Radiation therapy forms an integral component in the management of NSCLC. Recent advances in radiation therapy in NSCLC are based on both technical advances and the better understanding of the radiation biology of tolerances of normal tissues and the highest tolerable maximum tumor doses. Stereotactic body radiotherapy is now an acceptable treatment option for early stage peripherally situated NSCLC in patients unfit to undergo definitive surgery. Other recent strategies involve radiation dose escalation, use of PET-CT based treatment planning, isotoxic radiation therapy and use of particle beam radiotherapy.
Lung cancer is one of the commonest cancers reported globally. According to the GLOBOCAN 2012 [1], it is estimated that worldwide, an incidence of 16.7% makes lung cancer the commonest cancer in males and also contributes to the highest annual cancer related mortality of 34.2%. In females, the incidence is 8.8% with a mortality of 13.8%. The incidences of age standardized rate (ASR) for males and females were reported as 34.2 per 100,000 and 8.8 per 100,000 respectively. For both sexes combined, lung cancer was reported as the most fatal disease with the highest mortality of 19.4% of all malignancies.
In 2012, the National Institute of Cancer Epidemiology and Registration (NICER) reported that around 2500 and 1200 new cases are detected annually in males and females respectively in Switzerland [2]. Consequently, lung cancer represents the second and the third commonest cancer in males and females respectively in the country. During the period between 1995–1999 and 2005–2009, the percentage age standardized relative survival for men and women combined had shown an improvement for the 1st year following diagnosis from 37.8 to 44.5% and for the 5th year from 12.4 to 15.9%. The relative survival was found to be consistently better in women than men during both these calendar periods.
About 85–90% of all lung cancers are non-small cell lung cancers (NSCLC). Early diagnosis and improved therapeutic interventions through surgery, radiotherapy and chemotherapy, could have certainly attributed to the improved outcomes evident during this period. Surgery is still considered the primary modality for treatment of medically fit patients with operable early staged NSCLC. Chemotherapy has now a range of new chemotherapeutic agents and several promising targeted compounds. Radiation therapy, a key component in the management of these cancers has also undergone considerable technical improvements in the recent years. This article intends to present an overview of the various indications of radiotherapy in various stages of NSCLC and discuss the recent developments in the state-of-the-art in radiation therapy for NSCLC.
Radiation therapy options in NSCLC
The various radiation therapy options used in NSCLC are dependent on the stage of the disease, the patient’s general condition and the availability of specified radiation therapy facilities in a given institution. Thus, based on the NCCN, ESMO and DEGRO guidelines, radiation therapy in NSCLC could be broadly used as summarized (Fig. 1) [3–5]:
– Definitive or radical radiotherapy alone:
- a) With photons: 3D conformal radiotherapy (3D CRT), intensity modulated radiotherapy (IMRT) or volumetric modulated arc therapy (VMAT) supported by image guided radiotherapy (IGRT) and stereotactic body radiotherapy (SBRT). All these could be carried out with various respiratory gating techniques as may be available in a given center;
- b) Proton beam therapy
– Preoperative or postoperative radiotherapy: using the appropriate technique as stated above
– Radiotherapy in combination with chemotherapy: Concomitant chemoradiotherapy (CTRT) or sequential use of the two modalities
– Palliative radiotherapy with external beam radiotherapy or intraluminal brachytherapy.

The recent approaches in the radiation therapy for NSCLC involving treatment planning with respiratory gating, PET-CT based treatment planning, dose escalation with altered fractionation strategies, stereotactic body radiotherapy (SBRT), isotoxic radiation therapy approaches and use of particle beams – protons and carbons ions are summarized in the following sections.
