Not only in the warm season there are many potential targets of ectoparasites. For example, scabies (also called scabies) occurs more frequently in our latitudes in winter. What should be considered for these and other epizoonoses with regard to diagnostics, therapy and further intervention measures?
You are not safe from them anywhere. Be it bugs, fleas, plant mites, grass mites, mites of pets and livestock, trombidiosis or the human-borne scabies and lice. A detailed history, including inquiries about whereabouts, contacts with animals, plants, and people, helps to quickly narrow down the possible suspects. This is because the arrangement of the skin lesions and the clinical reactions – be they urticarial, pruriginous, nodular or pseudolymphomatous – do not necessarily indicate the causative agent.
Due to an increase in mobility (incl. sex tourism) and leisure activities in nature, as well as in connection with global warming, it can be assumed that we will be increasingly confronted with the issue of epizoonoses and ectoparasitoses.
Reactions in own bed
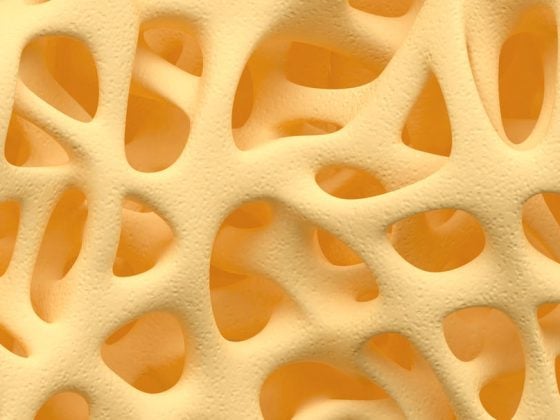
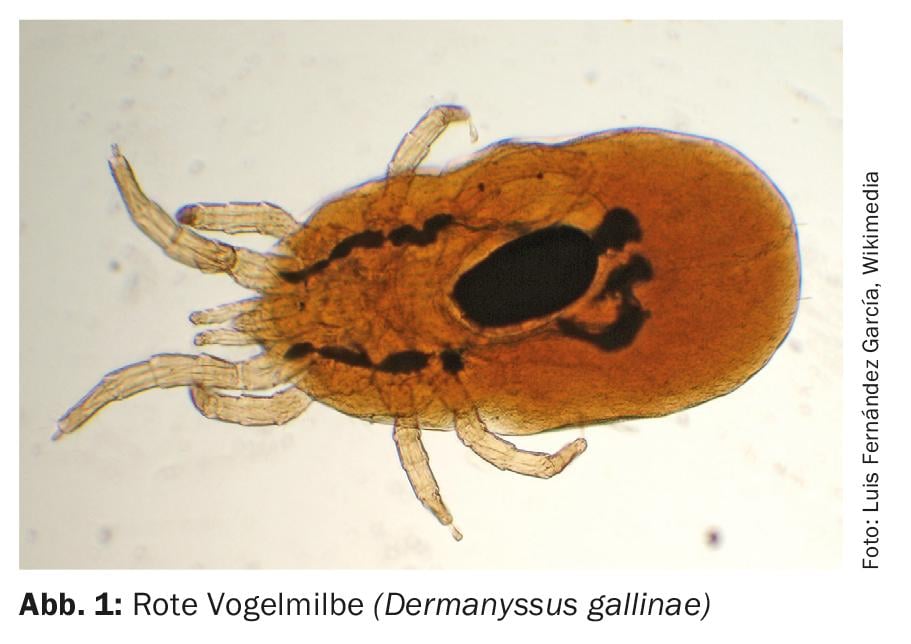
For example, if the bed is near the window under the roof, a pigeon roost on the roof can cause reactions from pigeon mites (Fig. 1), especially in young children. The reactions are more or less unsystematically distributed all over the body. Depending on the duration of exposure, reactions can sometimes look quite severe, with pruriginous or even mildly pseudolymphomatous features [1]. Therapy includes clearing out the pigeon loft, applying repellents, and topical therapy of bite sites with short-lasting high-potency steroids.
