When a patient reacts to the administration of a drug, the question for the treating physician is always whether it is an allergy or a non-specific reaction. Ultimately, this will determine the further course of treatment. An expert gave recommendations on how to proceed in certain situations.
When anaphylaxis occurs, one usually first thinks of an IgE-mediated allergy, mediated by mast cells or basophilic granulocytes. In addition, however, there are a variety of causes that cause anaphylaxis that are not due to allergy (box). The underlying mechanism of anaphylaxis is essential for the affected patient in terms of which substances and agents he or she can still use in the future. Not all substances are affected to the same extent by non-specific reactions, so-called “pseudoallergies”. Both allergic and non-allergic mast cell activation may be caused by aspirin and NSAIDs, opiates, antibiotics (vancomycin, quinolones), X-ray contrast media, muscle relaxants, narcotics and local anesthetics, but also plasma expanders, biologics, iron preparations and chemotherapeutic agents.
On the basis of three case studies, Dr. Lukas Jörg, Head of the Polyclinic for Allergology and Clinical Immunology, University Clinic for Pneumology and Allergology, Inselspital Bern, explained the diagnostics and therapeutic options for getting anaphylactic reactions under control [1].
Case 1: NSAID/Aspirin
A 38-year-old woman who had not taken pain medication for some time resorted to 400 mg of ibuprofen due to headache. After about 40 minutes, she initially developed mild rhinitis, followed by dyspnea and urticarial skin lesions mainly on the trunk and arm area. The medical history showed that the reaction occurred for the first time in the patient. She also suffered from mild asthma, which was treated with budesonide/formoterol.
For allergological clarification, Dr. Jörg uses skin tests (prick, intradermal and epicutaneous tests), in selected situations also in vitro tests (specific IgE, basophil activation test, lymphocyte transformation test). “However, one should keep in mind that a skin test, for example, can be used to detect an allergy, but not a nonspecific reaction to another substance,” the expert cautioned. “So often – especially with immediate type reactions – it boils down to provocation testing, exposing the patient to either the trigger or an alternative.”
Provocation testing was also used in the young patient’s case after a skin test was negative. The allergist’s goal was to find out if the use of other anti-inflammatory drugs was possible in the young woman. Dr. Jörg therefore performed the provocation test with aspirin, and inhaled due to the dyspnea.
At a dose of 10 mg or more, FEV1 dropped and the patient became increasingly obstructive. A drop in FEV1 to below 80% can be considered an indicator of a positive test result, according to the physician. “In this case, therefore, we must assume that the woman has an intolerance to anti-inflammatory drugs and not an allergy.” If she were allergic, the patient would simply have to avoid ibuprofen and the corresponding group. However, since she has now also reacted to a substance with aspirin, which has a different structure but the same mechanism of action, all anti-inflammatory drugs must be dispensed with in her case, Dr. Jörg explained.
With regard to the procedure, the allergist emphasized the importance of a thorough anamnesis; in particular, any underlying diseases should be inquired about. “Patients who have asthma or rhinosinusitis with nasal polyposis in particular are at increased risk of reacting to NSAIDs or aspirin.” The same is true for those with urticaria or angioedema. However, Dr. Jörg advises a skin test only if there is a clear suspicion of an allergy, such as when a patient reacts to diclofenac but states that he or she can tolerate ibuprofen.
For the future, he recommended that the 38-year-old avoid the Cox1 inhibitor group. Alternatives are paracetamol or opiates. After prior provocation testing, selective Cox2 inhibitors and metamizole are also possible.
| Non-IgE-mediated activation pathways of anaphylaxis. |
| – IgG – Complement – Bradykinin – Leukotrines – Prostaglandin E2 |
Effector cells – Neutrophils – Endothelial cells – Smooth Muscle – Mast cells – Basophile – Eosinophils |
Case 2: Iron infusions
A 50-year-old female patient suffered from iron deficiency. She should receive iron infusions of 200 mg iron sucrose over 20 minutes. After 15 minutes, the patient developed significant flushing, itching, a strong sensation of heat, and considerable discomfort. Since the woman would continue to require iron infusions in the future (initial peroral substitution had not worked), the question arose as to how she could continue to be treated.