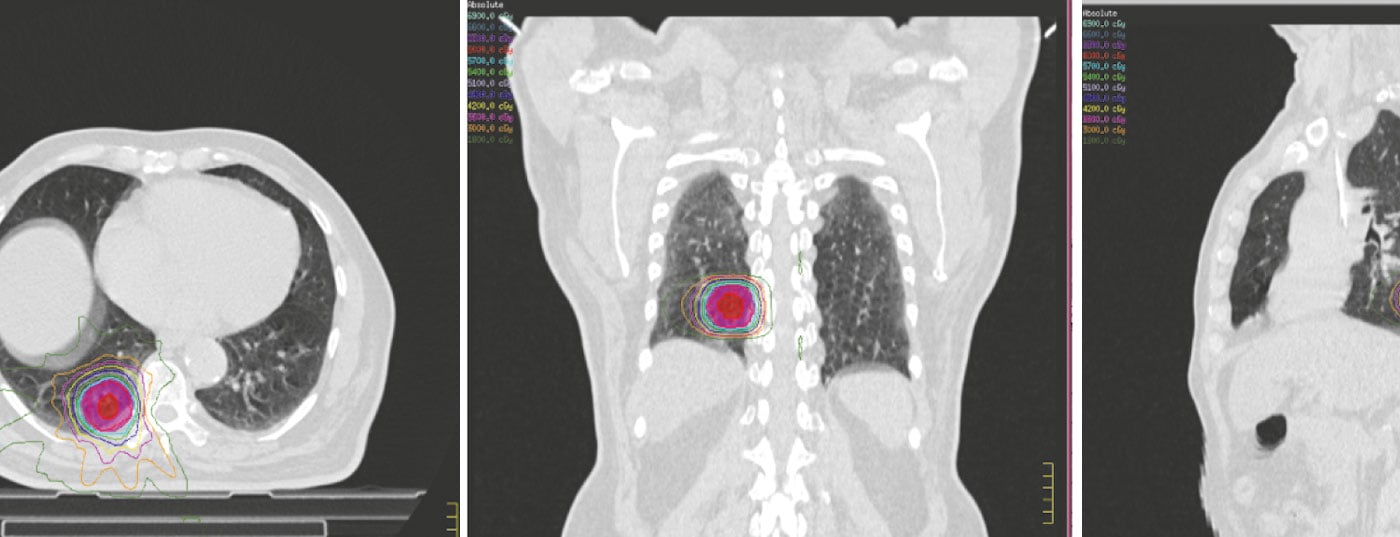
Treatment planning and respiratory gating
Most of the patients undergo a detailed evaluation at the various multidisciplinary tumor boards to outline the optimum treatment approach based on the tumor and patient characteristics. Once considered for radiation therapy, the patient undergoes a series of steps for radiation therapy planning aimed primarily to minimize the dose to the critical structures while delivering adequate doses to the tumor and the adjoining nodal stations (Fig. 2).
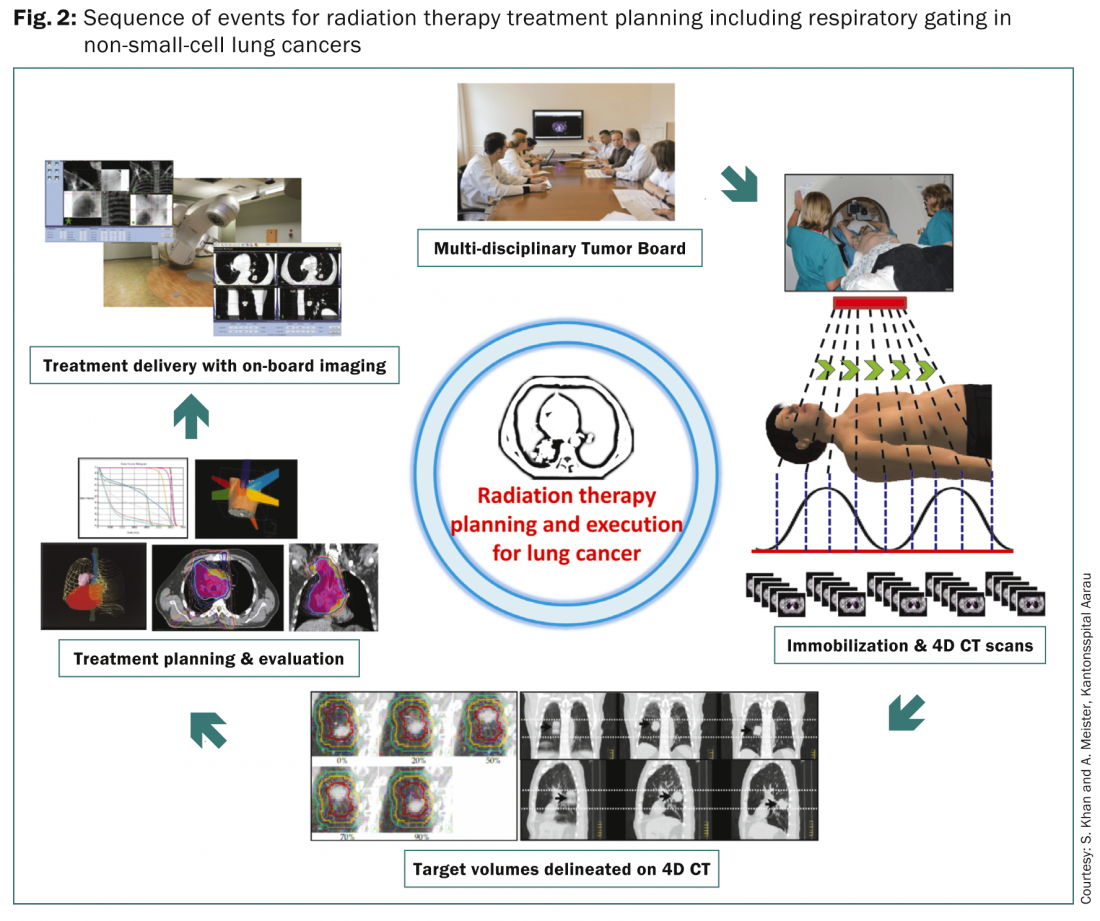
Since the lung tumors follow the respiratory movements, it is mandatory to take into account the respiratory movement and the resultant displacements of the primary lesion in lung. Several methods are presently available. These include free breathing or non-internal target volume (non-ITV) using standard CT simulation without 4D CT or fusion of inhalation or exhalation scans; breath-hold or gating non-ITV approach in which a single 3D CT image is acquired at a pre-determined respiration level; use of abdominal compressions during CT; 4D CT approach, which involves acquisition of at least two sets of 3D CT images at end-inhale or end-exhale and up to ten sets of 3D CT data sets corresponding to the various levels of respiration cycle. The 4D CT would be used to define the target volumes while a separate free-breathing CT is acquired for treatment planning and dose calculations. The resultant target volumes are usually defined as per the ICRU Reports 62 and 83 [6,7]. A detailed discussion on these is beyond the scope of this article and interested readers may refer to the ICRU reports 62 and 83 for a comprehensive review.
