One of the workshops at the annual meeting of the Swiss Society of Cardiology on June 12, 2014, examined the role of diet in cardiovascular disease. How do alcohol, omega-3 fatty acids or red meat affect cardiovascular risk, and what are the benefits of the Mediterranean diet?
(ee) Is there evidence for the benefit of a Mediterranean diet (MD) in the secondary prevention of cardiovascular diseases? Yes, said the speaker Prof. Dr. med. Hans Rickli, Kantonsspital St. Gallen, there are several corresponding studies. One example is the meta-analysis by Schwingshackl et al. which showed that high adherence to a Mediterranean diet is associated with a reduction in hs-CRP and IL-6 and an improvement in endothelial dysfunction [1].
The Lyon Heart Study (1999) was stopped early because significantly fewer myocardial infarctions occurred in study participants with MD – in contrast to a normal “Western Diet” [2]. Today, the effect of this study would probably be smaller because risk factors such as hypercholesterolemia or hypertension are better managed. However, if a diet in accordance with the food pyramid is consistently followed and those affected also take sufficient exercise, then it has a preventive effect (reduced cardiovascular risk 9% plus reduction in the risk of cancer and Alzheimer’s disease). However, it is problematic that secondary prevention approaches such as weight loss, diet, and smoking cessation are not popular among patients.
In primary prevention, the situation is less clear. A 2013 study compared three diets in individuals at high cardiovascular risk: low-fat, Mediterranean with additional nuts (walnuts, almonds, and hazelnuts, at least 30 g/d), and Mediterranean with additional extra virgin olive oil (at least 4 tablespoons/d), which is rich in polyphenols (Table 1 ) [3].
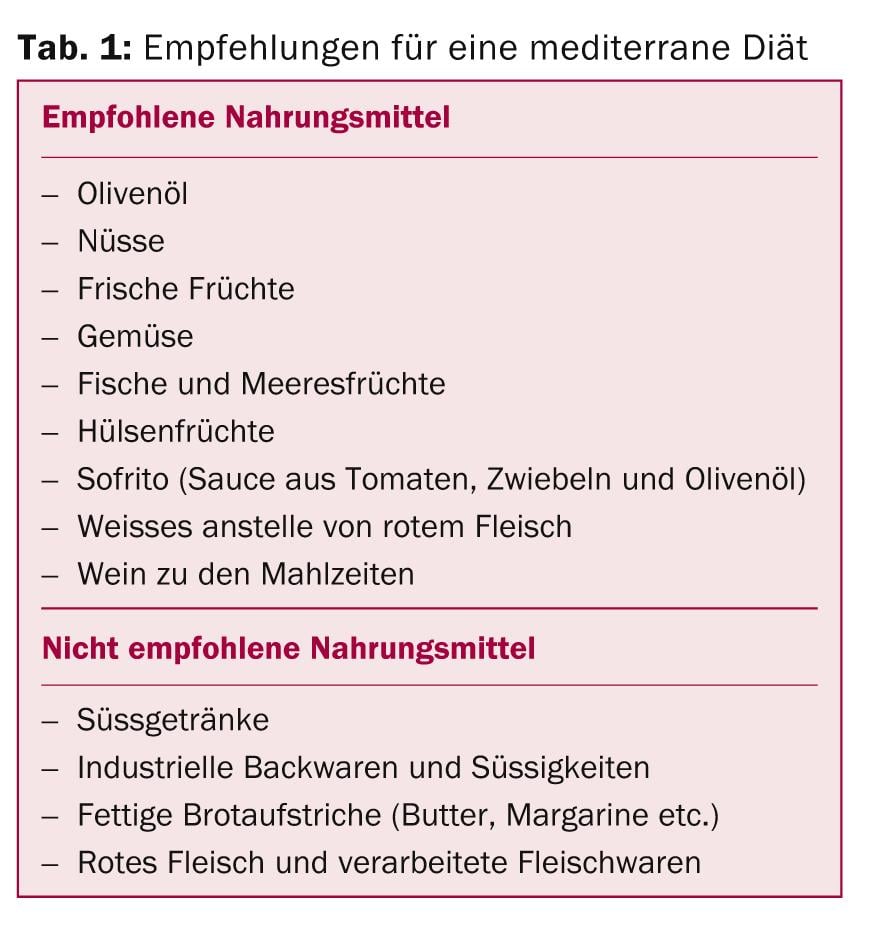
The study participants ate this way for about five years. Both Mediterranean diets performed better than the low-fat diet in terms of cardiovascular risk reduction, but the number needed to treat (NNT) was relatively high at 300. Above all, the number of cerebral strokes was reduced, but not the number of heart attacks. “The Mediterranean diet is one of many factors that can inhibit the early development of atherosclerosis,” the speaker said.
