Meningiomas of the skull base can lead to different symptoms depending on their location and size. The surgical procedure is very challenging due to the proximity to the caudal cranial nerves. The interdisciplinary treatment of inferior clivus foramen magnum meningioma is presented below.
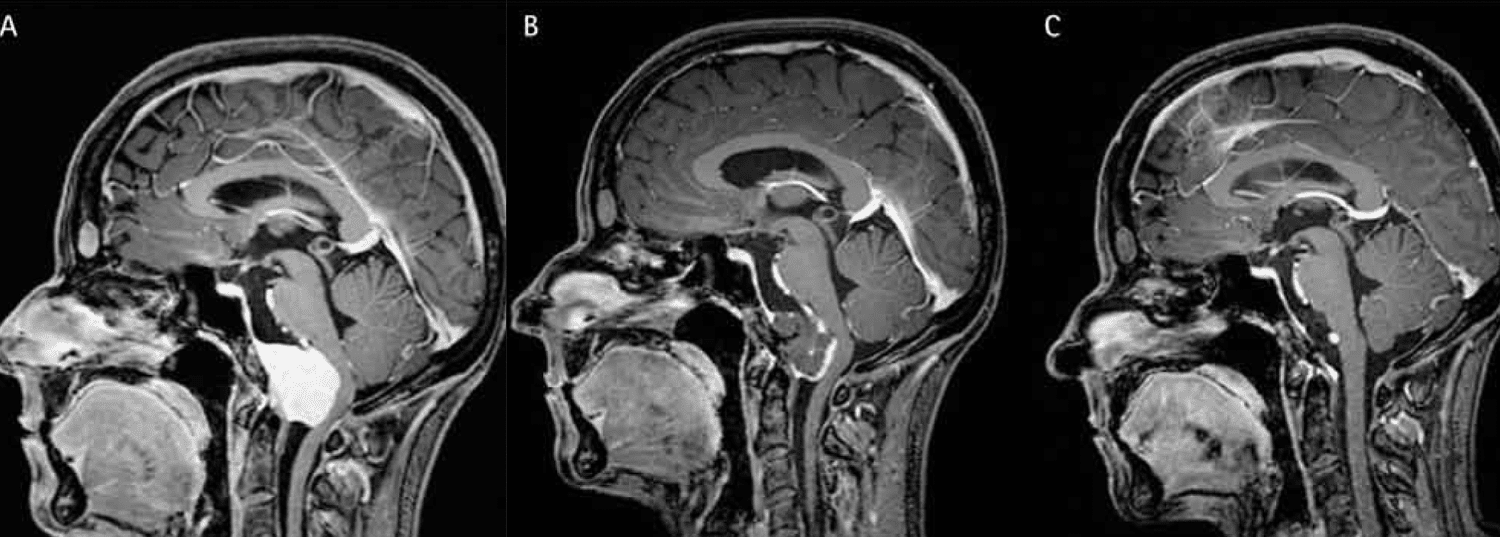
Case Report: The 39-year-old female patient observed slowly increasing gait unsteadiness and painful neck muscle tension. When a cervical disc herniation was suspected, an MRI of the cervical spine was first obtained. However, these images did not show a spinal stenosis as expected, but a meningioma at the ventral foramen magnum (Fig. 1). Neurologically, symptoms of discrete spinal ataxia and right hypoglossal nerve palsy with unilateral tongue atrophy were noted.
