In addition to the skin and respiratory tract, the eyes are also frequently affected by an allergic reaction. Both immediate-type, IgE-mediated, and late-type, T-cell-mediated reactions can occur on the eyelids and conjunctiva. The prototype of an immediate reaction of the eyelids is Quincke’s edema, and in the conjunctiva, hay fever conjunctivitis. In contrast, contact eczema in the eyelid area and gigantopapillary conjunctivitis are expressions of late-type allergy. Pathogenetically, atopic eyelid eczema and keratoconjunctivitis correspond to a combination of type I and type IV mechanisms.
Allergy is an exuberant specific immune response. Pathogenetically, the type I reaction (anaphylaxis type), immunoglobulin E (IgE)-mediated (most frequent clinical picture is allergic conjunctivitis), and the type IV reaction (tuberculin type), T-cell-mediated (most frequent clinical picture is contact eczema of the eyelids), are distinguished. Other examples of a type I reaction are anaphylactic shock after a bee sting or acute urticaria with Quincke’s edema after penicillin ingestion. The diagnosis of an IgE-mediated allergy is based, in addition to the medical history, on the performance of prick tests (immediate reaction after 20 minutes) and specific IgE determinations (RAST/CAP), occasionally on provocation tests (conjunctival, nasal, bronchial, peroral or subcutaneous, depending on the indication).
In the type IV reaction, a distinction is made between a sensitization phase, with presentation of the antigens (haptens) via dendritic cells (Langerhans cells) to T-helper cells in the regional lymph nodes, and an effector phase, where the sensitized T-lymphocytes come into contact again with the antigen-presenting cells in the epidermis/cutis and thereby release inflammation-causing lymphokines. The clarification of contact dermatitis is performed by means of epicutaneous samples (patch tests) with reading of the reaction after 48 and 72 hours and often requires great experience after the search for the suspected substance.
Allergic reactions of the eyelids
Allergic immediate reactions of the eyelids: The eyelids with the loose connective tissue are often the seat of swellings. It must be strictly differentiated whether the edema is an expression of a collateral swelling, as a consequence of an acute contact eczema, a contact urticaria (e.g. after latex contact), a local allergic event (e.g. after a mosquito bite in the eyelid area) or a genuine, hematogenously triggered Quincke edema, partly also in the context of an acute urticaria. Clinically, there may be pale eyelid edema or massive, deep edema; if allergic, itching and often conjunctivitis are present(Fig. 1). For etiology, immediate-type allergens include drugs, foods, inhalant allergens, insect bites (nonlocal, distant edema), and occasionally cosmetics.

Fig. 1: Quincke’s edema after aspirin (pseudo-allergy).
Differential diagnosis of Quincke’s edema must include hereditary angioedema due to C1 inhibitor deficiency (Fig. 2), ACE inhibitor-induced angioedema, autoimmune angioedema(Fig. 1), and idiopathic angioedema. Quincke’s edema, which is often triggered by aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs), has a pseudoallergic pathogenesis (imbalance in leukotriene metabolism). Infections (e.g., erysipelas) with collateral edema, eyelid swelling in acute contact dermatitis, eyelid edema due to an internal medical condition (hypothyroidism, nephropathy), and vena cava syndrome (thrombosis) must also be included in the differential diagnosis.

Fig. 2: Hereditary angioedema due to C1 inhibitor deficiency.
Contact eczema of the eyelids: Contact eczema of the eyelids may be acute (Fig. 3) or subacute-chronic (Fig. 4) . Depending on the stage, itching, redness, nodules, vesicles, edema, chemosis bulbi and scaling are prominent. Etiologically, cosmetics, mascara (additives, such as preservatives, dyes and fragrances, ointment bases), local therapeutics (eye drops, ointments) but also occupational allergens (vapors, dusts) are often in play. Also various allergens in metal or plastic eyeglass frames, such as nickel, plastic material (cellulose acetate, cellulose propionate, epoxy resin), additives (plasticizers, stabilizers, such as UV inhibitors [resorcinol monobenzoate, phenyl salicylate], wax polishes (turpentine, beeswax [Propolis](rosin, colophony), acrylics and solvents (ethylene acetate) can be the cause, so that a wide range of tests for contact allergens must be used for specific clarification by the dermatologist. (Fig. 5).