Fish and omega-3 fatty acids
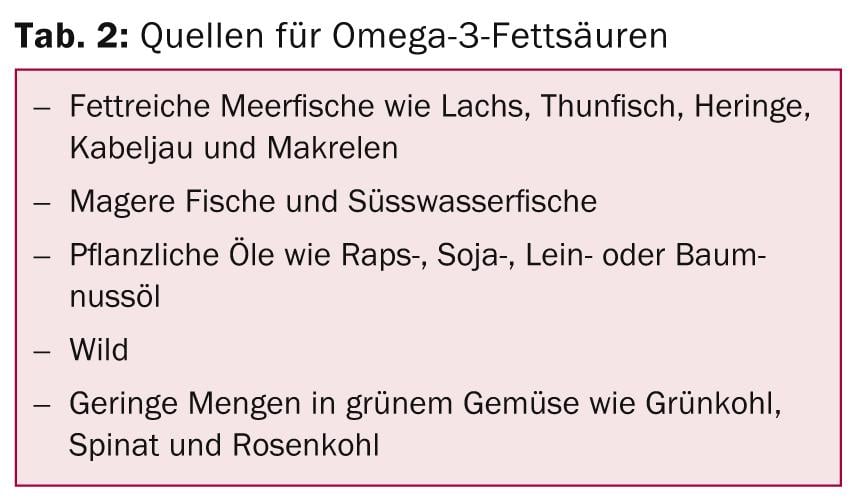
Prof. Dr. med. Hansjürg Beer, Kantonsspital Baden, presented the effects of omega-3 fatty acids on cardiovascular risk. As early as 1979, a study by Dyerberg and Bang showed that platelet aggregation was reduced and bleeding time was significantly longer in Inuit compared with control subjects from Denmark [4]. High consumption of omega-3 polyunsaturated fatty acids inhibits thrombus formation, platelet activation, and platelet adhesion. Alpha-linolenic acid (ALA) also reduces T-cell mediated inflammation. A high intake of ALA also showed a cardioprotective effect in the Nurses Health Study. In a 2012 meta-analysis, it was found that for every gram of ALA that you take more, the relative risk of cardiovascular death decreases by 10%.
A reduction in cardiovascular events also results from fish consumption of once to twice per week. Whether supplements also work is currently controversial. In the GISSI trial, in which participants took 1 g of omega-3 fatty acids per day for three years for secondary prevention, the main reduction was in rhythmogenic deaths. Fish oil substitution in diabetics showed no effect. Currently, there is no established evidence for the efficacy of supplements, but more and better-powered studies are needed. In the USA and Europe, different recommendations apply as to how many omega-3 fatty acids one should consume: In the USA, two fish meals per week are recommended for primary prevention, which is an environmental problem in view of the overfishing of the oceans; in Europe, it is recommended to cover 1% of the energy requirement with ALA (Tab. 2).
How dangerous is red meat?
Prof. Dr. Sabine Rohrmann, Institute for Social and Preventive Medicine, Zurich, provided information on current knowledge regarding meat consumption and cardiovascular risk. In Switzerland, only data on meat sales exist, but not on direct consumption. The most meat per capita was eaten in 1985 (about 70 kg per year), today it is about 60 kg per capita per year. Why high meat consumption is unfavorable in terms of disease risk is not completely clear. One problem is certainly the relatively high fat content of meat (especially in processed products such as sausage) with 30-50% saturated fatty acids. However, there are big differences between individual meat products, the speaker emphasized: “If a cow grazes on the alp, its meat has a different fatty acid composition than the meat of a cow that primarily stands in the barn and gets soybean meal.” The salt content in meat products is also often high.
Various studies show associations between the consumption of red meat or Meat products and cardiovascular mortality. Asian studies are an exception, which is probably due to the fact that less meat is consumed in Asia than here and Asian meat eaters also have a healthier lifestyle. The risk of ischemic stroke is significantly increased with high consumption of unprocessed and processed red meat. As a preventive measure, the salt content of meat products can be reduced: 10-20% of the salt can be omitted without changing the taste of the products.
But there are still many unanswered questions: Is it better to consume white meat? What are the interactions between meat and other food groups? For example, are the effects of meat consumption lower for fruit eaters than for people who hardly eat any fruit?
Alcohol and Cardiovascular Risk: Whether Beer or Liquor Doesn’t Matter
“There are very few intervention studies on the topic of alcohol and cardiovascular events,” explained Prof. David Conen, MD, University Hospital Basel. This is because, on the one hand, study participants do not want to give up alcoholic beverages, and on the other hand, non-drinkers cannot be encouraged to consume alcohol for ethical reasons. Therefore, existing knowledge is predominantly based on epidemiological data.