Incomparably more common are the usually more pronounced infiltrated maculopapules with a central slightly hemorrhagic halo and varying in size up to more than 10 cm. Usually it is only a small number of lesions occurring at the same time. These are caused by bed bugs (Cimex lectularius) (Fig. 2) . The bugs crawl between the gaps in the parquet, in the carpet or even in the irregularities in the plaster of the walls, can starve for up to a year and are usually active in the spring. The apartment and the corresponding room usually has a special, slightly musty smell. The attack usually takes place in the middle of the night and if you turn on the light, it is possible to catch a critter. The dam is 4-6 mm long (Fig. 3), the dorsal carapace has slight transverse grooves. With repeated bites over years, reactions usually become more severe and hyperergic or even allergic reactions with bronchial asthma develop [2].

In addition to local therapy and the application of insect repellent, an exterminator should also be organized here, who works, for example, with chlorpyrifos, a granulate that is spread and eradicates the bugs. In addition, there is a whole range of other measures such as vacuuming, heat treatment, cold treatment, application of insecticides/pesticides or inorganic materials such as diatomaceous earth to the use of organic materials such as bean leaves.

Reactions in foreign beds
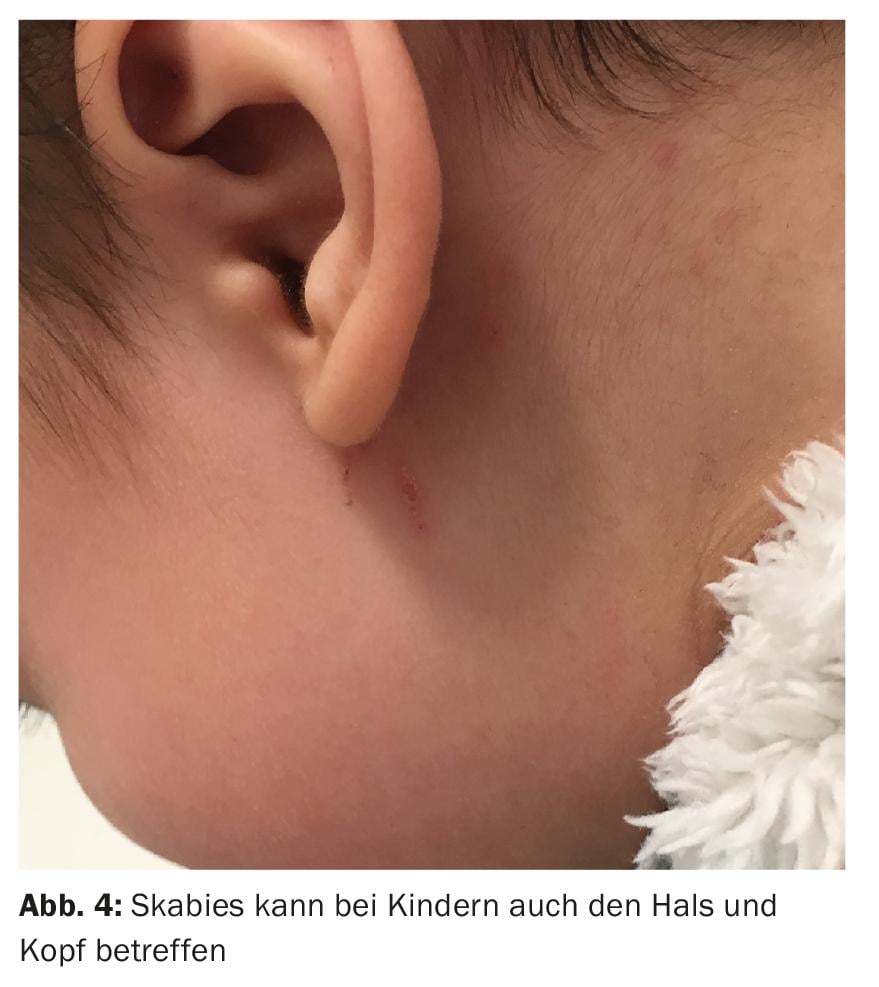
Depending on the type of accommodation and being with unfamiliar people, reactions to bug bites may occur in addition to possible sexually transmitted diseases. Typically, two weeks after an excursion, a very pronounced itching appears, which occurs at night and mainly affects the flexures, from the neck to the spaces between the toes. This is a case of scabies. Gradually, other family members are affected, albeit to varying degrees. In adults, infestation of the head does not occur, but it is possible in children (Fig. 4) and rarely in very old patients [3]. Clinically, there are hyperkeratotic papules as well as small ducts, especially on the fingers and feet. Sometimes, in a so-called mite mound, the mite mother can be found dermatoscopically, which manifests as a tiny black triangle and watches over her buried eggs. I personally do not treat scabies without a positive microscopic specimen (the greatest accuracy is from the genital area) with either clear oval to teardrop-shaped black fecal balls (skyballa) and the transparent eggs, which are about 50 µm long, or direct evidence of the mites.