Fig. 3: Acute, weeping contact eczema of the eyelids
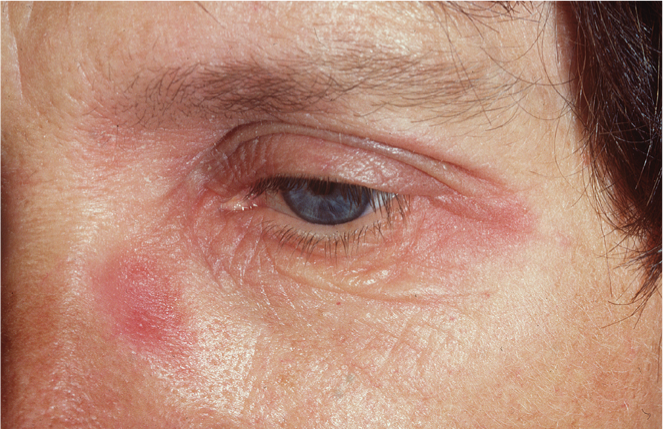
Fig. 4: Chronic contact dermatitis of the eyelids

Fig. 5: Contact eczema of the eyelids – Cause: eyeglass frame
Atopic eyelid eczema: Atopic eyelid eczema can occur in the context of disseminated atopic dermatitis (an atopic eczema) or in isolation. Itching, a livid redness of the upper and lower eyelids with palpable infiltration are clinically prominent. A typical feature of the neurodermitic constitution is the double fold of the lower eyelid (Dennie-Morgan) (Figs. 6 and 7) . Aetiologically, pollen (seasonal: neurodermatitis as pollinosis equivalent), house dust mites, animal epithelia and food can be determined as allergens anamnestically and by tests (prick tests, specific IgE determinations and especially Atopy patch tests with late reaction). Often, however, the allergological clarification remains negative: it is the “intrinsic” form of atopic eyelid eczema. Pathogenetically, this atopic manifestation is a combination of a type I (late-phase IgE-dependent immediate reaction) and a type IV reaction involving T lymphocytes and eosinophils. Topical weak corticosteroids (Ultracortenol® eye ointment) and the immunomodulators pimecrolimus (Elidel® 1%) or tacrolimus (Protopic® 0.03%) are used therapeutically. Black tea compresses are also of benefit, as well as wearing goggles for conjunctivitis, but these are often absent or very discreet, even with pollen etiology.

bb. 6: Atopic eczema of the eyelids with mild swelling of the eyelids.

Fig. 7: Atopic eyelid eczema during pollen season (neurodermatitis as pollinosis equivalent).
Allergic reactions of the conjunctiva
Conjunctivitis – immediate allergic reactions of the conjunctiva: Allergic conjunctivitis may occur seasonally, in the context of pollinosis, or parental. Clinical symptoms include itching, tearing, burning, and photophobia. Objectively, redness of the conjunctiva with vasodilatation (hyperemia), often chemosis bulbi, occasionally palpebral edema, or papillary reaction can be seen (Fig. 8).
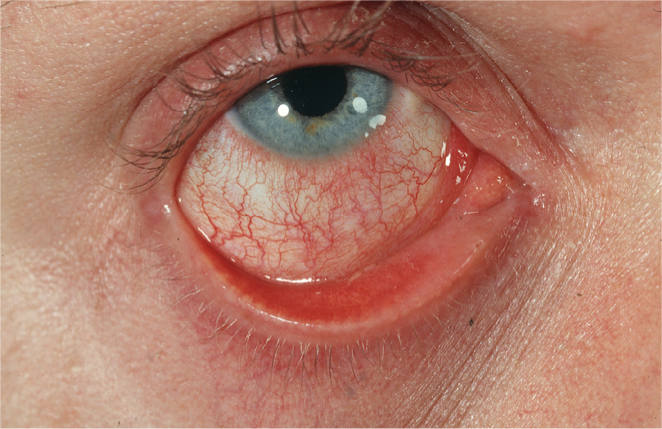
Fig. 8: Allergic conjunctivitis (here for pollen allergy).
Type I allergens that can be detected on prick testing are pollen (seasonal), dust mites, fungal spores, animal epithelia, food or occupational allergens (proteinaceous dusts, flours, spices, etc.) (Fig. 9).

