A study showed that treatment of diabetic foot ulcers with cold atmospheric plasma improves oxygen and nutrient supply to damaged tissue layers, stimulates blood flow and activates wound healing. This is of high clinical relevance for chronic wounds that are refractory to standard treatment.
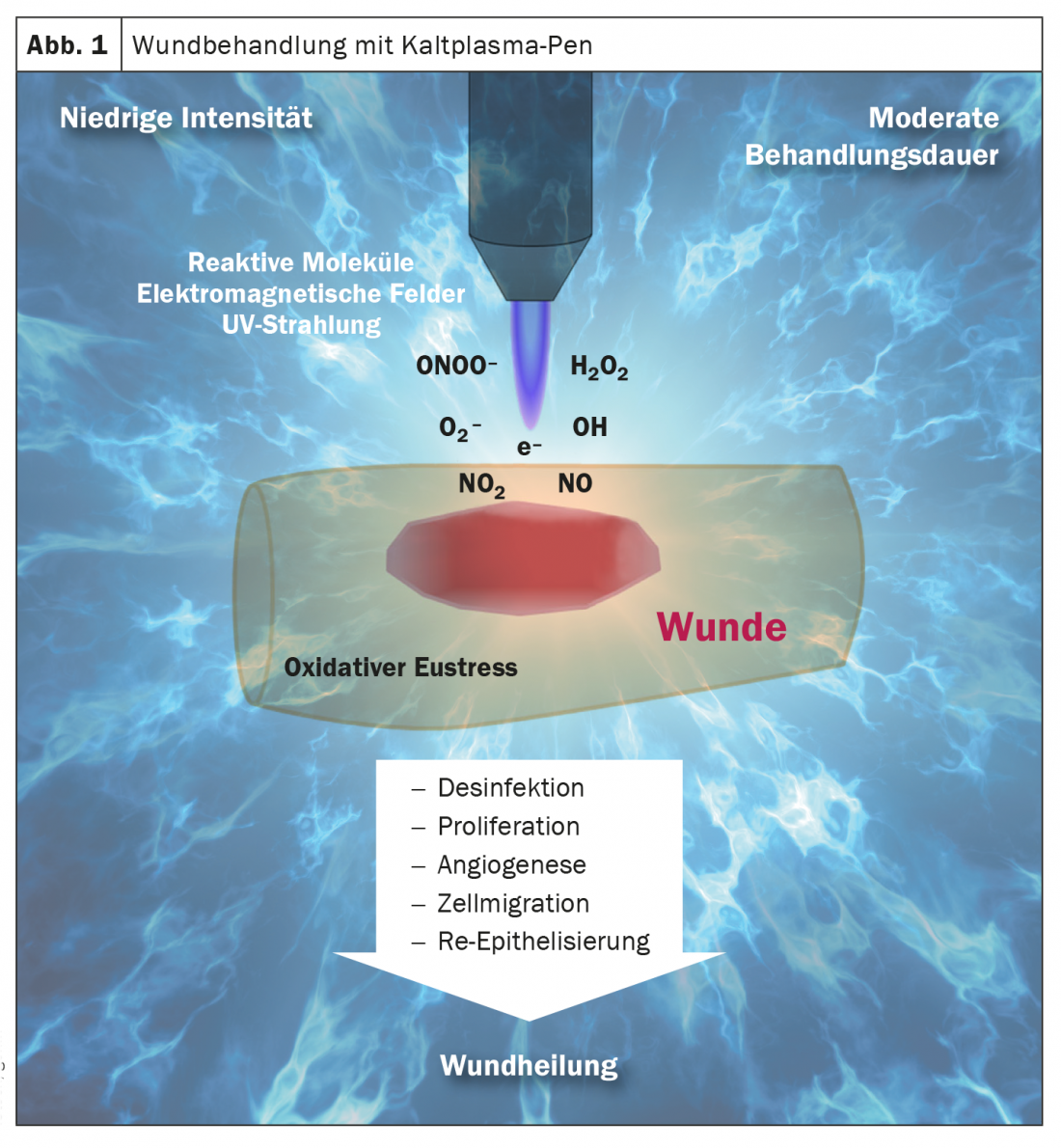
The management of chronic wounds remains a medical challenge and despite modern treatment methods, there are always wounds that do not close. In a prospective, randomized, placebo-controlled and patient-blinded clinical trial involving the Heart and Diabetes Center North Rhine-Westphalia (D), it was demonstrated that cold atmospheric plasma (CAP) significantly accelerates the healing process in chronic wounds refractory to standard wound therapy (Fig. 1, box).