Once the target volumes and the organs at risks are delineated, the treatment planning is undertaken to optimize the combination of co-planar or non-coplanar beams with different weightages, angles, shapes and beam on-times, depending on the treatment technique to be used – 3D CRT, IMRT and VMAT. A defined radiation dose and the fractionation schedule are outlined with dose constraints specified for various organs at risk, especially lungs, spinal cord, esophagus, brachial plexus and heart. The various alternate treatment plans undergo a careful evaluation and the final plan is selected based on the assessment of the dose-volume histograms for the doses to the target volumes and various organs at risk. Treatment delivery is usually undertaken under careful supervision and carried out either as free-breathing, breath-hold or gating. All these would need on-board imaging to minimize the errors between treatment plans and their daily execution.
PET-CT based radiation treatment planning
FDG PET-CT is now one of the routinely used diagnostic modalities for staging purposes in NSCLC. It is also used for radiation treatment planning due to several advantages [8] (Fig. 3).
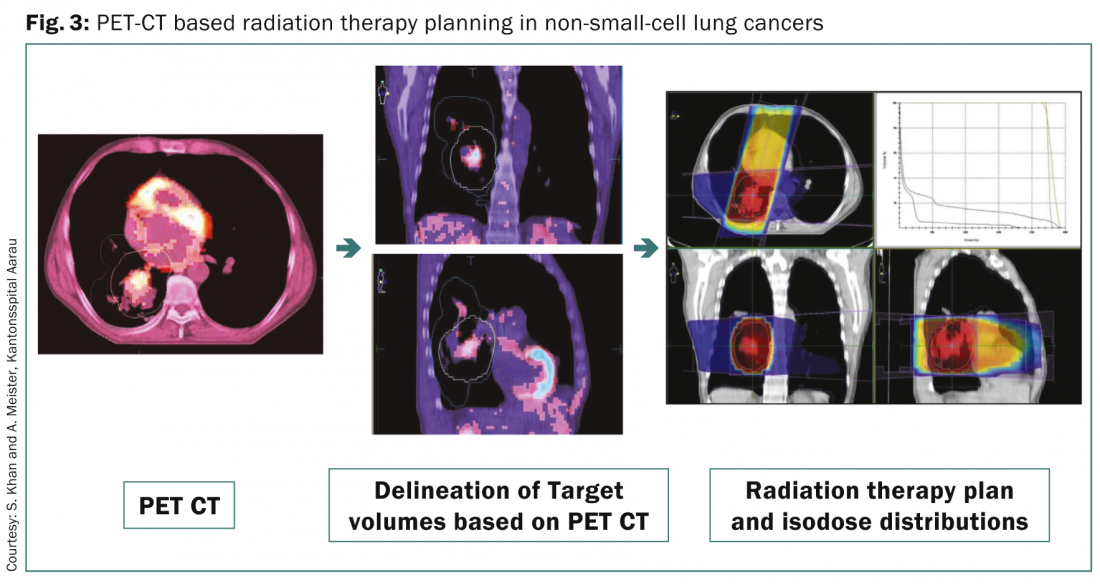
These include delineating the gross target volumes in a collapsed lung; assist in the identification of the involved regional lymph nodes for irradiation and planning of the CTV; detect any extrathoracic disease spread that may alter the disease stage and treatment plan for dose escalation to the gross disease based on the anato-metabolic images obtained through FDG-PET. 4D PET-CT has also been shown to be useful in accurate localization of patients with small tumors needing respiratory gated radiotherapy treatment and planning.
