Endometrial cancer is the sixth most common cancer in women worldwide and has a poor prognosis, particularly in terms of long-term results. The median overall survival time is less than three years. Effective therapy management is particularly indicated for patients with primary advanced or recurrent endometrial cancer. Now study results are raising hopes for a new combination treatment.
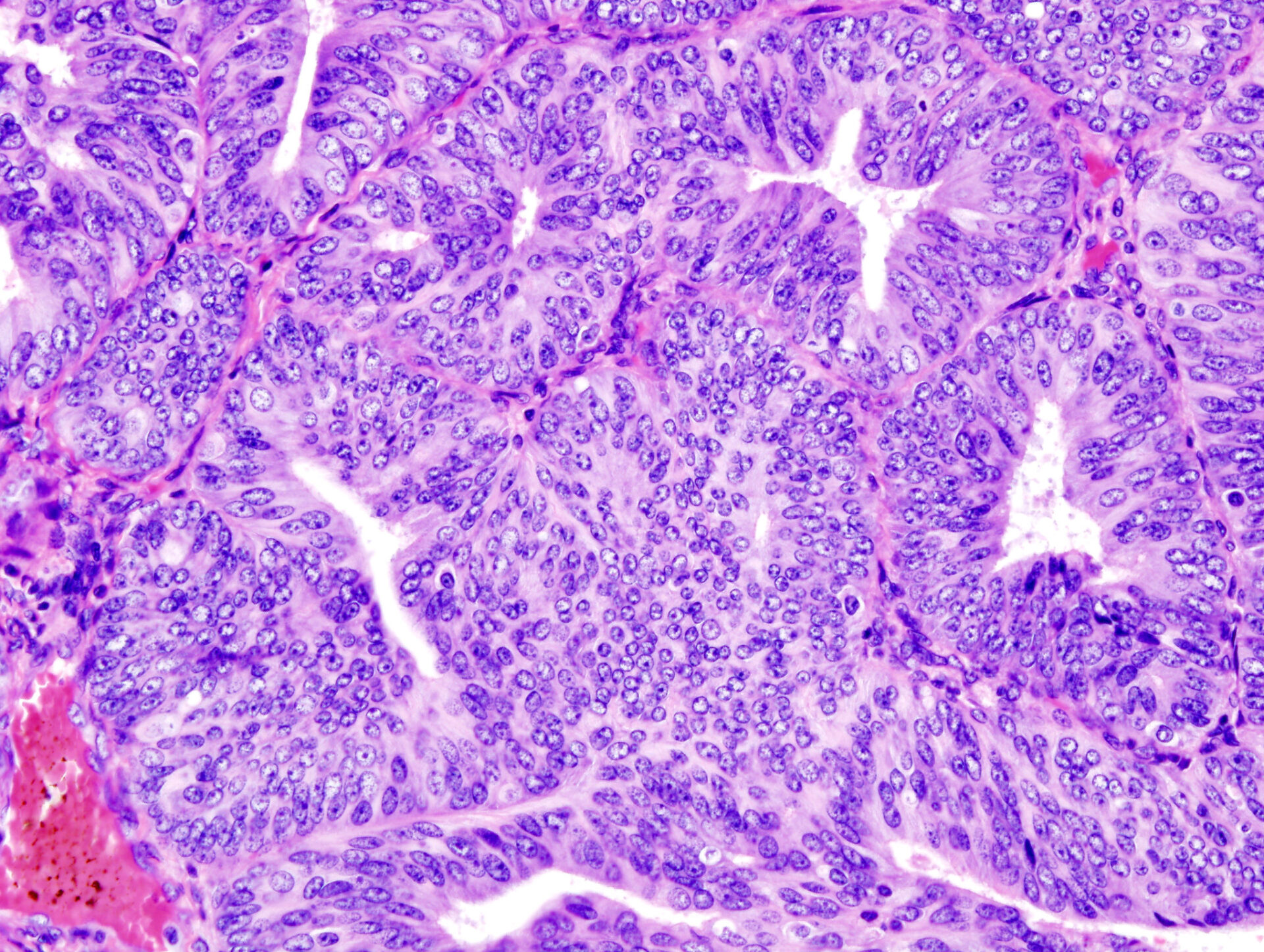
Endometrial carcinoma (EC) is a malignant tumor of the uterus originating from the inner mucosal layer of the uterus. The disease predominantly affects post-menopausal women, with a peak age between 65 and 85 years. Early menarche, late menopause, low parity or polycystic ovary syndrome are described as endogenous risk factors. Exogenous risk factors include non-cyclic oestrogen replacement therapy alone, tamoxifen therapy and previous radiotherapy. EC usually involves adenocarcinomas of the uterine lining. Serous and clear cell adenocarcinomas or squamous cell carcinomas occur only rarely. A distinction is made between oestrogen-dependent type I carcinoma and oestrogen-independent type II carcinoma. However, immunohistochemical and molecular markers are also playing an increasingly important role.
