If there is a narrowing of one or more coronary arteries, it is called coronary stenosis. The cause is usually atherosclerosis in coronary heart disease. But what to do when complex coronary stenosis is detected? What interventional measures does treatment management currently provide? These and other questions were addressed by Prof. Dr. med. Holger Nef, Giessen (D), in his lecture at the Academy Forum.
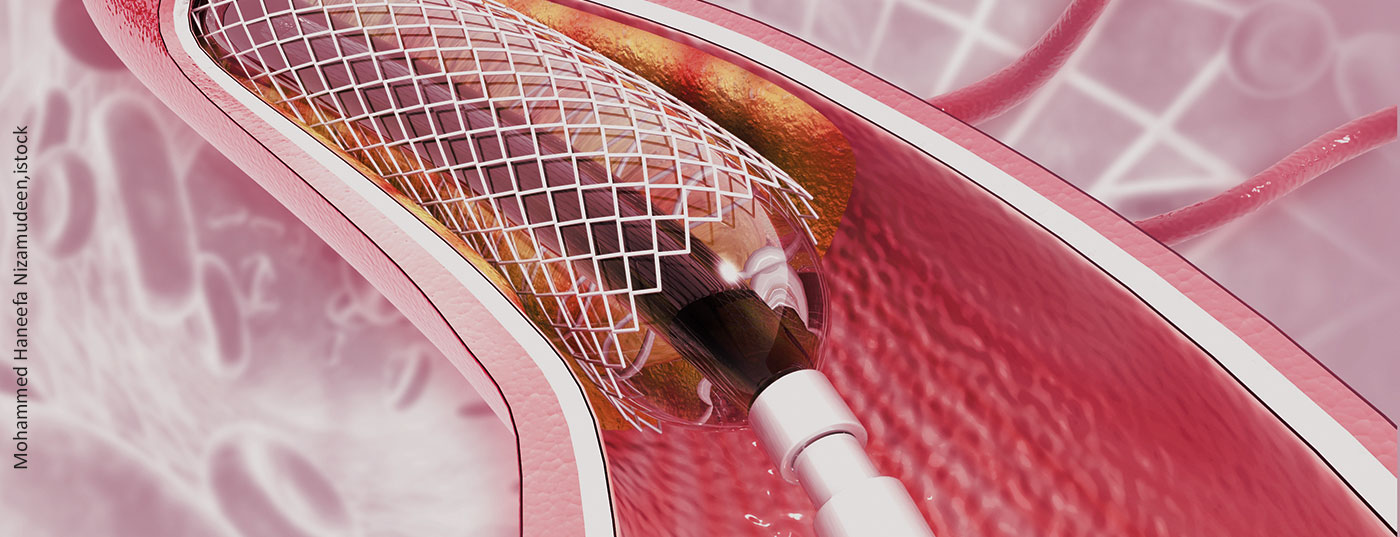
When is coronary stenosis to be defined as complex? In Europe, this is when at least three stents have been implanted, three lesions have been treated, a bifurcation with two stents has been performed, or the stent length measures greater than 60 mm. In this context, the main stem may well be counted as a complex lesion under certain circumstances, and calcification should also be considered, the expert said. In a registry work, it was demonstrated that the presence of a complex situation does correlate with clinical outcome. TLF, TLR, TVR, and MACE rates were significantly higher in patients with complex coronary stenoses than in patients without complex events. As a recent study shows, in practice it can be assumed that about half of all patients have complex lesions.
Regardless of whether a complex lesion is present with respect to the bifurcation, main stem, or calcified lesion, a radial approach should always be used whenever possible. Although the distal puncture is a little more difficult to apply due to the angle at the beginning, the sequence thereafter is just as safe and stable as an approach from the femoral side. However, in terms of all-cause mortality and bleeding rates, the radial approach is preferable to the femoral approach, as demonstrated by meta-analyses. The distal radial approach is currently experiencing a real hype. This is due to significantly lower occlusion rates, Nef reported.
Which approach is required?
What makes a bifurcation complex? According to the Medina classification, both main branch and side branch must be affected. According to the DEFINITION criteria, a complex bifurcation is present if the side branch has >90% diameter stenosis and >10 mm lesion length and two minor criteria are added. These include:
- More than just mild calcification
- Multiple lesions
- Bifurcation angle <45° and >70°
- MB-RVD <2.5 mm
- MB Lesion length >25 mm
- Thrombus.
This entails a two-stent strategy, he said. This includes culotte and DK crush as indispensable craft. Meanwhile, a DK can also be added to the culotte. Compared with one culotte, this procedure has the advantage of reducing the duration of the intervention and, in addition, DK-Culotte has the fewest apositioned stents. The two-stent strategy should be given preference over a single-stent strategy because it has significant advantages with regard to target vessel myocardial infarction, target lesion revascularization, and target lesion failure.
Imaging is an essential point in the complex lesion and is part of the interventional standard, as recent data regarding mortality rates show. It is also needed to detect the quality of the intervention. After all, what makes a good PCI – especially in calcified lesions? It is characterized by good deployment of the stent and the most adequate minimal stent area (MSA) >5.5 mm2 (IVUS) or 4.5 mm2 (OCT). Malappositions, dissections, and tissue progression should be avoided. However, calcium often cannot be visualized on imaging, which complicates the procedure. Very recent data have compared rotablation with lithotripsy. Non-inferiority of lithotripsy was observed, with significantly shorter procedure times and less contrast agent administration. Accordingly, this process could be a valuable addition in the future.
Source: Interventional Cardiology Update. Complex coronary stenoses – What is the current interventional therapy standard? Academy Forum, 20.04.2022, 13:30-15:00
Congress: 88th Annual Meeting of the German Society of Cardiology (DGK)
CARDIOVASC 2022; 21(2): 17 (published 6/25/22, ahead of print).