Urothelial carcinomas can occur in the upper or lower urinary tract. To examine the draining urinary tract (renal pelvic calices, ureters), computed tomography (CT) and magnetic resonance imaging (MRI) are among the methods used. CT is the most commonly used imaging technique in the diagnosis of tumors of the urinary system and nowadays offers the possibility of intravenous contrast agent applications and late imaging in addition to the thin-slice technique.
Upper urinary tract urothelial carcinomas were reported in the previous article. This type of tumor is incomparably more frequent in the lower urinary tract, especially in the urinary bladder. Numerous histologic subtypes exist [6]. The distribution pattern correlates to urothelial surface area. More than 90% of transitional cell carcinomas are found in the urinary bladder. At 95%, this tumor entity also accounts for the majority of bladder carcinomas overall. Only 5% correspond to adenocarcinoma and squamous cell carcinoma [1,4].
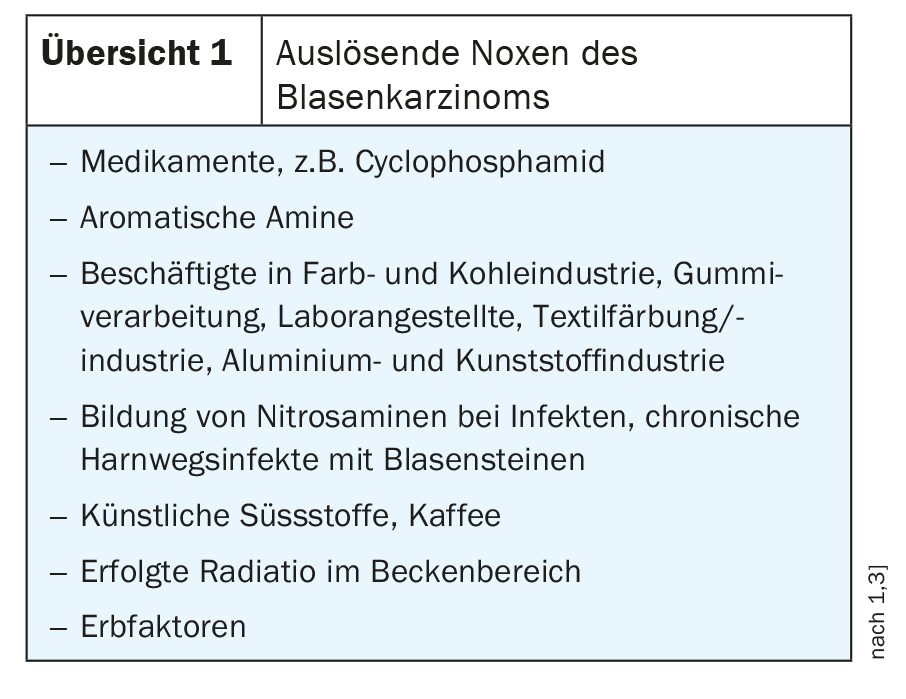
In Germany, about 30,000 new cases of bladder cancer are reported annually, the male:female ratio is about 3:1, and the relative risk of smokers to nonsmokers is 2:1 to 6:1. Rare tumor diseases in children have been described [5]. 30-40% of bladder cancers are thought to originate from cigarette use. Other triggering noxae are listed in overview 1 .
The symptomatology of bladder carcinomas is relatively nonspecific with painless micro- or macrohematuria, also irritable bladder symptomatology with frequent urination and dysuria. Pain in the bladder and bowel region may indicate an advanced stage. In cases of clinical suspicion of urothelial carcinoma, urine cytology has a high sensitivity in the diagnosis of aggressive carcinomas, but does not allow any conclusion on the localization in the urinary tract. Bladder tumor antigens can be determined.
Urethrocystoscopy can be used to confirm the diagnosis of the bladder tumor, including the location in the urinary bladder, as well as the size and number of tumors. Photodynamic diagnostics (PDD) supports better detection of urothelial carcinoma. In non-muscle-invasive carcinoma (Ta, T1, Tis), tumor ablation can be performed by transurethral resection of the urinary bladder (TURB), supplemented by intravesical early instillation therapy with mitomycin C. Radical cystectomy is the method of choice for tumor recurrence of high-grade urothelial carcinoma. Favorable condition for radiotherapy is the preceding complete TURB.
X-ray examinations with excretory urography (AUR) and sonography are of secondary importance in the diagnosis of tumors of the upper urinary tract, especially in the surrounding diagnosis. Sonography of the urinary bladder is a rarely requested examination in our practice, usually it is already done by the family doctor or urologist. When the urinary bladder is full and the bladder wall is highly echo-rich, the tumors present less echogenically, sometimes delineated by wall alteration. The false-negative rate is reported to be 40%, and the false-positive rate is 10% [4].
