At the EMUC Congress in Lisbon, two sessions highlighted diagnostic and therapeutic strategies in prostate cancer. One was the benefits and effects of Active Surveillance, and the other was a comparison of intermittent versus continuous androgen deprivation. A “pros and cons” session discussed whether the principle of “the fewer drugs, the better” also applies here.
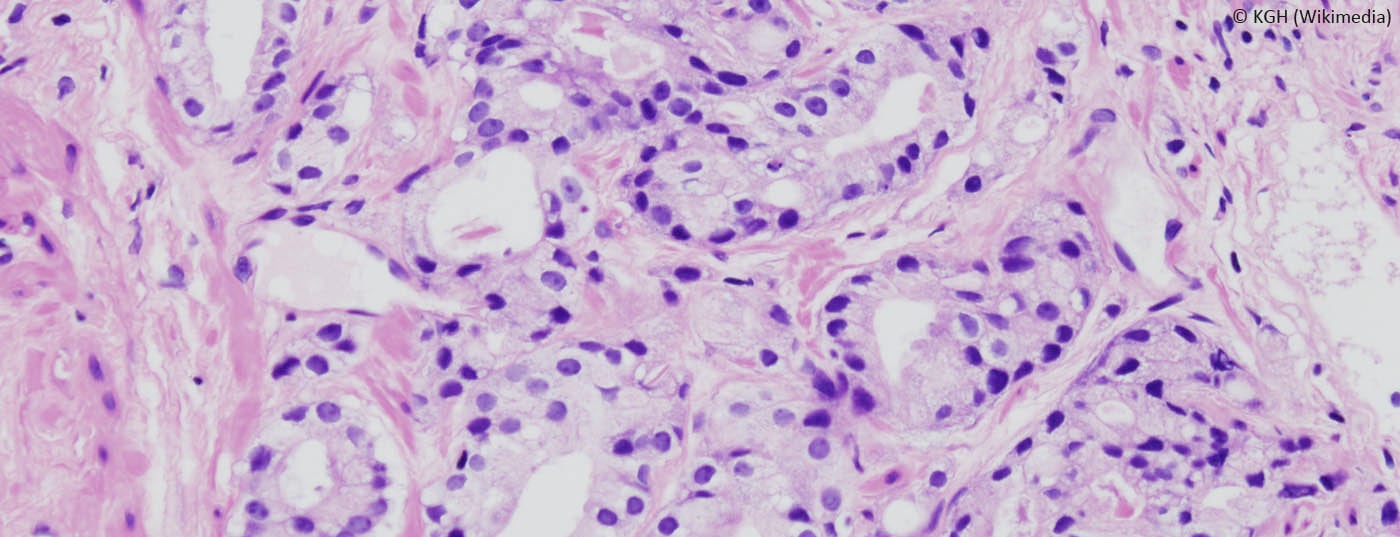
(ag) Prof. Monique Roobol, MD, Rotterdam, referred to the two faces of prostate cancer: on the one hand, the disease can be indolent, slow and rather harmless; on the other hand, it can be very aggressive, painful and fatal. Especially the indolent form is common in elderly patients. Although the PSA test is not specific for (aggressive) prostate cancer, men with values outside the norm are often subjected to further diagnostic tests, which in turn can lead to overtreatment. However, the natural history of the disease presents a continuum of risk that should be surveyed carefully and judiciously. According to epidemiological calculations, overdiagnosis is present in 22-42% of cases.
Active surveillance (AS) cannot prevent overdiagnosis, but it can reduce the associated harm (especially overtreatment). “You have to separate diagnosis more strictly from treatment, which means you need precise definitions of when it becomes dangerous and therefore necessary to intervene.” AS is thus a temporary but indispensable solution to address problems of overdiagnosis and overtreatment. Of course, because AS protocols rely on repeated transrectal prostate biopsies, they are not without risks.
Which examinations are part of the AS?
Studies are currently examining various potential tools for AS. Findings from genetics and various potential biomarkers are discussed. For example, one wonders about the predictive value of age, ethnicity, or family history, or whether genetic variables (T2-ERG, PCA3, etc.) play a significant role. This shows that only biopsy and PSA derivatives continue to consistently predict progression risk. “Even imaging tools such as MRI/ultrasound cannot yet replace repeated prostate biopsy,” she said.
