At the SGIM Great Update in Interlaken, the most common problems and challenges that a family physician encounters when dealing with patients suffering from lymphoma were discussed. The only difficulty is the meaningful naming: How do you name the more than 70 entities of malignant lymphomas so that it remains comprehensible for the patient and his relatives? Diagnosis and follow-up are also the responsibility of the primary care provider.
Prof. Dr. med. Andreas Lohri from the Cantonal Hospital Baselland opened his presentation with epidemiological data: “The Swiss cancer registries count about 1600 malignant lymphomas per year, a good third of the cases end fatally. This makes lymphomas together one of the most widespread cancers, but if one goes by the WHO classification, this group is divided into more than 70 different entities.”
More than 70% of Hodgkin’s lymphoma patients are disease-free after ten years; for B-cell lymphomas, which are the most common lymphomas, the figure is 40%, and for T-cell variants only 20%. Between 2001 and 2010, there were a total of 16,000 new lymphoma cases, of which approximately 6000 patients survived the disease.
“If you want to name the specific entity, it becomes difficult. While it is still relatively clear in the case of Hodgkin’s lymphoma, the general practitioner usually does not know what name to give diffuse large B-cell lymphoma (DLBCL), for example, so that the condition is also comprehensible to the patient and his relatives. In most cases, he then falls back on the actually obsolete term “non-Hodgkin’s lymphoma”. The Swiss patient organization for lymphoma sufferers and their relatives therefore provides the sufferer with specific information on the twelve most common lymphomas, including the names,” says Prof. Lohri.
Would you recognize lymphoma?
Symptoms may be unclear or lead in the wrong direction. A worldwide survey involving 1606 patients with various lymphoma conditions showed that about 50% visited the doctor for the first time because they had a check-up appointment anyway, or because they generally did not feel well. “So the initial symptoms are quite nonspecific, and the study also showed that in 30% of patients it took more than five months since the first visit to the doctor before the correct diagnosis was made,” Prof. Lohri explained. “About half of all lymphomas are extranodal and present with a wide variety of symptoms: whether neurologic as in CNS lymphomas, cutaneous as in T-cell lymphomas, or renal and cardiac in amyloid-producing lymphomas. Typical B symptoms become apparent quite late, but even before that, some patients complain of fatigue and depression.”
A correct diagnosis, preferably made in collaboration with a specialist, is therefore crucial. Basically, these include:
- a medical history (B-symptoms, family history)
- a laboratory (Hb, Lc, Tc, CRP, EBV, HBV, HCV, HIV, Toxoplasma, Bartonella)
- a status (lymph nodes, wards, spleen size, liver, ENT, skin)
- a biopsy (various tissue tests are available: IHC, FACS, cytogenetics, PCR, FISH).
- an imaging.
“PET provides very good data on disease progression, gives clues for prognosis and facilitates treatment decisions,” Prof. Lohri said.
How does the family doctor accompany the therapy?
Once the diagnosis is confirmed, treatment is usually performed by the specialist; the primary care physician may provide interim blood counts and administration of growth factors and antibiotics.
