Whether or not hypertension after apoplexy needs to be treated depends on a variety of factors. First, penumbra is dependent on systolic blood pressure, but a 10 mmHg increase in values above 180 mmHg increases the likelihood of poor outcome by approximately 25%. So what to do?
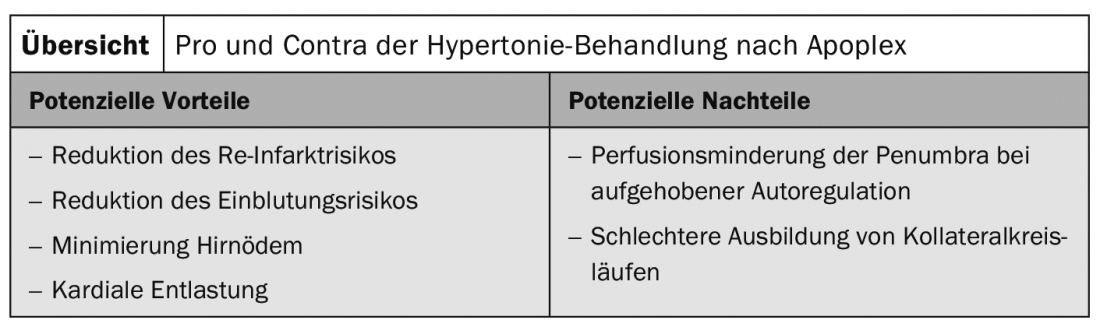
In acute stroke, 75% of patients suffer from elevated blood pressure. This may be due to stress from the event, a full bladder, nausea, vomiting, pain, and/or a physiological response to cerebral hypoxia, explained Prof. Andreas Luft, MD, Zurich. The question is whether the high blood pressure should be treated or not. On the one hand, reduction of the risk of re-infarction and hemorrhage, minimization of cerebral edema, and cardiac unloading argue in favor. But on the other hand, low blood pressure is also associated with poor outcome. Different studies have addressed this issue. Prof. Luft concluded that a cautious reduction by a maximum of 15-25% within 24 hours with the aid of short-acting intravenous antihypertensives is a suitable approach. This should be done under close monitoring, including arterial blood pressure measurement. Only in cases of hemorrhage should more intensive lowering to systolic <140 mmHg be attempted.
Source: Zurich Hypertension Day
Literature:
- Willmot, et al: Hypertension 2004.
- Castilio, et al: Stroke 2004.
- AHA Guidelines 2008
- Enames, et al: JNNP 2002.
CARDIOVASC 2019; 18(2): 31