Molecular typing enables more precise therapy
Molecular subtyping enables individualized risk stratification and a more precise choice of therapy. As part of The Cancer Genome Atlas (TCGA) project, four molecular subtypes of EC were identified using next generation sequencing (NGS):
- POLE: mutated polymerase epsilon (POLE) gene, impaired proofreading function during DNA replication, ultramutated phenotype
- MSI-H/dMMR: deficient mismatch repair (dMMR) due to mutations, high microsatellite instability (MSI-H), hypermutated phenotype
- Copy number high/TP53abn: high number of somatic copy number alterations, mostly TP53 mutations (TP53 abnormal)
- Copy Number low/NSMP: various mutations, no specific molecular profile (NSMP)
Building on this basis, targeted substances (e.g. Dostarlimab, Lenvatinib) have been developed in recent years. MSI-H tumors account for 25-30% of endometrial cancers. The increased expression of programmed cell death receptor 1 (PD-1) and its ligands (PD-L1 and PD-L2) and the high tumor mutational burden associated with dMMR-MSI-H tumors make them potentially susceptible to anti-PD-1 and anti-PD-L1 therapies.
Primary advanced or recurrent EC
Carboplatin plus paclitaxel is the standard chemotherapy for the first-line treatment of primary advanced or recurrent EC. However, the long-term results are still not satisfactory. Before the targeted agents were approved, there were no effective treatment strategies for patients who had failed platinum-based chemotherapy. Dostarlimab is an active immune checkpoint inhibitor that targets the PD-1 receptor. Based on the results of the GARNET study, the drug was approved for dMMR-MSI-H advanced or recurrent endometrial cancer. The researchers have now gone one step further: cytotoxic chemotherapy can have immunomodulatory effects, such as the interruption of immunosuppressive signaling pathways and an enhanced cytotoxic T-cell response. It was therefore reasonable to assume that the combination of chemotherapy and immunotherapy could have a synergistic effect in the tumor microenvironment. The ENGOT-EN-6-NSGO/GOG-3031/RUBY study therefore investigated the efficacy and safety of dostarlimab in combination with carboplatin and paclitaxel compared to placebo plus carboplatin and paclitaxel in patients with primary advanced or recurrent EC.
In the double-blind, multicenter Phase III study, 494 patients (118 of whom had dMMR-MSI-H-EC) were randomized in a 1:1 and received either 500 mg dostarlimab or placebo intravenously in combination with carboplatin and paclitaxel every three weeks for the first six cycles, followed by 1000 mg dostarlimab or placebo intravenously every six weeks for up to three years or until disease progression, discontinuation of treatment due to toxic effects, patient withdrawal, investigator’s decision to withdraw the patient, or death. The primary endpoints were progression-free survival in patients with primary advanced or recurrent dMMR-MSI-H-EC and in the overall population, as well as overall survival in the overall population. Secondary endpoints included progression-free survival determined by a blinded, independent central review, objective response, disease control, duration of response, time to second disease progression, patient-reported outcomes, and pharmacokinetic and immunogenicity analyses.
Prolonged progression-free survival
The overall survival rate after 24 months was 71.3% with dostarlimab and 56.0% with placebo. In the dMMR-MSI-H population, the estimated progression-free survival was 61.4% in the serum group and 15.7% in the placebo group. In the total population, it was 36.1% vs. 18.1%. The most common adverse events were nausea (53.9% versus 45.9%), alopecia (53.5% and 50.0%) and fatigue (51.9% and 54.5%). Patients with primary advanced or recurrent EC were found to benefit significantly from the combination of dostarlimab, carboplatin and paclitaxel in terms of a lower risk of disease progression.
Further reading:
- Mirza MR, Chase DM, Slomovitz BM, et al.: Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer. N Engl J Med 2023; 388: 2145–2158.
- www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/LL_Endometriumkarzinom_Langversion_3.01_.pdf (last accessed am 05.01.2024)
- www.gelbe-liste.de/krankheiten/endometriumkarzinom (last accessed on 05.01.2024)
- www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/krebsarten/andere-krebsarten/gebaermutterkoerperkrebs.html (last accessed on 05.01.2024).
HAUSARZT PRAXIS 2024; 19(1): 41
InFo ONKOLOGIE & HÄMATOLOGIE 2024; 12(1): 26
Cover picture: Histopathologic representation of endometrioid adenocarcinoma demonstrated in endometrial biopsy. Hematoxylin-eosin stain.
© KGH, wikimedia