With regard to heart attacks, the more alcohol someone drinks, the lower their risk of heart attack. However, one should not draw the wrong conclusions from this, because abstinence is often an indicator of poor health, there are quite a few ex-alcoholics among teetotalers, and people who drink a lot have a high risk of dying from cirrhosis of the liver or an accident – even before they can have a heart attack. Those who consume a lot of alcohol but otherwise live a healthy life (sufficient exercise, healthy diet, normal BMI, etc.) have a low risk of heart attack. In the case of stroke, the situation is different: The risk of stroke increases exponentially from a consumption of about 60 g per day. Two possible explanations are increased blood pressure with alcohol consumption and clustered atrial fibrillation.
Whether one consumes alcohol in the form of beer, wine, or liquor probably has no effect on cardiovascular risk. This is shown by studies from the USA, Ireland (with beer) and France (with wine). The type of drinking, on the other hand, probably plays a role. There is evidence that binge drinking (consuming large amounts of alcohol at irregular intervals) carries a higher risk of cardiovascular disease. However, it is difficult to find participants for corresponding studies, because binge drinkers often drink (too) much in general. One explanation for the increased risk associated with binge drinking is the so-called “holiday heart”: patients often arrive at the emergency department drunk and with atrial fibrillation (AF) during the holidays. Whether there is a “quantity threshold” above which VHF becomes clustered (women >2 drinks/d, men >3-4) is controversial.
Supplements bring nothing
Prof. Dr. med. Paolo Suter, University Hospital Zurich, gave a very engaging lecture on the topic of “Nutraceuticals”. Nutraceuticals are concentrated, biologically active substances derived from food in a capsule (for example polyphenols) – so theoretically cherry stems also belong to them. There is no evidence that these products have an effect on morbidity and mortality, Linus Pauling already found that out about 50 years ago. Most studies conducted later are methodologically inadequate and do not show positive outcomes with respect to hard endpoints.
Virtually every nutrient has a huge number of studies associating the nutrient with virtually every possible outcome. “But an association does not necessarily imply causality,” Suter said. “In the past, fish heads were thrown away, but today they are processed into nutraceuticals, for example, to isolate taurine or chondroitin.” Nutrition should not be separated from exercise and other lifestyle factors, such as smoking. Various studies have shown that supplement users fall prey to the misconception that they can eat and smoke a lot and neglect exercise.
FODMAPs – an excursion into gastroenterology
At the end of the workshop, Prof. Michael Fried, MD, Director of the Clinic for Gastroenterology and Hepatology at the University Hospital Zurich, spoke on the topic of FODMAPs. This abbreviation stands for “fermentable oligo-, di- and monosaccharides and polyols”, i.e. carbohydrates and polyhydric alcohols (lactose, fructose, fructans, galactans, sorbitol, mannitol, xylitol, etc.) found in many foods. FODMAPs are cardiovascularly healthy but are not well absorbed in the gut. In patients with irritable bowel syndrome (IBS), the most common gastrointestinal disease, they cause symptoms such as bloating and abdominal pain. Particularly problematic is fructose, which is now present in many foods, and lactose, which is often not tolerated by IBS patients. A study in which IBS patients were treated with a low-FODMAP diet showed significant improvement in IBS symptoms [6].
Source: Annual Meeting of the Swiss Society of Cardiology and the Swiss Society of Cardiothoracic Surgery, Workshop 9, June 12, 2014, Interlaken.
Literature:
- Schwingshackl L, Hoffmann G: Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis 2014 Apr. pii: S0939-4753(14)00109-4. doi: 10.1016/j.numecd.2014.03.003. [Epub ahead of print].
- Leaf A: Dietary prevention of coronary heart disease: the Lyon Diet Heart Study. Circulation 1999 Feb 16; 99(6): 733-735.
- Estruch R, et al: Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013 Apr 4; 368(14): 1279-1290. doi: 10.1056/NEJMoa1200303.
- Dyerberg J, Bang HO: Haemostatic function and platelet polyunsaturated fatty acids in Eskimos. Lancet 1979 Sep 1; 2(8140): 433-435.
- GISSI Investigators: Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 1999. 354(9177): 447-455. doi:10.1016/S0140-6736(99)07072-5.
- Halmos E, et al: A Diet Low in FODMAPs Reduces Symptoms of Irritable Bowel Syndrome. Gastroenterology 2014 Jan; 146: 67-75. http://dx.doi.org/10.1053/j.gastro.2013.09.046
CARDIOVASC 2014; 13(4): 32-34











