The treatment of chronic wounds is part of everyday practice. Often, these patients are multimorbid and require both causal and symptomatic treatment. The general practitioner plays an important role in interdisciplinary care, and the use of telemedicine services has also become established as part of the digitalization of healthcare. This has proven particularly effective in the care of chronic ulcers, as demonstrated by several study projects.
Approximately 90% of chronic wounds are vascular, with the majority being venous leg ulcers due to chronic venous insufficiency [1]. Other common causes include arterial occlusive disease, diabetic angiopathy, and pressure ulcers [1]. If a wound does not heal within eight weeks despite guideline-compliant treatment, it is by definition a chronic wound. Many patients with wound healing disorders are affected by multimorbidity and are dependent on outside help [2]. There is a need for multiprofessional integrated care. The general practitioner plays a key role, and increasing digitization in healthcare has also opened up new opportunities in the field of wound care [2]. The care of chronic wound patients with the inclusion of telemedical services has delivered convincing results both in terms of feasibility and acceptance by patients and users, according to PD Dr. med. univ. Barbara Binder, University Department of Dermatology and Venereology, Medical University, Graz (A) [3].
Saving resources while maintaining treatment standards
Being able to obtain medical advice quickly and regardless of location is becoming increasingly important. The current Corona pandemic is further driving the trend toward digitization in healthcare [4]. This also applies to the field of wound care (box) [5]. It has been shown that despite saving resources, treatment standards have been maintained, Dr. Binder said. With regard to wound management, the 2018 guidelines “Practice of Teledermatology” state that there is a high level of agreement between morphologic findings obtained by telemedicine and presence findings [6]. “Digital reporting can be equated to face-to-face reporting,” according to the corresponding statement of the expert consensus. The process of telemedical care can be summarized as follows: Patient data is recorded via PC, digital camera, smartphone, or app. Real-time or store-and-forward technologies are available for data transfer, with the latter being the most common. Data use” is defined as diagnostics, documentation, etc. Finally, the quality and data protection of the collected data is archived [6].
Local therapy of wounds in a holistic treatment approach
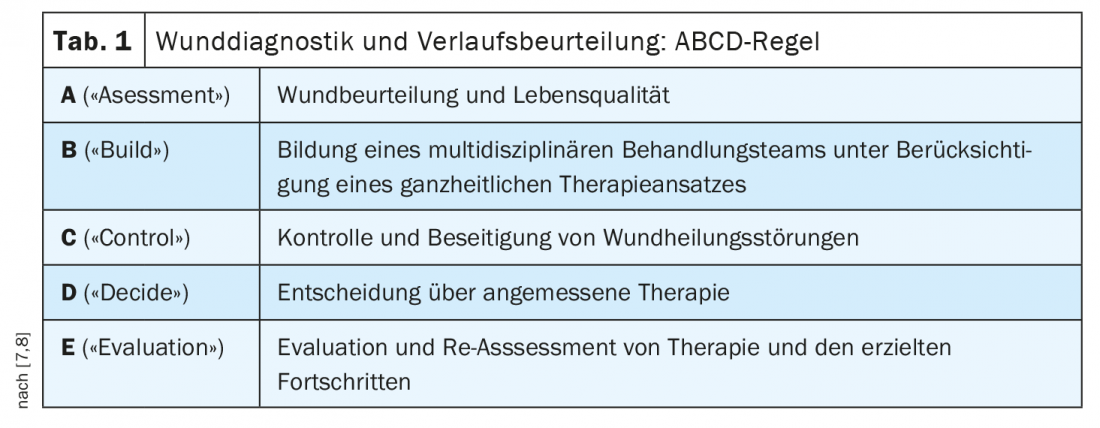
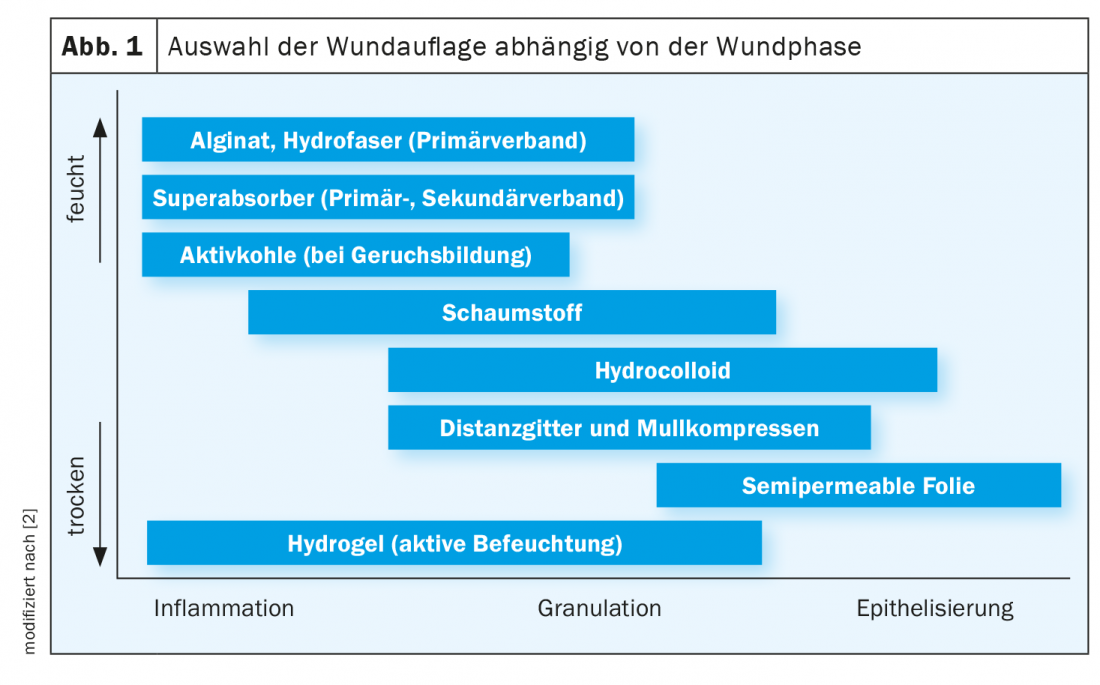
