Magnetic resonance imaging is a sensitive method for visualizing reversible and irreversible changes in brain tissue after epileptic seizures. The following case report specifically discusses diffusion imaging, which can visualize periiictal brain parenchymal changes very early after an epileptic seizure.
Case report: a 74-year-old female patient was found unconscious at home. The duration of unconsciousness could not be determined. The patient suffered from depressive episodes, alcohol dependence, and untreated arterial hypertension. In the emergency department, the patient suffered a generalized tonic-clonic epileptic seizure. She was not responsive at any time. Neurological examination revealed plegia of the left side of the body, and the limbs of the right side of the body were moved only in response to severe pain stimuli. In addition, there was a gaze deviation to the upper left. CSF examinations were unremarkable. CT, MRI, and EEG examinations were performed.
Imaging: MRI showed extensive cortical diffusion restrictions right hemispherically (Fig. 1). In addition, contralaterally, less pronounced diffusion restrictions existed confined to the cerebellar hemisphere(Fig. 2). T2-weighted imaging showed signal enhancement as well as cortical swelling in areas of disturbed diffusion(Fig. 1).

Fig. 1: (a) Right hemispheric cortical DWI signal enhancement; b) ADC lowering in the sense of cytotoxic edema.
Correspondingly, a signal enhancement and distension of the cortex is found in T2w (c).
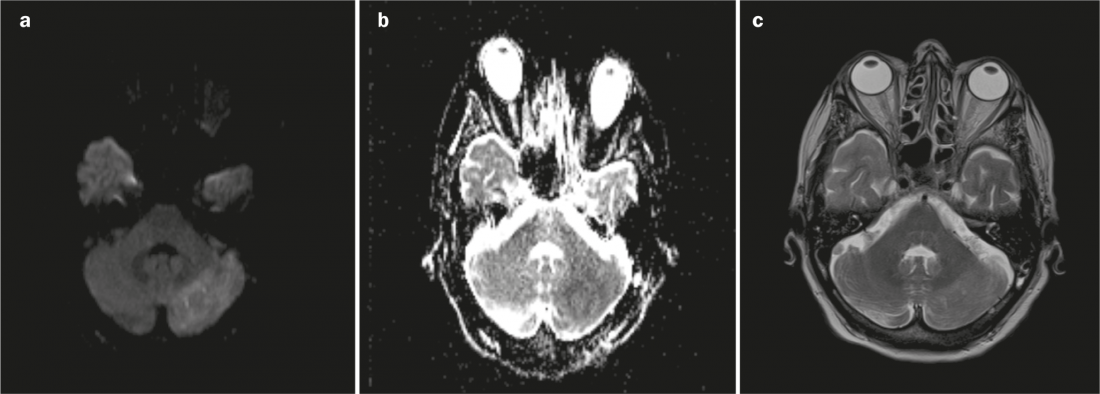
Fig. 2: Contralateral to the right hemispheric changes there are (a) DWI signal increases with (b) lowered ADC value as well as (c) T2w signal elevations of the left cerebellar hemisphere in the setting of crossed cerebro-cerebellar diaschisis.
Discussion: Periiictal changes were observed in the early days of computed tomographic imaging. With the increased availability of MRI, a whole spectrum of periiictal changes has been described over time. Generally, signaling alterations are found at the site of neuronal activity confined to the cortex [1]. These signaling alterations are the result of increased metabolism of neurons during an epileptic seizure. This initially results in increased blood flow due to the increased neuronal activity. At this stage, only increased perfusion can be detected; no morphologic changes are yet found. With persistence of the epileptic seizure, vasogenic edema occurs and leads to dilation of the extracellular space. This results in an overall increase in molecular diffusion, which is reflected in an increased ADC (“Apparent Diffusion Coefficient”) value (hyperintense in the so-called ADC map). If the seizure continues, the persistent depolarization of the neurons leads to an uncontrolled influx of Ca++ ions into the cells, with consecutive intracellular edema. This type of edema is also called cytotoxic edema because of the associated cellular damage. Compared to extracellular water, intracellular water is compartmentalized by numerous membranes, which leads to a restriction of molecular motion and thus a decrease in ADC value [1]. However, even real diffusion restriction (signal enhancement in DWI with lowered ADC) is often partially reversible after an epileptic seizure.
In some cases, periiictal diffusion defects may also occur at sites distant from the epileptogenic area. Thus, the term diaschisis describes dysfunction in a spatially separate brain region from the cortical or subcortical lesion. Crossed cerebro-cerebellar diaschisis represents damage caused by sustained excess excitatory activity along the cortico-pontine-cerebellar pathways and/or the lack of inhibition of these pathways by controlling inhibitory interneurons [2].
Our case shows epilepsy-type diffusion restrictions of the right cerebral and left cerebellar hemispheres restricted to the cortex. This characteristic distribution as well as the clinical symptoms of the patient allow the conclusion that status epilepticus with crossed cerebro-cerebellar diaschisis has occurred.
Unfortunately, despite expansion of anticonvulsant therapy, it was not possible to break through a renewed focal status epilepticus with two right hemispheric foci. The patient therefore died 48 h after admission to the hospital.
Tilman Schubert, MD
Michele Pansini, MD
Prof. Dr. med. Stephan Wetzel
PD Stephan Rüegg, M.D.
Arne Fischmann, MD
Literature:
- Yu JT, Tan L: Diffusion-weighted magnetic resonance imaging demonstrates parenchymal pathophysiological changes in epilepsy. Brain research reviews 2008 Nov; 59(1): 34-41.
- Cole AJ: Status epilepticus and periictal imaging. Epilepsia 2004; 45(4): 72-77.