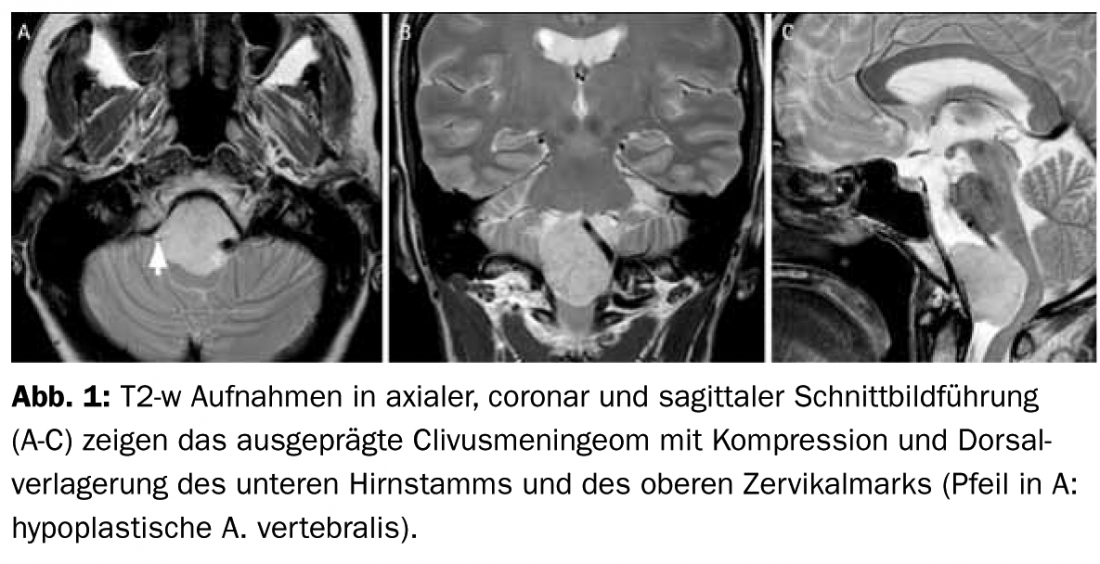
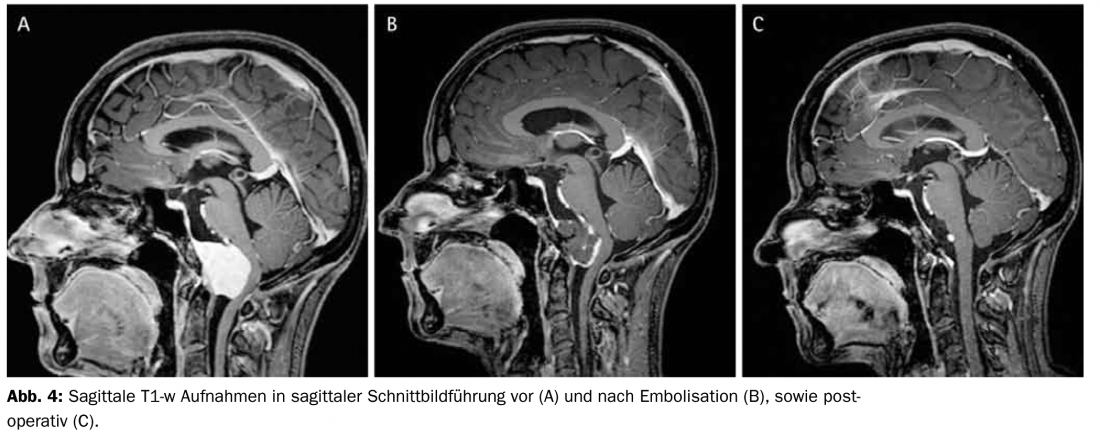
Catheter angiography confirmed the pronounced hypervascularization of the tumor already suspected by MRI. Under local anesthesia, embolization of the tumor was performed via the ascending pharyngeal artery on both sides (densarcade) and a meningeal branch of the right vertebral artery. A liquid embolisate (Onyx= precipitating copolymer dissolved in DMSO) was used for this purpose. This resulted in angiographic near-complete devascularization of the tumor, which was also evident on MRI performed immediately before surgery (Figs. 2, 3B, 4).