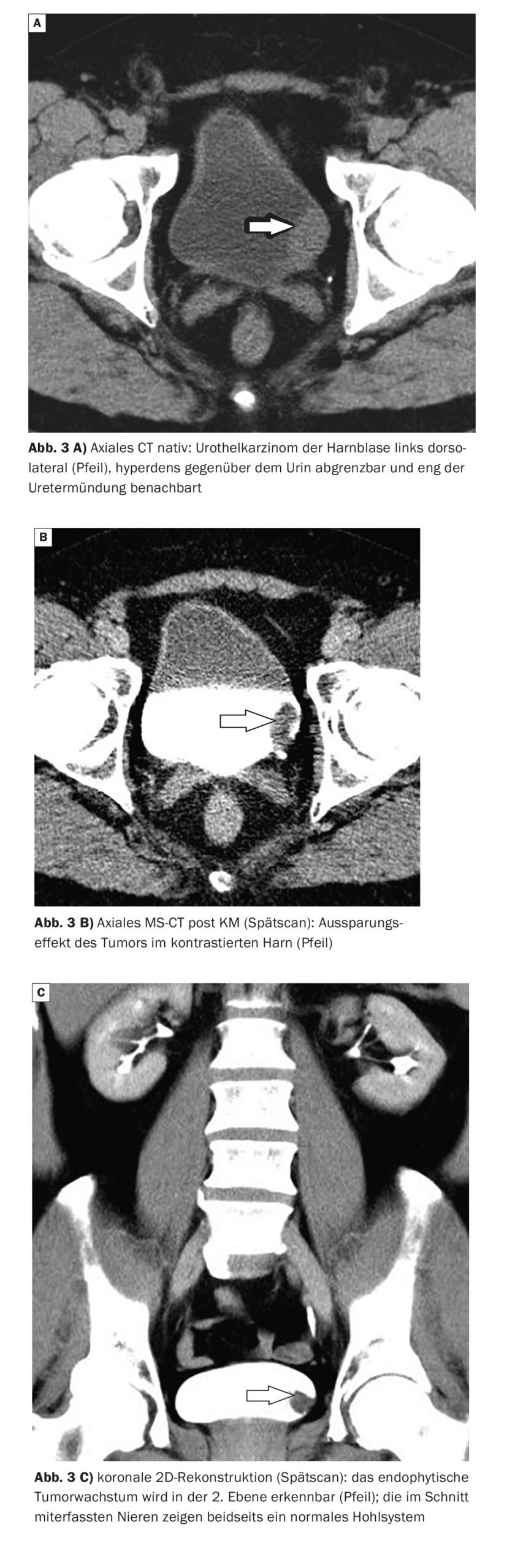
In addition to direct visualization of bladder tumors, computed tom ography also offers the possibility of clarifying lymphogenic and hematogenic metastases and the detection of resulting functional disorders in urinary retention due to stenosis or obstruction of the ureteral orifice in the urinary bladder. It is by far the most common imaging examination in the diagnosis of tumors of the urinary system. The thin-layer technique, intravenous contrast agent application, and late imaging have been shown to be effective [7].
MRI has a high detection rate of bladder tumors. The urothelial carcinomas show a dominant localization on the lateral and dorsal bladder wall [2], often near the ureteral orifice. Multicentric occurrence and high recurrence rate after TUR are characteristic and can be confirmed by MRI. Intravenous contrast agent application improves the tumor detection rate.
Case studies
In case report 1 (Fig. 1A and 1B), tumor recurrence of urothelial carcinoma of the posterior wall of the urinary bladder in the orifice of the right ureter is seen on CT. 3 years earlier, the now 70-year-old patient had undergone TURB followed by mitomycin treatment. The recurrent tumor resulted in significant outflow obstruction, the right ureter was markedly dilated, and perfusion of the kidney was restricted. The man experienced an increasing feeling of pressure with progressive pain symptoms in the area of the right flank; microhematuria was confirmed by laboratory chemistry.
Case 2 (Fig. 2) shows a multicentric finding of urothelial carcinoma of the urinary bladder with dorsal and dorsolateral space-occupying lesions in close proximity to the ureteral orifice. The 29-year-old patient had recurrent macrohematuria.
Case report 3 (Figs. 3A to 3C) demonstrated computed tomographic evidence of a tumor of the left urinary bladder on “stone CT” for suspected urolithiasis with recurrent microhematuria. The examination was enhanced with contrast scans, and the tumor findings in the 63-year-old patient were confirmed.
Take-Home Messages
- The main site of urothelial carcinoma is the urinary bladder.
- Men are more frequently affected than women, and multicentric tumor growth occurs.
- Symptomatology is nonspecific with hematuria; pain may be present in advanced tumor stages.
- The most important imaging examination procedure in
Urothelial carcinoma is computed tomography.
Literature:
- ElSharnoby O, et al.: Bladder urothelial cell carcinoma as a ra-re cause of haematuria in children: Our experience and review of current literature. J Pediatr Surg 2022; 57(7): 1409–1413.
- Hamm B, et al.: (Hrsg.): MRT von Abdomen und Becken. 2., völlig überarbeitete und erweiterte Auflage. Georg Thieme Verlag Stuttgart, New York 2007; 222–227.
- Comprehensive Cancer Center Ulm, www.uniklinik-ulm.de/
comprehensive-cancer-center-ulm-cccu.html, (letzter Abruf 26.06.2023) - Manski D. Harnblasenkarzinom: Symptome, Diagnose und Staging: https://urologielehrbuch.de/harnblasenkarzinom_03.html, (last accessed 26.06.2023)
- Samaratunga H, Delahunt B: Recently described and unusual variants of urothelial carcinoma of the urinary bladder. Pathology 2012; 44(5): 407–418.
- Xu N, et al.: Integrated proteogenomic characterization of urothelial carcinoma of the bladder. J Hematol Oncol 2022; 15(1): 76.
- Yu EM, Belay S, Li W, Aragon-Ching JB: Non urothelial and urothelial variants of bladder cancer. Cancer Treat Res Commun 2022; 33: 100661.
HAUSARZT PRAXIS 2023; 18(8): 42–44
InFo ONKOLOGIE & HÄMATOLOGIE 2023; 11(4): 32–34