Consistent topical basic therapy can improve skin hydration and restore skin barrier function. The individual selection of ingredients is based on the symptoms. A combination of hydrophilic and lipophilic ingredients is preferable.
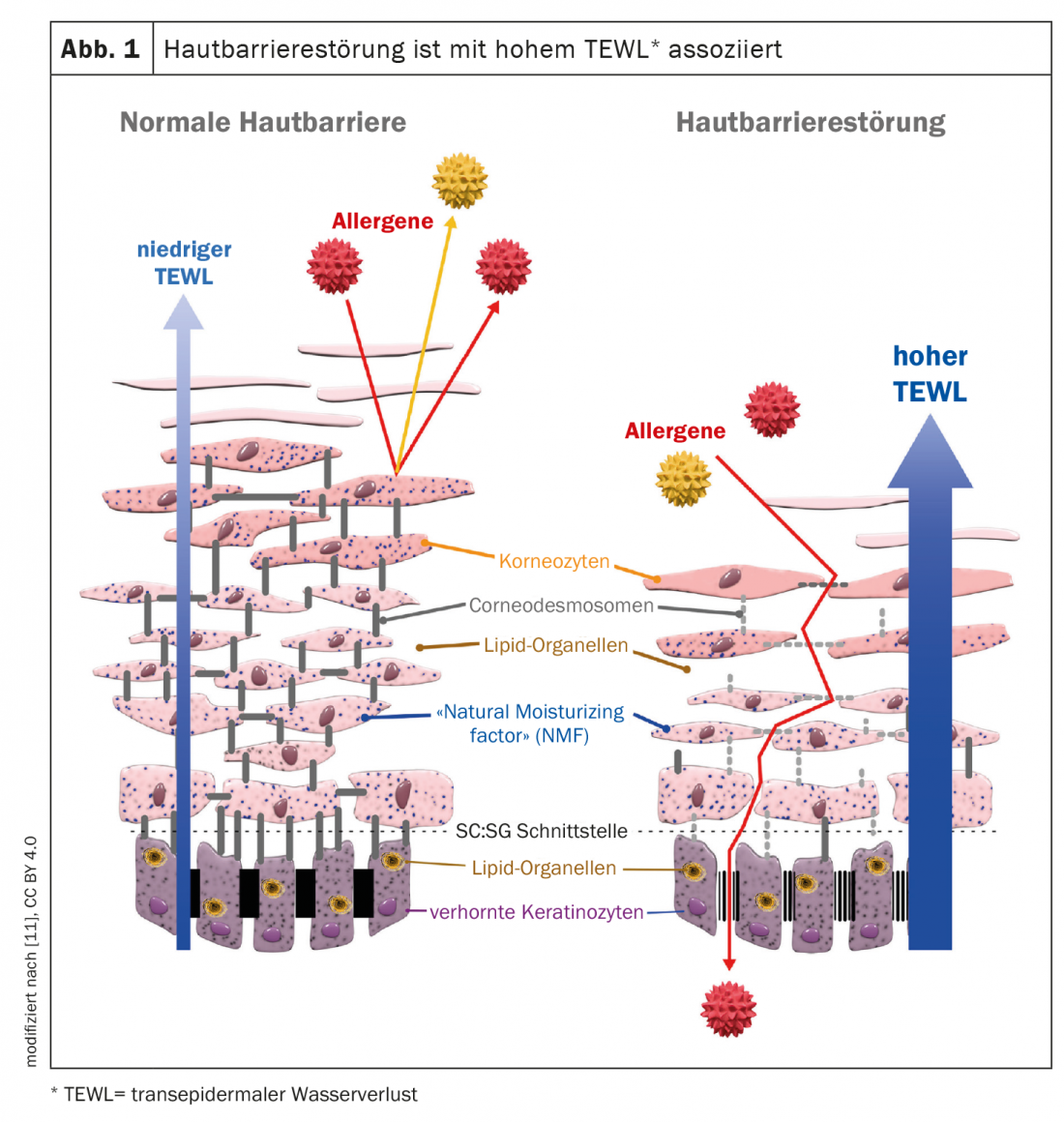
In the case of xerosis cutis (synonym: xeroderma) is a skin condition poor in hydrolipids, which is characterized by a reduced quantity and/or quality of lipids or hydrophilic substances [1]. Objectively recognizable signs of xerosis cutis include dry, scaly, rough, and lackluster skin that may be characterized by decreased elasticity, a coarsening of the skin’s relief, and wrinkling to erythema and fissures [2]. Tightness and pruritus can also be perceived individually as pain or burning sensations and significantly affect the quality of life of those affected. In addition to constitutional xeroderma or xeroderma caused by exogenous factors, it frequently affects patients with atopic dermatitis, psoriasis, or ichthyosis, and xerosis cutis is also a possible symptom in certain internal diseases (e.g., diabetes, renal and biliary diseases) [2]. A functioning intercellular lipid layer, proper arrangement and differentiation of corneocytes with sufficient levels of natural moisturizing factor (NMF) are crucial for an adequate skin moisture content of 10-20% [2]. Measurement of barrier function via transepidermal water loss (TEWL) by tewametry is an important parameter for objective assessment of xerosis cutis. Often, xeroderma is associated with an epidermal barrier disorder and thus an increased sensitivity to environmental influences, irritants and allergens (Fig. 1). In an epidemiologic study including over 48,000 individuals, the odds ratio (OR) for atopic eczema was 3.99 (CI 3.42-4.65) [3]. Basic topical skin care is recommended in national and international guidelines for all stages and severities of atopic dermatitis [4–6].