The clinical outcomes based on PET-CT based planning are quite promising and appear to have a low incidence of loco-regional recurrence. In a study of 137 patients, with stage III NSCLC, loco-regional recurrence was 14.6% for patients planned using PET-CT [9]. The results from a pilot study of 32 patients, reported only one patient each with regional failure and local tumor progression after PET-CT based concurrent chemoradiotherapy [10]. Presently, several groups in Europe and USA are exploring the use of FDG-PET for radiation therapy in NSCLC (ClinicalTrials.gov Identifier: NCT01024829 and 01507428). The application of PET-CT based planning could be further enlarged in future studies involving dose escalation to the primary tumors. This could be carried out with PET using hypoxic tracers, like F-MISO, 18F-FAZA or 18F-HX4 which can identify hypoxic radioresistant areas that could especially benefit from selective dose escalation [8].
Dose escalation and altered fractionations strategies
Dose escalation studies have been undertaken in a bid to improve the local control and had shown to improve the median survival from 20 to 26 month with doses escalated to 74 Gy in multiple phase I/II co-operative group studies along with concurrent chemoradiotherapy [11–13]. However, the recently reported results of the phase III trial, RTOG 0617 randomizing patients to 74 Gy in 37 fractions vs. standard 60 Gy in 30 fractions with weekly paclitaxel/carboplatin with or without cetuximab failed to show any benefit with 74 Gy [14]. Surprisingly, the local and loco-regional failures were worse in the higher dose arm, although the toxicities between the two groups were comparable. The possible reasons of this could be an increased cardiac dose and the extended overall treatment time in the high-dose arm. The final report and the possible reasons for the lack of improvement with higher doses are being investigated.
Altered fractionation schedules using hyperfractionation (e.g. CHART: 54 Gy in three daily fractions of 1.5 Gy during twelve continuous days) have also been explored in NSCLC and randomized trials have shown a benefit in survival outcomes over conventional fractionations schedules [15–17]. The regime however is logistically difficult to deliver even though they promise to improve the survival outcomes.
With the availability of PET-CT based treatment planning and state-of-the art radiotherapy treatment techniques, hypofractionated radiation schedules with delivery of doses greater than the standard 2 Gy per fraction are being currently explored and have shown promise for early stage tumors resulting in a median survival of 38.5 months [18]. These have led to their use in stereotactic body radiotherapy in early NSCLC, especially in patients medically unfit for surgery.