Therapy of scabies can be based on the current S1 guideline [6]. Among other things, the age of those affected is a criterion. It is also important that all family members are treated at the same time – even those who are currently asymptomatic but may already be infected. In addition to the two-day therapy from the neck to the sole of the foot including the spaces between the toes and subungually with topical ivermectin or four to five percent permethrin cream, there is also the possibility in Switzerland of administering ivermectin in tablet form, although corresponding preparations are only available on order abroad and it actually represents an off-label indication.
Following therapy and parallel measures such as changing bedding and clothing twice and washing at at least 60°, post-scabies eczema develops, especially in atopic patients, and may last for four to six weeks and should not be confused with a recurrence of scabies. Therefore, refatting therapy should be started immediately after the two-day treatment, if necessary also with topical steroids several times a week as part of an interval treatment.
Unplanned contact with unknown persons can also transmit the pubic crab louse (pediculosis pubis), which nests in the apocrine glands in the genital area and axillary, and more rarely in the eyebrows, eyelashes, and abdominally. In children, the crab louse may also occur on the face. The itching is not particularly severe, but a typical feature are the small hemorrhagic spots, the maculae ceruleae. It is important here in the case of sexual contact to address possible transmission of sexually transmitted diseases such as syphilis, HIV and scabies. See the treatment of head lice or scabies.
Reactions in the gazebo or near bushes
It was wonderful to sit outside on the veranda in the evening – had it not been for such an unpleasant reaction on all open skin areas! Trombidiosis, also called autumn or spring mite infestation, causes urticarial and maculopapular ictal reactions after four to twelve hours. In most cases, the mites crawl to the nearest waistband or barrier such as shoulder or bra (Fig. 5) and lay their larvae there. Thus, the reactions to the parasites (Neotrombicula autumnalis) are found distributed on the extremities and not linearly arranged. Particularly in thin-skinned and moist areas of the body – i.e. the back of the knee, groin, bend, belly button, armpits – the parasites nest for three to five days. They bite into the skin with their sickle-shaped mouthparts and leave their host as soon as they are “full”. When you scratch yourself for the first time after being stung, you are usually removing the larva that sits in the top of the wheal. By taking a history, the location of the possible attack can be located. Classic examples are barbecuing in a forest clearing or drinking tea in an arbor or garden restaurant.

Quick relief is achieved by insect repellent. However, for a sustainable solution, the relevant bushes must be sanitized, e.g. by spraying with a 1-2% neem oil solution (from the Indian neem tree Azadirachta indica).
Reactions in shallow waters
Garden ponds, ponds, and shallow waters in lakes with relatively warm water temperatures bring on the summer itch (“swimmers itch,” called cercarial dermatitis or schistosomiasis), which often causes discomfort twelve hours after exposure and manifests as urticarial papules that become flat. These are triggered by cercariae (Schistosoma sp.), which is transmitted via the intermediate host fleas-geese-goose droppings-water snails. These small skin parasites nest in the skin but do not penetrate it and die with fading dermatosis after three days. History of whereabouts the day before seeding usually leads to a tentative diagnosis. It is not possible to protect oneself against it, so that symptomatic therapy and avoidance of the water during the warm season are often the only options. With global warming, the frequency of Shistosoma-infested waters and corresponding human exposure is increasing in the northern hemisphere [4].