Safety of the AS difficult to define
It would also be interesting to know to what extent AS specifically affects quality of life. However, previous data on this are not randomized and often exhibit selection bias. They show comparable levels of quality of life as after radical therapy. Prof. Robool emphasized the importance of collecting prospective long-term data on AS. “Considering the natural long course of early-stage prostate cancer, mid-term outcomes of AS become even more important. So it’s not enough to just collect mortality as a safety outcome of AS.” Predictive models could be used to predict which patients are psychosocially vulnerable to AS (with stress, anxiety, and depression). Ultimately, however, the survey of quality of life as an important outcome of AS needs to be better standardized.
Specific evidence-based guidelines on AS are also urgently needed.
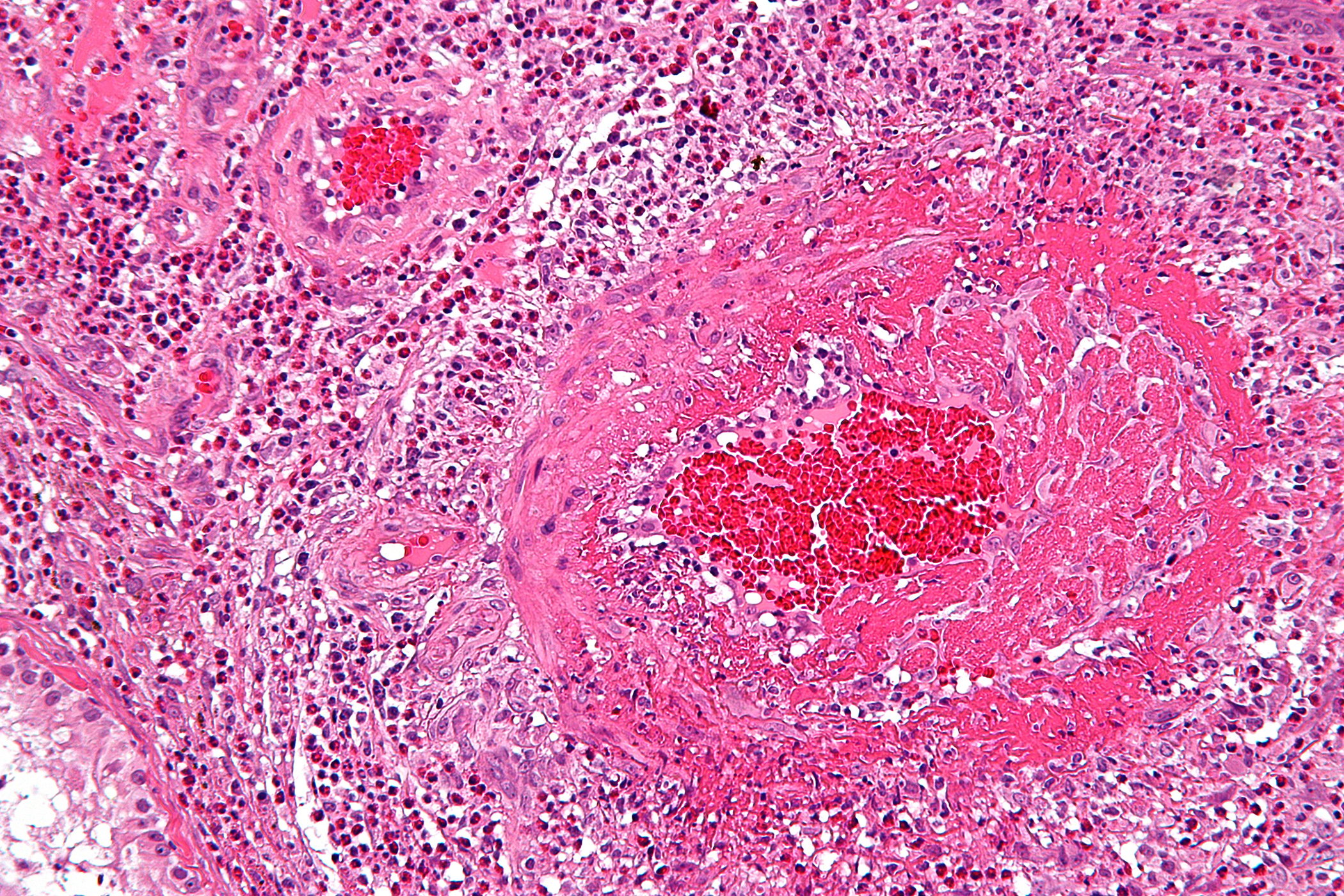
Therapy: intermittent or continuous androgen deprivation?
