Functional abdominal pain can lead to a significant impairment of the quality of life and daily coping of the affected person and can already occur in adolescence. Chronification is common and requires a treatment strategy tailored to it. Among other things, cognitive-behavioral therapy methods and the use of herbal-based medicines have proven effective.
Functional gastrointestinal complaints cannot be explained by somatic disease or specific bodily functions (e.g., menstrual periods), nor by drug use or toxic effects, and occur over a period of at least 6 months. According to the current Rome IV criteria, epigastric pain (EPS), characterized by dominant upper abdominal pain or burning and is considered one of the two leading symptoms of functional dyspepsia (FD) (Fig. 1) [1].
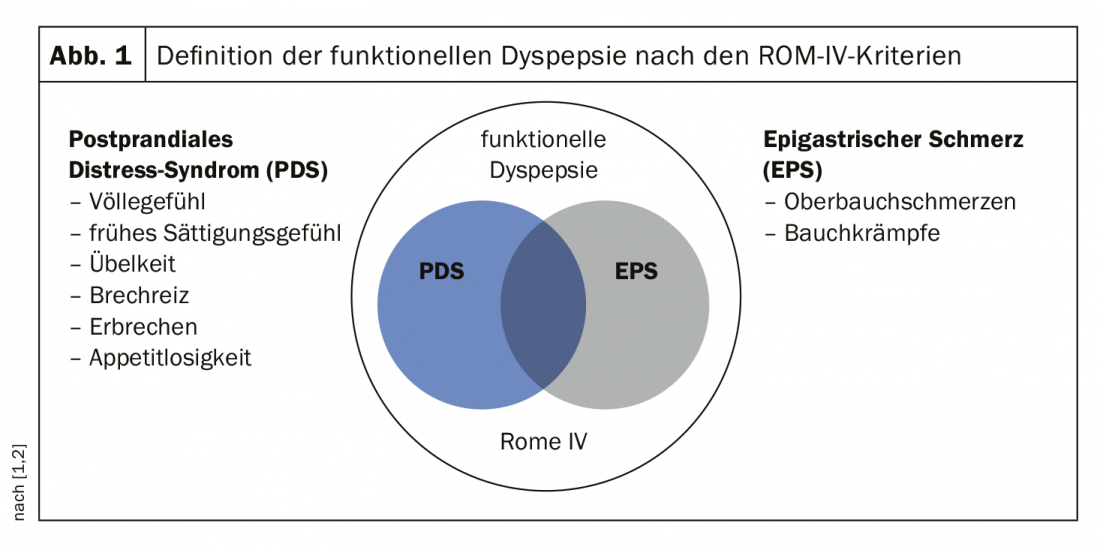
The second leading symptom of FD is postprandial distress syndrome (PDS), which is characterized by feelings of fullness and premature satiety. With a prevalence of 10-20%, FD is one of the most common functional disorders of the gastrointestinal tract [2]. In the prospective DIGEST study (“Domestic International Gastro Enterology surveillance Study”), approximately one-third of over 5500 respondents in a representative sample of the general population reported dyspeptic symptoms, with 6.5% suffering from acute and 22.5% from chronic dyspeptic symptoms [3]. The latter are characterized by a periodic alternation of acute symptoms and symptom-free or symptom-free intervals. Sustained freedom from symptoms is achieved by only one fifth of FD patients [1,4–6]. The etiology of functional upper abdominal pain is not fully understood, but visceral hypersensitivity, i.e., hypersensitivity to sensations in the digestive tract, is thought to play a role. Psychosocially stressful life situations and mental disorders (e.g. depression, anxiety disorder) are also possible influencing factors. Several empirical findings confirm that there is a relationship between psychological factors and functional gastrointestinal symptoms. For example, Steinsvik et al. demonstrate that there is a positive correlation of postprandial gastrointestinal symptoms with an anxiety problem and with neurotic symptoms [7]. Measurement tools used included the Visceral Sensitivity Index and the Eysenck’s Personality Questionnaire-neuroticism.