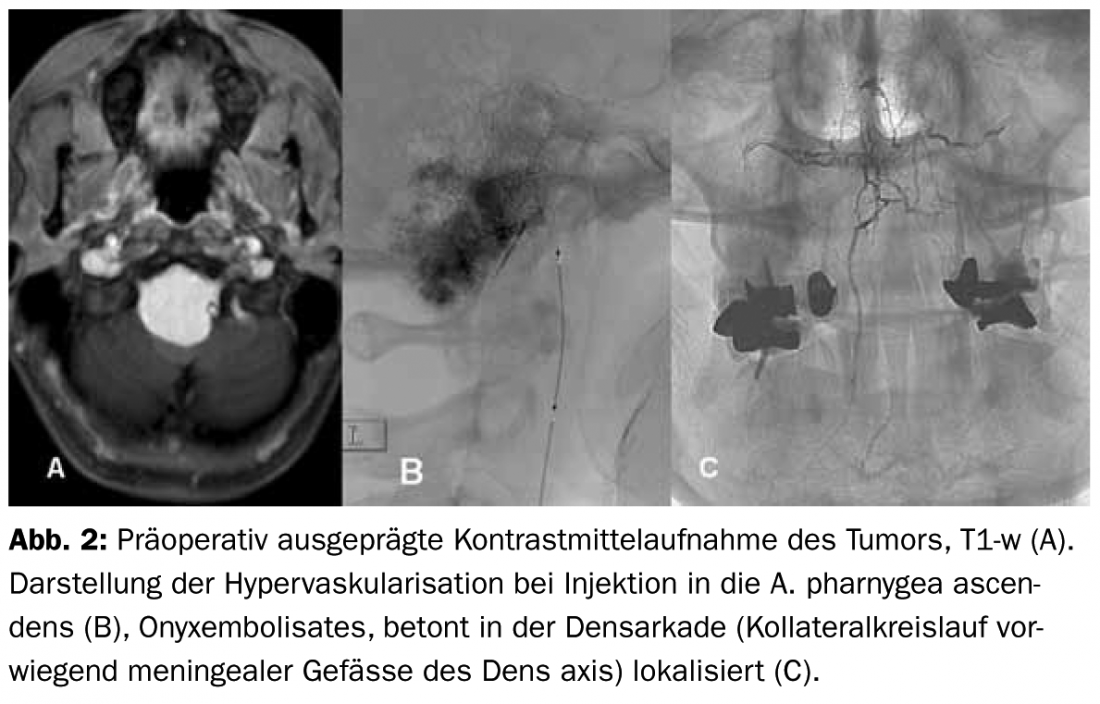
Five days after embolization, surgical resection was performed (Fig. 3).
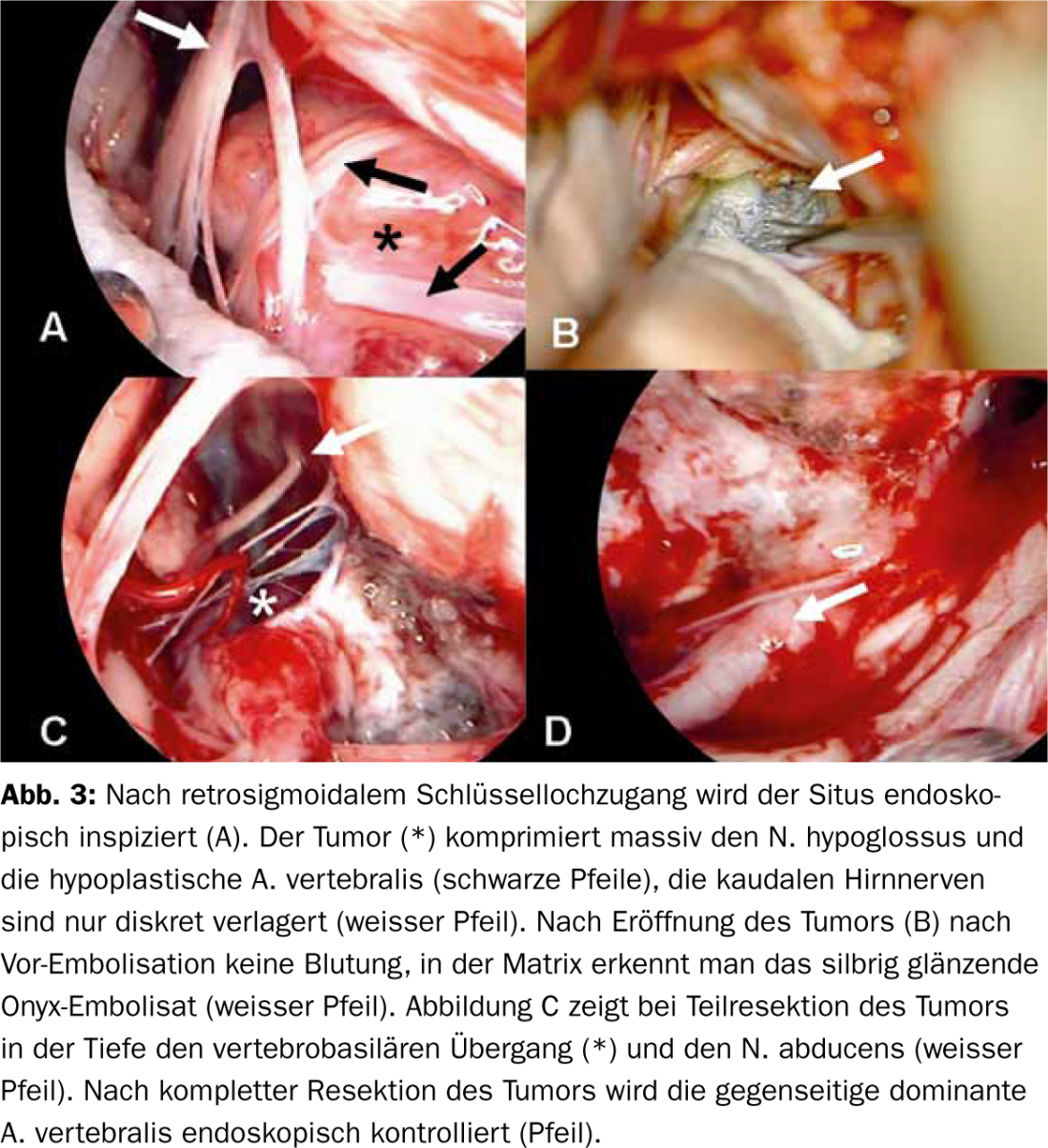
An intraoperative CT was obtained in lateral recumbency and the integrated navigation system was registered. The caudal clivus and ventral foramen magnum were visualized via a retrosigmoidal mini-craniotomy. Due to the optimally placed keyhole access, no brain retraction had to be applied during the entire operation. Steps of microsurgical tumor resection were monitored endoscopically. Because of preoperative embolization, the devascularized and already partially necrotic tumor could be gradually exposed without bleeding and without injuring the eloquent surrounding structures. Intraoperative electrophysiology with SSEP/MEP measurement and monitoring of the caudal cranial nerves showed no pathological changes. Intraoperative CT was performed immediately postoperatively for resection control.
The primary postoperative course was regular, with hoarseness and dysphagia showing rapid and complete regression; imaging showed only a tiny tumor remnant on MRI. Tongue atrophy was no longer detectable after six months.
Discussion: This case illustrates the value of interdisciplinary collaboration in complex tumors of the skull base using modern techniques.
The almost complete devascularization of the tumor facilitated the subsequent resection. Embolization with liquid embolisate (Onyx) allows gradual elimination of the tumor umbilical vessel and is performed to simultaneously achieve occlusion of the tumor main vessels and their collateral supply and induce subsequent tumor necrosis. The choice of endovascular access route is critical to avoid potential compromise of the arterial cranial nerve supply. The endoscopically as well as computed tomographically controlled resection allowed an optimal visual, the intraoperative neuromonitoring a safe functional control of the resection in terms of minimally invasive and maximally effective surgical therapy.
Literature:
- Teo C. Endoscopic-assisted tumor and neurovascular procedures. Clin Neurosurg 2000;46:515-25.
- Shie et al. Therapeutic embolization of meningiomas with Onyx for delayed surgical resection. Surg Neurol 2008; 70:478-81
InFo NEUROLOGY & PSYCHIATRY 2013; 11(1): 24-25.