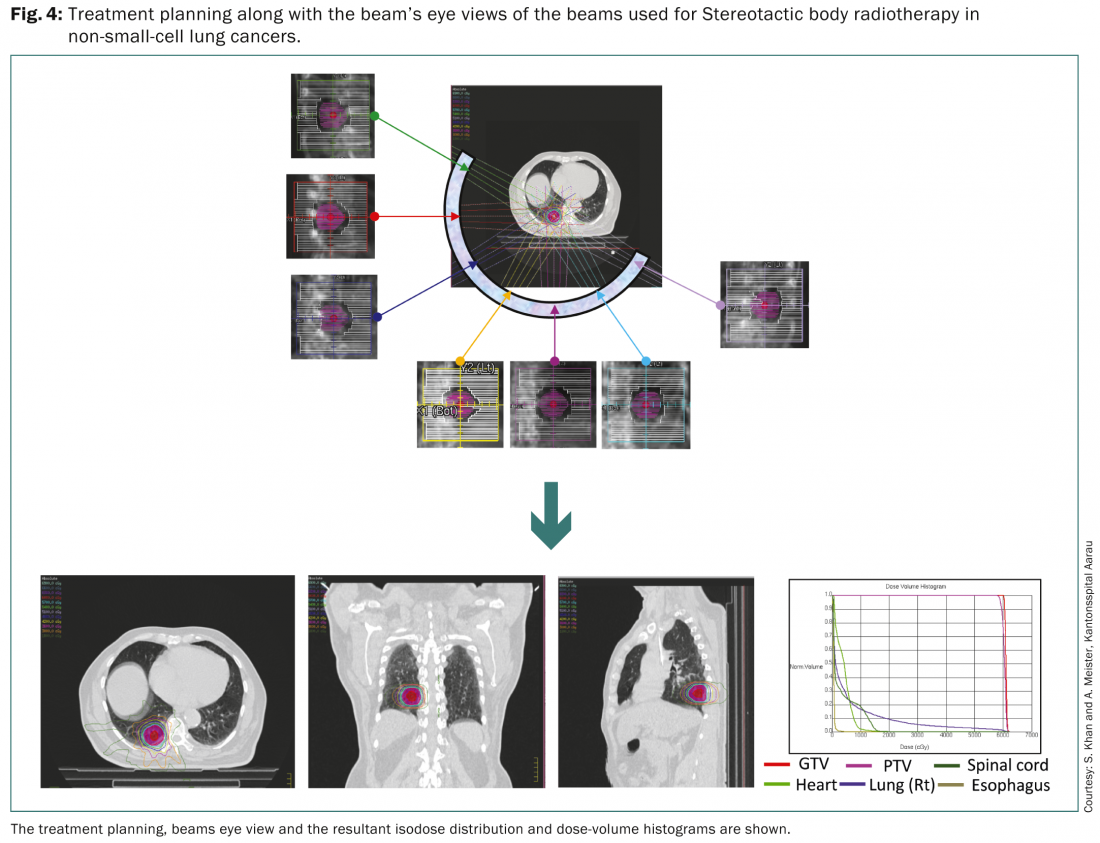
Stereotactic Body Radiotherapy (SBRT)
SBRT permits delivery of a high radiation dose to small tumor volumes with precision and allows the practice of a hyperfractionated high-dose radiation therapy. As per the European Organisation for Research and Treatment of Cancer (EORTC), SBRT is a suitable approach for patients with node negative, peripheral lesions less than 6 cm and could be used for elderly patients who are not fit for surgery [19]. It could also be applied to patients who had undergone a prior pneumonectomy. Respiratory gating along with treatment planning based on FDG PET-CT is recommended for delineation of the different target volumes.
A systematic review reported by Soldà et al. compared the outcomes with a surgical cohort from a series of 45 reports compromising 3771 patients [20]. A wide range of dose fractionations schemes were reported. These ranged from 30 Gy in a single fraction to 45–72.5 Gy in three to ten fractions. The 2-year survival for 3201 patients with stage I NSCLC with SBRT was 70% with a 2-year local control of 91%. This compared well with 2-year survival of 68% in 2038 patients of stage I treated with surgery. There was no difference in survival or local progression free survival amongst patients treated with different radiotherapy techniques used for SBRT.
A recent meta-analysis just reported, was carried out in 4850 patients from 40 SBRT studies and compared with the surgical outcomes from 23 studies comprising of 7071 patients in stage I NSCLC [21]. The mean age of patients on SBRT was lower than those in the surgical series at 74 and 66 years, respectively. On adjusting for proportion of operable patients and age, the overall survival, disease free survival and local control did not significantly differ between SBRT and surgery. The authors concluded that surgical approaches remained the current standard of care for medically operable patients, but those who are medically unfit or may refuse surgery, SBRT should be offered as a standard of care due to its proven effectiveness and low toxicity.
SBRT is usually advocated for peripheral tumors and its use in centrally located tumors is still uncertain due to an anticipated higher risk of toxicity. The outcomes of SBRT in 90 patients with central (50%) and peripheral (56%) located stage I NSCLC have been reported from a combined database of 13 German and Austrian academic radiotherapy centers [22]. Peripheral tumors had received a higher biologically effective dose (BED10) (72 Gy for central vs. 84 Gy for peripheral tumors). The 3-year actuarial overall survival was 29% for central compared to 51% in peripheral tumors (p<0.001), while the corresponding freedom for local progression was 52% and 84% respectively (p<0.001). No significant differences in the treatment related toxicities were reported. These results although indicate that central tumors could be treated with SBRT, but its outcomes are perhaps limited by a reduced dose in central tumors.