| Chronification often already in the teenager age As a 2020 study by Sjölund et al. [19] shows, abdominal pain at age 12 is a risk factor for functional gastrointestinal symptoms at age 16. In this prospective population-based empirical study in Sweden, data from 4089 children in the 1994-1996 birth cohorts were analyzed with respect to epigastric complaints at 1,2, 12, and 16 years of age. In 44.9% of those affected by abdominal pain symptoms at age 12, these persisted until age 16, and the risk of functional gastrointestinal symptoms in general was significantly increased. In contrast, there was no statistical association with upper abdominal pain in early childhood. Parents were interviewed for information on symptoms at 1-2 years of age; information on symptoms at 12 and 16 years of age was based on self-reports. |
Multimodal treatment is recommended for adolescents
After ruling out organic causes and determining the diagnosis of functional abdominal complaints, psychological procedures play an important role in treatment. The effectiveness of cognitive-behavioral therapy methods has been empirically demonstrated many times [8–10]. Within the framework of psychoeducation, the pathophysiological relationships of the functional complaints are explained. In addition to the model of visceral hypersensitivity (lowered individual pain threshold), trigger factors such as stress are also addressed. The treatment goal of cognitive-behavioral therapy methods is to reduce pain symptomatology and improve quality of life by learning constructive coping behaviors. In addition to psychoeducation, relaxation methods, various cognitive procedures (e.g., distraction techniques, cognitive restructuring), and stress reduction measures can be used [11–13]. Relaxation methods such as progressive muscle relaxation, imagination (fantasy journeys) or autogenic training can counteract the pain-induced tension. Cognitive restructuring is about ensuring that latent chronically persistent pain symptoms are not experienced as uncontrollable, but that active coping behavior is possible through pain management strategies. This also includes reduction of passivity in order to promote the patient’s fitness for everyday life, including vocational-social integration (education, occupation) [14]. Among the drug approaches for the treatment of functional dyspepsia in adolescence, probiotics and peppermint oil-containing drugs are recommended [15]. Carmenthin® is a phytopharmacological preparation based on peppermint and caraway oil, which is authorized for use by health insurance companies in Switzerland for adults and adolescents aged 12 and over for the treatment of mild cramps, bloating, epigastric pain and flatulence [16]. The analgesic and relaxing effects of peppermint oil on the muscles of the gastrointestinal tract are based on the binding of the ingredient menthol to the cold receptor (TRPM8), respectively, a cold signal triggered by it, followed by an inhibitory effect on pain transmitting nerves [17]. The tolerability of Carmenthin® is good even with frequent and long-term use [18].
Literature:
- Stanghellini V, et al: Rome IV – Gastroduodenal Disorders. Gastroenterology 2016 pii: S0016-5085(16)00177-3
- Madisch A, et al: The Diagnosis and Treatment of Functional Dyspepsia. Dtsch Arztebl Int. 2018 Mar; 115(13): 222-232.
- Eggleston A, Farup C, Meier R: The domestic/international gastroenterology surveillance study (DIGEST): design, subjects and methods. Scand J Gastroenterol 1999; 231(Suppl): 9-14.
- Ford AC, et al: What is the prevalence of clinically significant endoscopic findings in subjects with dyspepsia? Systematic review and meta-analysis. Clin Gastroenterol Hepatol 2010; 8: 830-87.
- Talley NJ, Ford AC. Functional dyspepsia. N Engl J Med 2015; 373: 1853-1863.
- Talley NJ, Walker MM, Holtmann G: Functional dyspepsia. Curr Opin Gastroenterol 2016; 32: 467-473.
- Steinsvik EK, et al. Postprandial Symptoms in Patients With Functional Dyspepsia and Irritable Bowel Syndrome: Relations to Ultrasound Measurements and Psychological Factors. J Neurogastroenterol Motil 2020; 26(1): 96-105.
- Eccleston C, et al: Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2009: CD003968.
- Huertas-Ceballos A, et al: Psychosocial interventions for recurrent abdominal pain (RAP) and irritable bowel syndrome (IBS) in childhood. Cochrane Database Syst Rev 2008: CD003014.
- Palermo TM, et al: Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: an updated meta-analytic review. Pain 2010; 148: 387-397.
- Seemann H: Psychoeducation in the treatment of pain. In: Behrendt BB, Straub A (eds.): Handbook of Psychoeducation & Self-Management. Behavioral therapy approaches for clinical practice. Tübingen: dgvt-Verlag 2005; 347-412.
- Warschburger P, Gross M: “Stop the pain” – A cognitive-behavioral treatment program for children with abdominal pain – First results of a pilot study. Behavior Therapy 2008; 18: 162-7.
- Zernikow B: Pain management in children, adolescents and young adults. Heidelberg: Springer 2009.
- Di Lorenzo C, et al: Chronic abdominal pain in children: a technical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2005; 40: 249-61.
- Andrews ET, Beattie RM, Tighe MP: Functional abdominal pain: what clinicians need to know. Archives of Disease in Childhood, 09 Mar 2020. DOI: 10.1136/archdischild-2020-318825 PMID: 32152039
- Specialized information: www.compendium.ch
- Deutsche Apothekerzeitung (DAZ): DAZ 2018 (9): 73, 01.03.2018.
- Madisch A, et al: Internist 2015; 56, (Suppl. 1): 28.
- Sjölund J, et al: Prevalence and Progression of Recurrent Abdominal Pain, From Early Childhood to Adolescence. Clinical Gastroenterology and Hepatology 2020,:https://doi.org/10.1016/j.cgh.2020.04.047
GP PRACTICE 2020; 15(8): 24-25.