recht M: The Throwing Shoulder. The
- Common Injuries and their Underlying Mechanisms. Semin Musculoskelet Radiol 2014; 18(4): 404-411.
- Jensen G, et al: Acromioclavicular joint injuries. Trauma Surgeon 2015; 118: 1041-1055.
- Prudnikov OE, Prudnikov DO: Terrible triad of the shoulder. Upper Extremity 2011; 6: 199-207.
Helpful link:
www.shoulderdoc.co.uk
HAUSARZT PRAXIS 2016; 11(4): 10-15