Basic principles of topical therapy of xerosis cutis
Essentially, it involves adding moisture in the form of natural moisturizing factor (NMF) or “humectants,” replenishing barrier lipids, and reducing moisture loss by forming a lipid film on the surface [2]. Regular applications of moisturizing and lipid-containing topicals can counteract skin dryness and associated skin barrier disorders and itch symptoms [6]. The galenics of the product used should always be tailored to the individual skin condition, with more hydrophilic formulations being recommended in acute phases of eczema, while more lipid-rich formulations can be used in interval phases [7]. Hydrophilic ingredients mostly consist of low-molecular, water-binding substances (e.g. glycerin or urea). Due to their low molecular weight, these can penetrate the stratum corneum, where they take over the role of the “Natural Moisturizing Factor” (NMF) or act as “Humectants”. NMF is essential for the water-binding capacity of the horny layer. In the case of lipophilic ingredients, the mineral oil-based hydrocarbon mixtures (e.g., petrolatum or kerosene) form a thin lipophilic film layer on the surface of the skin, which helps to improve the barrier function and increase the water content of the skin [2].
Adherence and compliance are crucial
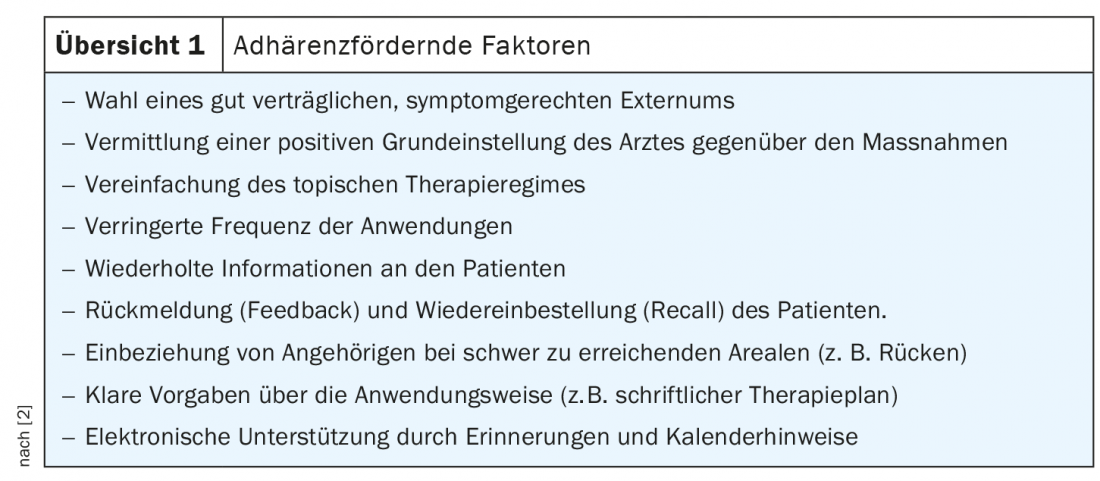
A prerequisite for successful treatment is the regular application of topical measures. Compliance and adherence play an important role [8,9]. Adherence research shows that consistent implementation of recommended topical therapy is often not optimally implemented. Non-adherence is influenced by a variety of factors. The points summarized in Overview 1 may help improve adherence [10]. Sufficient information to the patient as well as a good understanding of the patient about the implementation of the agreed measures is a basic requirement. It may be helpful to explain the significance of xerosis cutis to the patient in simple terms and to explain the benefits of treatment using pictures and diagrams. Offering the opportunity to try out suitable preparations in the practice can also have a positive effect. In addition, patients should be actively approached in advance and during the course of treatment as to whether there should be any obstacles to the use of topical measures. If there is evidence of poor adherence, it is useful to ask patients about possible reasons [2].
Literature:
- Kresken J, Daniels R, Arens-Corell M: Guideline of the GD Gesellschaft für Dermopharmazie e.V.: Dermocosmetics for cleansing and care of dry skin. Society for Dermopharmacy, April 30, 2009. .
- Augustin M, et al: Position paper: diagnosis and therapy of xerosis cutis. JDDG 2018; 16 Suppl 4: 3-35.
- Augustin M, et al: Prevalence, predictors and comorbidity of dry skin in the general population. JEADV 2019 33(1): 147-150.
- Eichenfield LF, et al: Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. JAAD 2014; 71: 116-132.
- Werfel T, et al: S2k guideline on diagnosis and treatment of atopic dermatitis–short version. JDDG 2016; 14: 92-106.
- Wollenberg A, et al: Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. JEADV 2018; 32: 657-682.
- Statement of the Gesellschaft für Dermopharmazie e.V.: Topical basic therapy for neurodermatitis, www.gd-online.de (last accessed 20.10.2022).
- World Health Organization (WHO): Adherence to long term therapy: evidence for action. www.who.int/chronic_conditions/adherencereport/en/2003, (last accessed 20.10.2022)
- Osterberg L, Blaschke T: Adherence to medication. N Engl J Med 2005; 353: 487-497.
- Augustin M, et al: Adherence in the Treatment of Psoriasis: A Systematic Review. Dermatology 2011; 222(4): 363-374.
- Katibi OS, et al: Moisturizer therapy in prevention of atopic dermatitis and food allergy: To use or disuse? Ann Allergy Asthma Immunol 2022; 128(5): 512-525. www.annallergy.org, (last accessed 20 Oct 2022).
DERMATOLOGIE PRAXIS 2022; 32(5): 58-59