The question of whether continuous (CAD) or intermittent androgen deprivation (IAD) shows better results was also discussed at the congress. Maha Hussain, MD, Michigan, reviewed the study situation: “Many phase III studies comparing IAD with CAD unfortunately have relevant limitations: Patient populations are often highly mixed and samples are relatively small. Treatment schedules differ and endpoints (e.g., time to progression) are not uniformly defined. In addition, most papers have too short a follow-up.” Hussain concluded that IAD has not yet shown superiority in terms of overall survival in any randomized trial. The non-inferiority – if it was defined statistically at all – could either not be proven at all or, according to the speaker, only with too high HR limits: While SWOG9346 [1] exceeded the defined HR threshold of 1.2, NCIC PR7 [2] found non-inferiority, but only with a higher threshold of 1.25 (which, according to the speaker, should be questioned). Indeed, in concrete terms, this would mean that a 25% increase in mortality risk from using IAD instead of CAD is still tolerable. Results are also mixed and inconsistent in the “time to progression” endpoint. “Since the benefits in terms of quality of life are also not very convincing, you really have to wonder what the relevance of the intermittent option is in the first place,” she explained.
Overall, the role of CAD in the adjuvant setting is undisputed, he said. With androgen deprivation and local therapy, the survival of these patients can be decisively prolonged.
In patients with non-metastatic PSA recurrence, neither approach has shown significant benefit to date (although IAD is discussed as an option).
“For metastases, on the other hand, CAD seems to tend to offer a survival advantage. If one still applies IAD because of the slightly better quality of life, then only after fully informing the patient and taking into account the worse survival outcome,” Hussain said.
All a matter of interpretation?
This critical view was contradicted by Prof. Per-Anders Abrahamsson, MD, Lund. In his opinion, the existing data must be interpreted in exactly the opposite way, namely positively: for some selected patients, IAD represents an equivalent alternative to CAD. “Reviewing the literature referred to by the previous speaker, one finds no clear evidence for superiority or inferiority of IAD compared with CAD (applies to survival [1–3] and time to progression [4,5]). Although the equivalence of the variants has not yet been sufficiently proven statistically, it seems plausible in view of the data available to date, at least in selected patients,” said Prof. Abrahamsson. “IAD will never be a therapy that can be considered in all patients, certainly not those with high tumor burden. This is one of the reasons why the highly mixed populations of many studies are problematic.” However, the intermittent variant is better tolerated and possibly – although studies would have to show this first – it prevents certain long-term complications of AD [6]. European guidelines (EAU) also newly point out that the status of IAD can no longer be considered purely investigative. Both speakers agreed that research efforts must be intensified if more concrete conclusions are to be drawn.
Source:6th European Multidisciplinary Meeting on Urological Cancers, November 13-16, 2014, Lisbon.
Literature:
- Hussain M, et al: Intermittent versus continuous androgen deprivation in prostate cancer. N Engl J Med 2013; 368: 1314-1325.
- Crook JM, et al: Intermittent androgen suppression for rising PSA levels after radiotherapy. N Engl J Med Sep 6 2012; 367(10): 895-903.
- Mottet N, et al: Intermittent hormonal therapy in the treatment of metastatic prostate cancer: a randomized trial. BJU Int 2012 Nov; 110(9): 1262-1269.
- Calais da Silva FE, et al: Intermittent androgen deprivation for locally advanced and metastatic prostate cancer: results from a randomised phase 3 study of the South European Uroncological Group. Eur Urol 2009 Jun; 55(6): 1269-1277.
- Salonen AJ, et al: The FinnProstate Study VII: intermittent versus continuous androgen deprivation in patients with advanced prostate cancer. J Urol 2012 Jun; 187(6): 2074-2081.
- Sciarra A, et al: Intermittent androgen-deprivation therapy in prostate cancer: A critical review focused on phase 3 trials. European Urology 2013; 64(1): 722-730.
InFo ONCOLOGY & HEMATOLOGY 2014; 2(10): 22-23.