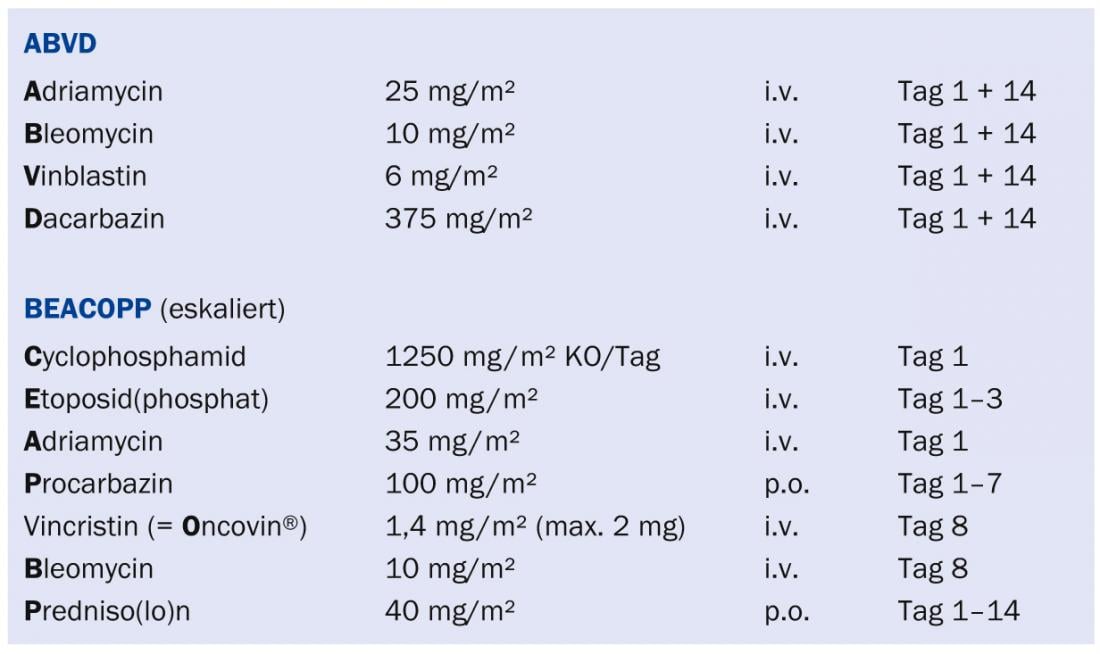
“Therapy algorithms should optimally be planned in an interdisciplinary conference. Basically, the therapy has the goal of curing the patient with a regimen that is as non-toxic as possible and does not cause any side effects later on. This goal has not been achieved to date. New research avenues are therefore needed to further optimize treatment. Nevertheless, one must not forget the great progress that has been achieved with the currently used therapeutic regimens (especially the ABVD regimen in limited Hodgkin’s lymphoma and the BEACOPP regimen in advanced Hodgkin’s lymphoma) (see box) . In B-cell and many other lymphomas, the R-CHOP regimen (with the antibody rituximab) has performed very well. For indolent forms, bendamustine combinations are becoming increasingly important. This drug has an excellent therapeutic index, its main toxicities being cytopenias and skin rashes. Radiation therapy is less frequently used in the curative setting today because the late effects can be significant,” Prof. Lohri explained.
How long are follow-up examinations necessary?
Before 2000, many Hodgkin’s patients received radiation doses, some of them large. According to recent studies, mediastinal irradiation significantly increases the risk of cardiac disease 10 to 25 years after treatment [1]. Since the primary care physician is responsible for the follow-up care of the so-called “lymphoma survivors”, he also has the crucial role of recognizing and correctly diagnosing such late complications.
In the follow-up of irradiated patients, the American College of Radiology recommends screening by stress test and echocardiography from five to ten years after treatment because of the increased cardiac risk.
The risk of second tumors is also increased after radiation therapy: one study showed that about 10% of patients who received radiation at 20 developed breast cancer at about age 50 [2]. Therefore, an MRI of the breast and a mammogram are recommended starting ten years after radiation.
Look into the future
Finally, Prof. Lohri spoke about some relevant innovations in the therapy and diagnosis of lymphoma:
- PET will allow a cure with less aggressive treatments in the future.
- Radiation will be avoided in the curative setting in the future.
- Many new molecular and immunotherapeutic drugs are in development: such as tyrosine kinase inhibitors (ibrutinib), immunomodulators, second generation antibodies.
“The primary care physician must have lymphoma on his diagnostic radar in any case if he detects fatigue, chronic pruritus, anemia, systemic symptoms in viral hepatitis or chronic EBV or HIV infection. But he is also the central contact person in the long-term management of the cured lymphoma patient and thus assumes an important role in the early detection of associated late effects,” Prof. Lohri concluded his presentation.
Source: “Lymphoma: What the GP needs to know”, Seminar at SGIM Great Update, November 14-15, 2013, Interlaken.
Literature:
- Galper S, et al: Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation. Blood 2011; 117: 412-418.
- Dores GM, et al: Second malignant neoplasms among long-term survivors of Hodgkin’s disease: a population-based evaluation over 25 years. J Clin Oncol 2002; 20(16): 3484-3494.
HAUSARZT PRAXIS 2014; 9(3): 36-37