Thus, SBRT for lung cancer is a viable treatment approach for peripheral tumors up to 6 cm and could be considered as an alternative to patients who are otherwise medically unfit for surgery [3–5]. A BED of >100Gy, prescribed at the encompassing isodose is usually desirable to achieve the optimal results.
Isotoxic or personalized radiotherapy
Isotoxic or personalized radiotherapy involves administration of radiation doses based on the individual patient’s normal tissue constraints. The present practice of radiation therapy involves individually shaped radiation beams conformed to the tumor dimensions in each individual patient, paving a step towards individualized radiation treatment planning. However, the individualized treatment could also be extended to include the highest tolerable total tumor dose (TTD) that could be delivered and tolerated in a given patient respecting the normal tissue constraints. Baardwijk et al. hypothesized that the best achievable radiation schedule would include the highest TTD based on individualized normal tissue dose constraints delivered in an overall treatment time of less than five weeks [23]. They were able to demonstrate its feasibility and delivered a mean tumor dose of 63 Gy (range 46.8–79.2 Gy) in medically inoperable patients with locally advanced NSCLC with acceptable acute and late tissue toxicity. They achieved a complete metabolic response in 44% patients with 1-year overall survival of 57.1%. Several ongoing trials are currently underway at several centers of UK and Europe.
Reymen et al. recently reported the outcomes in stages T4N0-1 and single nodal station IIIA-N2 of individualized isotoxic accelerated radiotherapy (INDAR) and chemotherapy in NSCLC [24]. 83 patients were treated with a median dose of 65 Gy (43.5–72 Gy) in a median overall treatment time of 30 days (17–48 days). The treatment consisted of 30 fractions of 1.5 Gy twice daily followed by 2 Gy per fraction up to a maximal TTD limited by normal tissue constraints. 52 patients received concurrent while 31 were treated with sequential chemotherapy along with INDAR. The overall survivals for T4N0-1 at 2- and 5-years were 55 and 25% respectively while the corresponding survivals for IIIA-N2 were 53 and 24% respectively. The most severe side effect observed was grade 3 esophagitis in seven patients, but they were all resolved with conservative treatment.
These results indicate that the isotoxic radiotherapy with individualized dose prescriptions could further improve the outcomes of these locally advanced inoperable tumors and achieve long-term survival with low morbidity. Further dose escalation with improved radiation therapy planning and delivery, novel chemotherapy drugs or biologically targeted agents or even a combination with surgery could be certainly explored in future isotoxic radiotherapy trials.
Particle beam therapy – proton and carbon beam therapy
The characteristic Bragg peak (low dose at entrance of the beam and a rapid fall off at maximal dose deposition) provides a unique dosimetric advantage of protons and carbon beams over the photons [25]. Radiobiologically, although photons are believed to be nearly similar to protons, the high linear energy transfer properties of carbon-ions confer a radiobiological advantage of carbon-ions over both proton and photons. Thus, theoretically the proton and carbon-ion dose distributions could be more conformal to the target volumes with lesser integral doses compared to photon based radiation therapy.
A number of phase I/II studies with particle beams have been found to be safe and efficacious in stage I NSCLC. A meta-analysis conducted by Grutters et al. has looked at the comparative effectiveness of protons, photons and carbons [26]. The corrected 2-year overall survival was 53% for conventional photon radiotherapy, 70% for SBRT, 61% for protons and 74% for carbon. At 5-year, the overall survivals for conventional radiotherapy (20%) were significantly lower than that of SBRT (42%), proton (40%) and carbon-ion therapy (42%). Thus, it appears that although the results with particle therapies are better than the conventional photon beam, they are still comparable with those of SBRT. It is believed that particle therapy could perhaps be more beneficial in stage III NSCLC, where the 2-year overall survival drops to a mere 26–36% with conventional chemoradiotherapy [26].
A recent report from Chang et al. highlighted the capability of intensity modulated proton therapy (IMPT) to be feasible along with 4D CT based respiratory motion management for NSCLC. In a pilot study involving 34 consecutive patients, IMPT with respiratory gating was found to produce significant reduction in all the dosimetric parameters under consideration than the standard IMRT [27].