Kindergarten reactions
If it itches on the head, head lice are the primary suspect; if it itches on the body and at night, scabies. With head lice, there is often a small epidemic among students. If the laustante does not pay a visit to the school, the parents must provide louse search and treatment. If you search the hair, you will find so-called “nits”, mostly empty shells that stick to the hair. It is more difficult to find the live lice, which crawl around on the scalp and are only about one to two millimeters in size. Again, it is important that all children are treated at the same time. This is usually done with a special shampoo containing the substances malathion (1%) or permethrin (1%), which is left to act for ten minutes. This procedure is repeated after one – or two weeks in the case of malathion. As prophylaxis, continue treatment five times a week for those over two years of age: Malathion, pyrethrins, and permethrin are considered first-line treatments. Isopropyl myristate/ST-cyclomethicone solution and dimeticone can be used as alternatives if therapy fails [5]. Internal administration of ivermectin would also be an alternative. In addition, the nit comb should not be missing, with which the still existing larvae and also the empty and dead larvae bags can be removed from the hair.
Reactions in the house
There are a large number of possible sites of attack, necessitating extensive detective differential diagnosis. First, the following questions must be answered: Are there pets in the household? Has there been any contact with pets? What is the distribution of skin irritations? Is there a so-called bite road? Does anyone have old dresses/secondhand clothes that may have been in the box for a long time? Biting reactions in a bite street indicate fleas that hop linearly and often infest the fragrant children or women in isolation, while the others in the room or family are unaffected. A more grouped arrangement of skin lesions or solitary lesions may be due to animal mites and, as with flea bites, may affect only individual family members. Humans are considered only as intermediate hosts in the case of animal mites and fleas, but animals must be examined and treated. The application of insect repellent also works excellently as a prophylactic.
Special: We are all mite carriers: the demodicose
Almost forgot that we humans are carriers of hair follicle mites especially in adulthood (Demodex folliculorum). Demodex mites proliferate especially in cases of coarse-pored skin, rosacea and seborrhea and lead to an additional inflammatory component, indeed they are partly entirely responsible for a papular and also itchy dermatosis on the face. (Fig.6). The detection is relatively simple and so the elongated transparent mites can be detected in the microscopic direct preparation or also by tear-off preparation of the skin with transparent adhesive tape (stick and pull off several times) under the microscope in medium magnification. If the usual treatments for rosacea and acne are often of limited use here, the local application of ivermectin cream causes the itching and papules to disappear within days.

Take-Home Messages
- A combination of clinical examination, exposure, and other information is required to make the diagnosis. Information on whereabouts and contacts with humans and animals can provide clues to identify originators of bite reactions.
- The causative agent cannot necessarily be inferred from the expression of the skin lesions, although linear bite tracts suggest fleas and large reactions with a central hemorrhagic yard suggest bedbugs. Parasites on the skin can be diagnosed under the microscope – occasionally it is possible to find bed bugs or active fleas and mites early in the morning.
- If there is an epidemic infestation (e.g. in kindergarten or family), in case of scabies the simultaneous treatment of the whole collective and sanitation of the sources brings permanent cure.
Literature:
- Fehr M, Koestlinger S: Ectoparasites in small exotic mammals. Vet Clin North Am Exot Anim Pract 2013; 16(3): 611-657.
- Anliker MD, Wüthrich B: What is your diagnosis? Bedbug sting reaction caused by Cimex lectularius (common bedbug). Practice 1999; 88(49): 2017-2019.
- Modi K, Patel D, Shwayder T: Scalp-to-toes application of permethrin for patients with scabies. Dermatol Online J 2018; 24(5).
- Kaffenberger BH, Shetlar D, Norton SA, Rosenbach M: The effect of climate change on skin disease in North America. J Am Acad Dermatol 2017; 76(1): 140-147.
- Cummings C, Finlay JC, MacDonald NE: Head lice infestations: A clinical update. Paediatr Child Health 2018; 23(1): e18-e24.
- Sunderkötter C, et al: S1 guideline on the diagnosis and treatment of scabies (AWMF register number: 013-052). www.awmf.org/uploads/tx_szleitlinien/013-052l_S1_Skabies-Diagnostik-Therapie_2016-12.pdf, last accessed 06 Nov 2018.
HAUSARZT PRAXIS 2019; 14(1): 31-34
DERMATOLOGIE PRAXIS 2019; 29(1): 12-15