Diagnosing nerve pain remains a challenge. According to the current validated standard questionnaires, further clarifications such as quantitative sensory testing are also used, depending on the case. A new study now provided normative data for the back that can be used to analyze and better classify neuropathic pain in this area.
(ag) Neuropathic pain, defined as a direct result of a lesion or disease in the somatosensory system, is common. The causes are varied – for example, herpes infection, multiple sclerosis, or polyneuropathies can cause central or peripheral neuropathic pain. Typical symptoms include burning, tingling, numbness, but also shooting pain or sensory deficits such as decreased perception of cold. However, the symptoms are by no means uniform.
Improve understanding of nerve pain
Quantitative sensory testing (QST), developed in Germany, aims to measure and standardize typical changes in skin sensitivity. Seven tests are used to test the sensation of pain and the perception of cold, heat, sharp and fine touches as well as pressure and vibration. The procedure takes about 30 minutes per test area. It was established by the German Neuropathic Pain Research Network (DFNS). The QST provides a patient-specific sensitivity profile. With the help of this profile, conclusions can be drawn about the nerve damage. For example, it can be answered whether fine or thick nerve fibers are affected or whether the injury is in the central or peripheral nervous system.
How can the results be assessed?
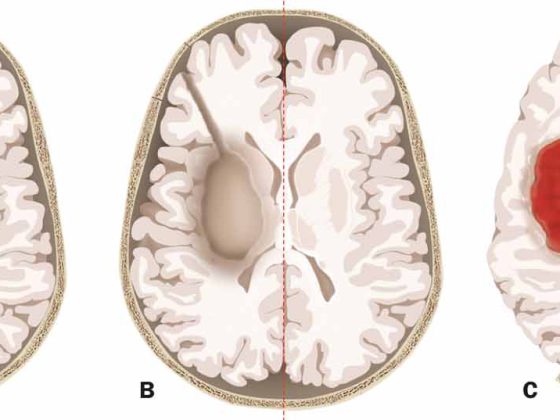
For the best possible assessment of the QST profiles, also especially with regard to a possible targeted therapy that takes into account the specific pain mechanisms, the DFNS provides a database. This currently contains anonymized data from a good 3000 patients and over 600 healthy subjects. Comparison between patient and subject data provides normal values for each QST point depending on age and sex. Thus, respective stimulus responses can be classified as pathological under- or overfunctions. Low functions indicate a lesion in the somatosensory system, and high functions indicate allodynia and hyperalgesia. The findings are systematized with the LoGa classification (Lo = “loss” i.e. loss/negative symptom; Ga = “gain” i.e. increase/positive symptom). With the additional numerical code from 0-3, thermal (1) and mechanical (2) symptoms or their combinations (3) can be collected. The finding of thermal hypesthesia (L1) combined with mechanical allodynia (G2) would thus be classified as L1G2.
The database also allows patients with similar sensitivity profiles to be divided into groups for which specific therapies can be sought.
Back pain
So far, there are age- and gender-related QST standard values for the areas face, foot and hand. In a recent study [1], the aim was to collect reference values also in the back region. Typical sensitivity changes in patients with postzosteric neuralgia should thus be described.
Methods: QST profiles of the back were obtained from 162 healthy subjects. Sensory profiles of other areas were within the normal range.
Results: The QST showed a lower sensitivity of the upper back compared to the hand, and a higher sensitivity of the lower back compared to the foot. However, no systematic differences were shown between the two back areas.
Age played a significant role in most parameters, but gender only insofar as the pain threshold under pressure was significantly lower in women than in men. For the pain threshold in cold, the confidence intervals mostly exceeded the “safety cutoffs”, therefore only relative reference values (difference left-right, difference hand-back) were usable. The subjects were most sensitive to pressure pain.
Application example for postzosteric neuralgia
With the data obtained, hypersensitivity, pain and insensitivity in the back can now be classified into values within and outside the norm.
In the second part of the study, the new standard values were tested directly in practice for their applicability. They compared the values with QST data from more than 70 patients with postzosteric neuralgia. This condition usually affects the back. Interestingly, the analysis revealed sensitivity patterns that differed from those seen in neuropathies of other causes: Compared with the newly obtained reference values, patients showed thermal and tactile deficits and dynamic mechanical allodynia, mostly without a reduced mechanical pain threshold.
In the future, the new data or norm values will enable the precise analysis of the sensitivity changes of a wide variety of pain diseases of the back (post-thoracotomy, chronic back pain), which in the optimal case can also be used for therapy.
Literature:
- Pfau DB, et al: Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): reference data for the trunk and application in patients with chronic postherpetic neuralgia. Pain 2014 May; 155(5): 1002-1015.