With a spurge of proton beam facilities, the introduction of intensity modulated proton beam therapy (IMPT) and on-board volume image guidance, results with proton therapy could be expected to improve, though this needs to be confirmed through randomized trials with SBRT.
Conclusions
NSCLC continues to impose a challenge for the treating oncologists to integrate the best possible options of a combination of surgery, radiotherapy and chemotherapy. Even with the latest developments in each of these modalities, both local control and overall survivals continue to be of concern to the treating oncologists.
The present technological developments in radiation therapy, along with the understanding of the radiobiological implications of the various dose-fractionations schemes, have certainly enabled a safer and a more precise delivery of radiation therapy. This has opened up the various options like SBRT, isotoxic radiotherapy, particle beam etc. as a possible alternative for a select group of patients. However, the integration with other modalities like chemotherapy agents and the newly developed molecular targeted therapies needs further investigation based on both evidence and personalized medicine to produce the desired outcomes.
Prof. Dr. med. Niloy Ranjan Datta
Dr. med. Silvia Gómez Ordóñez
Prof. Dr. med. Stephan Bodis
Literatur:
- Ferlay J, et al.: GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available at: http://globocan.iarc.fr.
- Bordoni A, et al.: Trends in lung cancer survival in Switzerland. Schweizer Krebsbulletin 2012; 3. Available at: www.nicer.org/assets/files/skb_3-2012_nicer_lung_cancer_survival_in_ch.pdf.
- Vansteenkiste J, et al.: Annl Oncol 2013; 24(suppl 6): vi89–vi98.
- NCCN Clinical practice guidelines in Oncology: Non-small cell lung cancer, version 4. 2014. Available at: www.nccn.org/professionals/physician_gls/pdf/nscl.pdf.
- German Society for Radiation Oncology (DEGRO): Guidelines for extracranial stereotactic radiotherapy. Available at: www.degro.org/dav/html/download/pdf/ESRT_Leitlinie.pdf.
- International Commission on Radiation Units and Measurements: Prescribing, Recording and Reporting Photon Beam Therapy (Supplement to ICRU Report 50), ICRU Report 62, Bethesda, MD, 1999.
- International Commission on Radiation Units and Measurements: Prescribing, Recording and Reporting Photon Beam Intensity Modulated Radiation Therapy, ICRU Report 83, Bethesda, MD, 2010.
- Chi A, Nguyen NP: Front Oncol 2014 Oct 7; 4: 273.
- van Baardwijk A, et al.: Eur J Cancer 2012; 48: 2339–2346.
- Fleckenstein J, et al.: Int J Radiat Oncol Biol Phys 2011; 81: e282–289.
- Bradley JD, et al.: Int J Radiat Oncol Biol Phys 2010; 77: 367–372.
- Schild SE, et al.: Int J Radiat Oncol Biol Phys 2006; 65: 1106–1111.
- Sociniski MA, et al.: J Clin Oncol 2008; 26: 2457–2463.
- Bradley J, et al.: J Clin Oncol 2013; 31(15): 7501.
- Belani CP, et al.: J Clin Oncol 2005; 23: 3760–3767.
- Hatton M, et al.: Int J Radiat Oncol Biol Phys 2011; 81: 712–718.
- Saunders M, et al.: Lancet 1977; 350: 161–165.
- Bogart JA, et al.: J Clin Oncol 2010; 28: 202–206.
- Ruysscher DD, et al.: J Clin Oncol 2010; 28: 5301–5310.
- Soldà F, et al.: Radiother Oncol 2013; 109: 1–7.
- Zheng X, et al.: Int J Radiat Oncol Biol Phys 2014; 90: 603–611.
- Schanne DH, et al.: Strahlenther Onkol 2014, doi: 10.1007/s00066-014-0739-5.
- van Baardwijk A, et al.: Int J Radiat Oncol Biol Phys 2008; 71: 1394–1401.
- Reymen B, et al.: Radiother Oncol 2014; 110: 482–487.
- Grant JD, Chang JY: Biomed Res Int 2014: 389048. doi: 10.1155/2014/389048.
- Grutters JPC, et al.: Radiother Oncol 2010; 95: 32–40.
- Chang JY, et al.: Int J Radiat Oncol Biol Phys 2014; 90: 809–818.
InFo ONKOLOGIE & HÄMATOLOGIE 2015; 3(1): 6–12