With regard to patients with chronic wounds, it is particularly important that the treatment concept is both causal and symptomatic. However, outpatient follow-up appointments for progress assessment and early detection of complications are often time-consuming and costly for patients. The use of telemedicine could offer relief here, according to Dr. Binder [3]. Reducing the number of doctor and clinic visits and eliminating transportation results in time and cost savings without compromising the quality of medical care. The most important steps in the care of wound patients are diagnostics, treatment planning, dressing changes and checks. The ABCDE rule is a practical guideline for wound diagnosis and assessment recommended by the German Chronic Wound Initiative [7,8] (Tab. 1). The selection of the appropriate wound dressing is phase-dependent [2] (Fig. 1); the T.I.M.E. scheme (“Tissue”=tissue, “Infection”=infection, “Moisture”=moisture, “Edge”=wound edge), among others, serves as an aid here. In an infected wound, the goal is to reduce the germ load, for which wound dressings with antimicrobial substances can be used. If a moisture imbalance is present, appropriate wound dressing materials (e.g., hydrogel, foam dressings, negative pressure wound therapy) can be used to create a wound environment that promotes healing. If epithelialization of the wound margin is to be promoted, the use of negative pressure wound therapy may be useful. For the therapy and recurrence prophylaxis of venous leg ulcers, ulcer compression stocking systems are also indicated.
Evaluation of telemedicine care in patients with chronic ulcers.
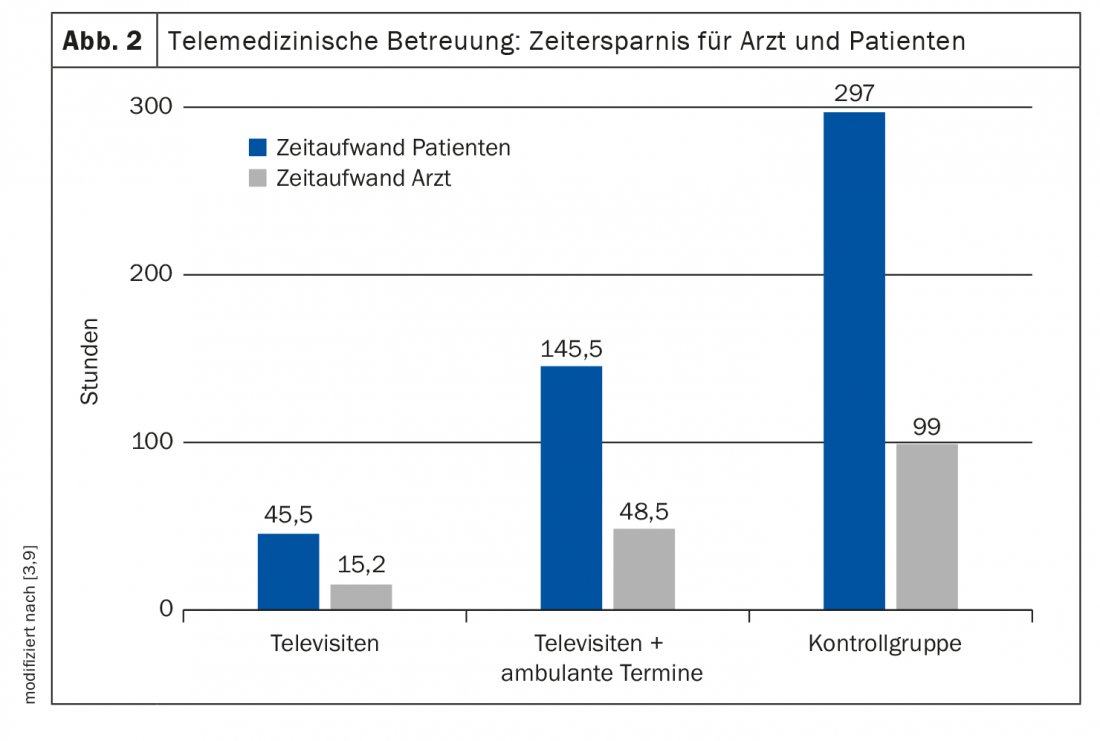
A study published in 2019 evaluated the implementation of telemedicine-assisted treatment for patients with chronic ulcers. A total of 40 patients (18 female and 22 male) were included in the study. The treatment period was about 6 months. Half of the subjects were assigned to the telegroup and half to the control group, and the median age was 75 years (range: 39 to 88) [9]. A special application was used in the telegroup to upload photos of the ulcers, clinical findings, and medical history. After reviewing the patient’s data, the specialist made a treatment recommendation and a follow-up appointment was scheduled. The results of the study showed that considerable time savings for physician and patient were achieved in the mainly telemedicine group compared to the control group [3,9] (Fig. 2). The acceptance and recommendation rate of teledermatological care was very high; at the same time, the number of clinical visits could be significantly reduced and thus also waiting times and transport costs for the patients. Per patient and month, 1.6 outpatient visits were performed in the control group, and only 0.6 in the telegroup. In six patients, care was provided exclusively via televisits. This is just one of the many examples of successful implementation of eHealth in wound care.