Diabetic foot syndrome carries risk of amputation
Diabetic patients are prone to ulceration, which can easily become infected, progress to gangrenous wounds, and ultimately require foot amputation to prevent a life-threatening condition [1]. The prevalence of diabetic foot ulcers in Europe is 5.1% according to epidemiological data, with type 2 diabetics being affected slightly more frequently than and type 1 diabetics [3]. Prolonged hyperglycemia and repeated hypoglycemia also lead to impaired cognitive and psychomotor functions in the longer term due to neuronal changes caused by micro- and macroangiopathies. Diabetic neuropathy can lead to increased and unnoticed skin lesions and consequent damage to this important infection barrier [2]. Data from Germany showed that 85.6% of patients with minor amputations and 63.7% with major amputations were diabetic.
Cold plasma therapy as a supplement to standard wound care
Cold atmospheric plasma is a non-invasive therapy that acts painlessly on both the skin and underlying tissue layers. In this process, physical plasma is obtained by electrical excitation of noble gases, such as argon [4]. This is also called the fourth state of aggregation. To enable direct application to the body surface, the initially hot plasma is converted into cold plasma by temperature reduction. The cold plasma particles consisting of electrons and ions are applied with a special pen. The purely physical therapy principle has proven to be a useful addition to standard wound care in clinical practice [4]. Cold plasma therapy is a very well tolerated therapy option with few side effects and has great potential in the field of chronic wound care, as recent study data show.
Randomized controlled trial confirms clinical benefit
Forty-three inpatients with a total of 62 superficial or infected wounds* caused by diabetic foot syndrome were studied, in which no healing tendencies were apparent despite three weeks of standard wound therapy [5]. 33 wounds from 29 patients were randomized to cold atmospheric plasma (CAP) and 32 wounds from 28 patients were randomized to placebo. The final evaluation included 31 wounds per group. Study participants received eight applications of cold plasma or placebo in addition to standard wound care (box). The primary endpoints were defined as reduction in wound surface area and reduction in clinical infection and microbial burden compared to baseline.
**
defined. Secondary endpoints were time to infection reduction and relevant reduction in wound size (>10%) as well as treatment-associated adverse events and patient well-being assessment parameters. At the ninth session, i.e., after a two-week treatment period, the cold plasma-treated group showed a significantly greater reduction in wound surface area compared with the placebo group, thus fulfilling the primary endpoint of the study (Table 1) [5].

In addition, cold plasma treatment resulted in improvement in other parameters of wound healing. The authors summarize the effects observed in this study as follows: therapy with cold plasma led to a reduction in wound area, granulation, and acceleration of wound closure, independent of antimicrobial effect. No treatment-related adverse events occurred during treatment in either group.
* Wagner-Armstrong classification 1B or 2B.
** Baseline = start of treatment.
Literature:
- Moxey PW, et al: Lower extremity amputations–a review of global variability in incidence. Diabet Med 2011; 28(10): 1144-1145.
- Fürst T, Probst-Hensch N: Diabetes mellitus. Burden of Disease and Care in Switzerland, Obsan Report 20/2020, www.obsan.admin.ch (last accessed 06/15/21).
- Zhang P, et al: Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Annals of Medicine 2017; 49(2), https://doi.org/10.1080/07853890.2016.1231932.
- Stratmann B, Barten MJ: Cold plasma therapy for the treatment of chronic wounds. Forum Sanitas – The Informative Medical Magazine 2017 (3): 33-35. https://safw.ch/images/safw/dokumente/Barten-Stratmann.pdf.
- Stratmann B, et al: Effect of Cold Atmospheric Plasma Therapy vs Standard Therapy Placebo on Wound Healing in Patients With Diabetic Foot Ulcers: A Randomized Clinical Trial. JAMA Netw Open 2020; 3(7): e2010411.
- Swiss Diabetes Association, www.diabetesschweiz.ch/ueber-diabetes.html (last accessed 06/15/21).
- International Working Group on the Diabetic Foot (IWGDF): IWGDF Guidelines on the prevention and management of diabetic foot disease, 2019.
- Wound Network Kiel, https://wundnetz-kiel.de/kalt-plasma-behandlung-neue-wege-im-wundmanagement (last accessed 06/15/21).
- Boeckmann L, et al: Cold Atmospheric Pressure Plasma in Wound Healing and Cancer Treatment. Appl Sci 2020 (10): 6898.
HAUSARZT PRAXIS 2021; 16(7): 36-37