Fig. 9: Occupational allergic conjunctivitis in allergy to a protein granule.
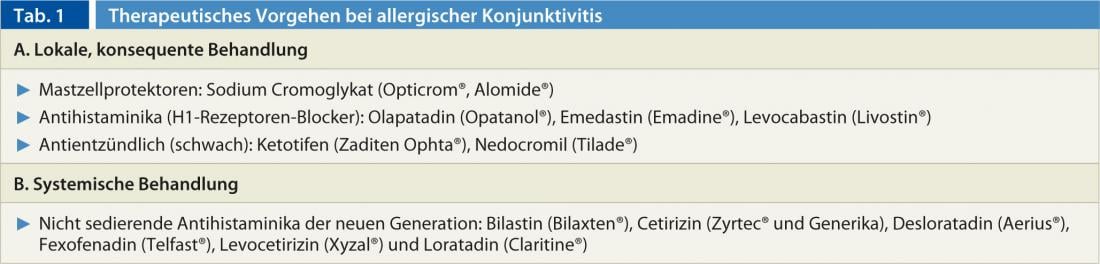
Therapeutic options include exposure prophylaxis (wearing of protective goggles or masks in case of occupational exposure, house dust clean-up, elimination of pets, etc.) and drug therapy, mostly topical, especially in isolated conjunctivitis, or with oral antihistamines(Tab. 1).
The “hay fever” conjunctivitis with its annually recurring symptoms carries the risk of a floor change to rhinoconjunctivitis, rhinitis and pollen asthma. In case of severe symptoms and at the stage of rhinoconjunctivitis, the implementation of hyposensitization treatment (specific immunotherapy, SIT), as the only causal therapy – must be considered in time. The success of SIT, both sublingual and subcutaneous, has been demonstrated by numerous double-blind, placebo-controlled studies over one to five years.
Conjunctivitis vernalis: Vernal (kerato)conjunctivitis is rarely seen in a general practice setting and is usually diagnosed and managed by the ophthalmologist. It occurs before puberty (around 11 to 13 years, rarely after 30), has a course of five to ten years, and then disappears spontaneously. The male sex is more frequently affected and manifests in spring to late summer, especially in warm climates. Complications may include keratitis punctata and corneal ulceration with subsequent scarring. The typical picture is represented by so-called “paving stones” on the tarsal conjunctiva. Atopy is common in family and personal history, and skin and blood tests (IgE) are not always positive for pollen. This is a local allergic event: Eosinophils and possibly allergen-specific IgE can be detected in the tear fluid. There is evidence also for a late-type (T-cell) response. The therapy is difficult, antihistamines are not very effective, mostly topical corticosteroids, possibly Tacrolimus (Protopic® 0,03%) have to be prescribed by the ophthalmologist.
Atopic keratoconjunctivitis: It occurs in patients with manifest, rather severe atopic dermatitis (neurodermatitis) and usually occurs between the ages of 18 and 50. The course is chronic over many years, as well in winter as in spring. Patients complain of itching, tearing, burning, and a watery to mucous white secretion. Complications may include limbal infiltration, scarring, and corneal scarring. Ophthalmologically, hyperemia of the conjunctiva, papillary hyperthropia, and, in complications, so-called Horner’s transtasis spots and corneal tension are noted (Fig. 10). Concomitant symptoms or further complications are chronic blepharitis, upper lid eczema, symblepharon, keratoconus, cataract (cataracta syndermatotica, Fig. 11), atopic uveitis, herpes simplex infection and even retinal detachment. It is imperative that care be provided in collaboration with an ophthalmologist and a dermatologist.
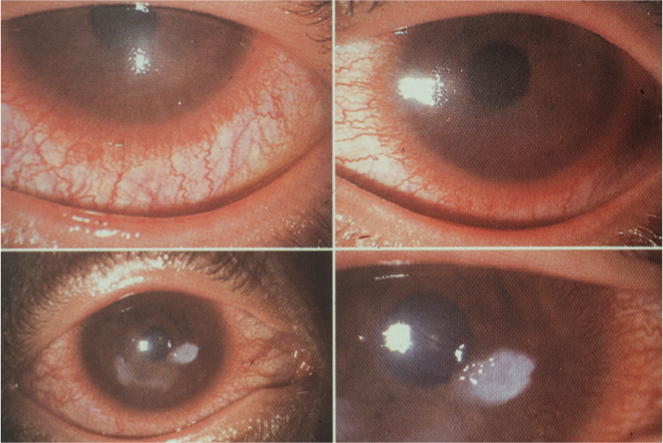
Fig. 10: Atopic keratoconjunctivitis
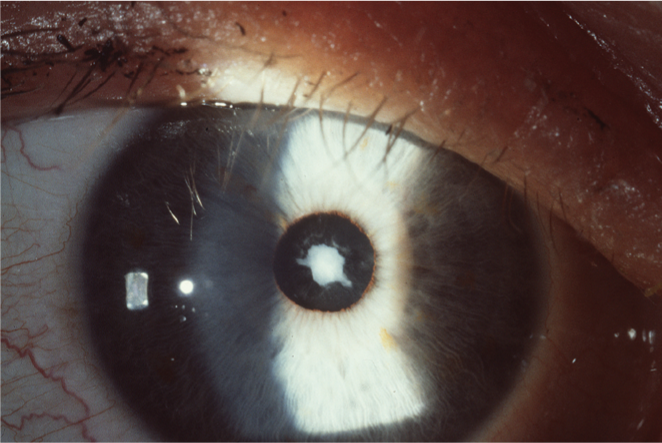
Fig. 11: Cataract (Cataracta syndermato-tica) in atopic keratoconjunctivitis.
Gigantopapillary conjunctivitis: This particular form of conjunctivitis is also diagnosed by the ophthalmologist. Clinically, affected individuals complain of itching, clear exudate, blurred vision, and foreign body sensation. Ophthalmologically, giant papillae of the tarsal conjunctiva, hyperemia, ciliary injection, and mucus are noted. Gigantopapillary conjunctivitis occurs in wearers of contact lenses, soft in 2%, hard in 5% of cases. It is a type IV allergy or intolerance reactions to lens material (polymers), irrigation fluid, eye drops or contaminants.
Contact allergic conjunctivitis: This conjunctivitis is triggered by contact allergens in the eye area, especially by local therapeutics and therefore pathogenetically corresponds to a type IV reaction of the conjunctiva. Differential diagnosis between type I or type IV allergic conjunctivitis can be difficult (Fig. 12) and often requires detective intuition and broad skin testing with type I and type IV allergens (Table 2).