Conclusion: high patient satisfaction and good implementability
Several corresponding study projects have also been carried out and evaluated at the Medical University of Graz [10,11]. In the “Teleulcus” project, 16 patients with 45 chronic leg ulcers were cared for. The university wound center monitored wound status telemedically, and wound care was provided by ambulatory care services with the participation of primary care physicians in patients’ homes. All parties involved were satisfied with the processes and results, although it was recognized that digital images alone were not sufficient and that additional information was required on the general condition of the patients, relevant previous diseases, complications and previous response to therapy [11]. The conclusion of another study was also extremely positive [12]. A total of 16 patients with leg ulcers who were involved in home health care were included in the study. The initial examination at the clinic was followed by the telemedical support phase. The home care provider sent images of the wound once a week with additional information, including the patient’s general health . An expert then provided a clinical assessment with care-related medical notes. After three months, a follow-up examination was performed at the on-site clinic. Overall, the implementability of telemedicine care proved to be very good [12]. The quality of the transmitted image material was sufficient in 92% of the cases and a very good assessment of the clinical findings was possible. Acceptance of telemedicine care was high among both patients and caregivers.
Congress: Wound Congress Nuremberg (D), 2.12.2021
Literature:
- GP training Hamburg: Chronic wounds – the secrets of the wound manager, 13.08.2021
- Schlager J, et al: Wound care in family practice, 2020, issue 7-8.
- Binder B: Teledermatology and chronic wounds, Nuremberg Wound Congress, 2-3 Dec 21.
- Swiss Forum for Integrated Care: Vernetzte Grundversorgung, Trendszenarien 2028, www.fmc.ch, (last accessed 13.01.2022).
- Oropallo A, et al: J Wound Care 2021; 30(Sup2): S12-S17.
- Augustin M, et al: J Dtsch Dermatol Ges 2018; 16 Suppl 5: 6-57.
- Moore Z, et al: J Wound Care 2019; 28(3): 154-161.
- Dissemond J: J Dtsch Dermatol Ges 2017; 15(7): 732-734.
- Eber EL, et al: Dermatologist 2019; 70: 34-353.
- Medical University of Graz, Teledermatology www.medunigraz.at/universitaetskliniken/dermatologie-und-venerologie/forschung/teledermatologie (last accessed Jan. 13, 2022).
- Binder B, et al: Teledermatological care of patient with leg ulcers – a pilot project. EHEALTHCOM 2008(2): 53-55.
- Binder B, et al: Teledermatological monitoring of leg ulcers in cooperation with home care nurses. Arch Dermatol 2007; 143(12): 1511-1514.
HAUSARZT PRAXIS 2022; 17(1): 34-35