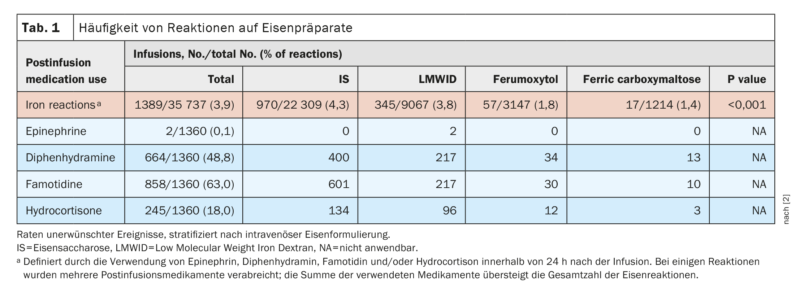
Reactions after iron preparations are in the low single-digit percentage range (Tab. 1) . As a rule, these are also non-allergic reactions. The exception is Low Molecular Weight Iron Dextran (LMWID), which is known to cause reactions to the carrier substance in affected individuals. However, LMWID is no longer approved in Switzerland anyway.
Another clue is provided by the latency period of anaphylaxis: a large proportion of reactions occur very quickly; especially with parenteral substances, it is atypical for a person to develop a reaction only after 15 minutes. “If someone gets an infusion, whether it’s iron or a biologic or chemotherapeutic, for example, and the reaction doesn’t come until 15 or more minutes later, that’s more indicative of nonspecific mast cell activation or a pseudoallergic mechanism,” Dr. Jörg explained.
Iron administrations often release complement gap products such as anaphylatoxin C5a, which can lead to mast cell degranulation, the expert said. “This is often a dose issue, meaning the reactions occur during the course or toward the end of the infusions or when the infusion is administered very quickly.”
In the case of the 50-year-old, doctors changed the drug and administered the infusion very slowly over a two-hour period. The woman tolerated this without any problems. Dr. Jörg did not perform a skin test on the patient. In such cases, this is not expedient because it is irritating. The allergist also advises against premedication, as this can lead to mild reactions being masked.
Case 3: X-ray contrast agent
A 38-year-old female patient required a CT scan of the abdomen and received an injection of the radiographic contrast agent iomeprol. Shortly after administration, she developed flushing, hypertension, nausea, heat sensation, and isolated urticarial skin lesions, especially on the arms.
The team at Inselspital first performed skin testing: “For severe reactions, we always do a prick test first; for milder reactions, we test intradermally in certain concentrations, which is more sensitive.” The 38-year-old’s skin test was negative, and there were no indications of an allergy.
This is often the case with mild reactions, which tend to be triggered by nonspecific mast cell activation. Severe reactions (e.g., with hypotension and bronchospasm), on the other hand, tended to indicate allergy. In the case of anaphylaxis or moderate to severe reactions, allergological clarification is always mandatory to see which substances can be used in the future.
Premedication is a good way to suppress milder nonspecific mast cell activation, but it is a misconception to use it for allergies, Dr. Jörg says: “An allergic reaction will break through despite premedication.” That’s precisely why it’s important to clarify in advance whether an allergy or nonspecific mast cell activation is present, he said.
Take-Home Messages
- Pseudoallergic reactions are based on direct activation of mast cells and cannot be distinguished with certainty from an allergic reaction in the acute event.
- As a rule, reactions tend to be milder and occur with a delay in parenteral drug administration (clear dose dependence).
- The distinction is central, since which substances can be administered again depends on it.
- Skin testing cannot detect pseudoallergy.
Congress: FomF Update Allergology
Sources:
- FomF Update Allergology – Expert Forum. Lecture “Pseudoallergy to drugs. Diagnosis and therapy options”, 6.04.2023.
- Arastu AH, Elstrott BK, Martens KL, et al: Analysis of Adverse Events and Intravenous Iron Infusion Formulations in Adults With and Without Prior Infusion Reactions. JAMA Netw Open 2022; 5(3): e224488; doi: 10.1001/jamanetworkopen.2022.4488.
InFo PNEUMOLOGY & ALLERGOLOGY 2023; 5(3): 18-19.