Fig. 12: Difficult differential diagnosis between type I or type IV allergic conjunctivitis. Cause here thimerosal (merthiolate), an organic mercury compound, used as a preservative in many eye drops, lens cleaners, and vaccines

CONCLUSION FOR PRACTICE
- Diseases of the external eye can affect the eyelids or conjunctiva in isolation, with type I and type V allergies.
- In the eyelids, Quincke’s edema or atopic eyelid eczema (in neurodermatitis, but also isolated) may occur as an expression of an IgE-mediated immediate reaction.
- Allergic contact eczema of the eyelids and conjunctiva can be caused by cosmetics, mascara, eyeglass frame material, local therapeutic agents (active ingredients and additives, such as preservatives in eye drops and ointments), and occupational substances.
- Allergic eye diseases require clarification by an allergist, because only the elimination of the allergen brings freedom from symptoms. Prick tests and specific IgE determinations as well as so-called atopy patch tests and epicutaneous tests are used depending on the indication.
- Especially the clarification by means of epicutaneous samples often requires great experience after the search for the suspected substance.
- Conjunctivitis in pollen allergy is the most common form of allergic eye disease and usually the beginning of the atopic career (rhinitis, asthma). The indication for specific immunotherapy (SIT) must therefore be made at an early stage.
- In addition to the allergic conjunctivitis of immediate and late type, more severe clinical pictures of the conjunctiva can occur, such as the (kerato-)conjunctivitis vernalis – often very therapy-resistant in boys – the atopic keratoconjunctivitis in neurodermatitis (complication: cataract) and the gigantopapillary conjunctivitis as intolerance reaction in contact lens wearers. Their diagnosis and treatment must be done by the ophthalmologist, who will refer the patient to an allergist as needed.
Bibliography with the author











